Tony West
advertisement
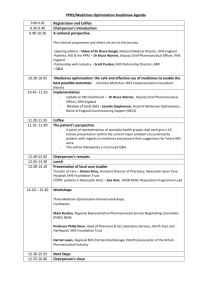
QIPP – viewed from a Foundation Trust Tony West PDIG Committee Member Chief Pharmacist, Guy’s & St Thomas’ NHS Foundation Trust The Background • GSTFT - < £1 bn turnover • Part of King’s Health Partners – KCH, SLaM & KCL... . £2 bn turnover • • • • 2/3 activity is ‘specialist’ care 1 million patient contacts per year No PFI build Viewed as ‘successful’... up until now!!! London SHA – the perfect storm ? Shift to ‘lower cost’ setting Elective core 20 % aggressive 20 % Non- elective Out-patients A &E 10 % 40 % 50 % 10 % 55 % 60 % London SHA – the perfect storm ? Decommissioning Elective core 5% aggressive 7% Out-patients A &E Diagnostics 5% 50 % 10 % 10 % 60 % 15 % Add in the national picture... • ‘Growth’ at 0.1 % above GDP deflator • Tariff – Zero growth in PbR tariff... so any growth funding for NHS will barely cover volume increase – Non-elective capped at 2008/09 activity, over activity only paid at 30 % – Looking to not pay anything for re-admissions – %age of tariff ‘withheld’ for quality... CQUINs What does that mean ? • CIP target for: – 2010 / 11 – 10% – 2011 / 12 – 5 - 10% – 2012 / 13 – 5 - 10% = • Much more for the same or • Same for much less or • Less for an awful lot less Which brings me nicely to medicines.. • London SHA planning assumptions – ‘core’... £286 m savings by 2016/17 – ‘aggressive’.... £455 m savings • GSTFT – £ 75 m.... > 10% of ‘clinical’ spend – 2/3 of which is PbR excluded... pass thru – Local PCTs looking for savings on above – PbR excluded medicines charged at acquisition cost... i.e. we add NO overhead – 2.5 % rise in VAT adds £1m extra cost QIPP • Quality – Safety – Outcome – Patient experience • Innovation • Prevention • Performance - KHP • Excellence in – Clinical care – Education & training – Research ( + application of research) • Partners, whether NHS or Academia have to address financials So... what can you do to help us ? • Understand our, i.e. NHS, environment • Cash will be tight... must recognise that – we cannot afford waste – we have to drive efficiency – we must get value for money • NHS, patients and tax payers generally – we must not compromise quality • Revolution rather than evolution ? What doesn’t work for us ? • Supply chain inefficiency – Out of stock – Short orders – Exceeding ‘quota’ – Packaging incompatible with our automation – Multiple coding – Lack of integration What doesn’t work for us ? • For the introduction of new medicines (which we DO want to see) – Duplication of effort... – Patient Access schemes – ‘Phoney’ orphan medicines – Blatant attempts to extend patent life while offering little or no value What doesn’t work for us ? • Lack of transparency – Homecare • Valuable, but if don’t know what it actually costs how can we determine real ‘value for money’ ? • Where a tied deal is with one provider.. what room for innovation and the use of ‘small businesses’ such as community pharmacists ? – VAT • UK position unique in EU... it will get challenged • Tax avoidance not a sound base for any business • Do current initiatives offer the UK tax payer true value for money ? The sad facts... • UK has one of poorest access to new medicines for its citizens • Patients still don’t get benefit from medicines they are prescribed... the adherence / concordance agenda • Transfer of care still a major problem The opportunities... • NHS structural changes... high risk but right direction • ‘Value based pricing’... the end of the UK being the ‘reference price’ ? • Supply chain is inefficient.. there must be savings for all? • Collaboration... possibly partnerships given the ‘any willing provider’ thrust of White Paper