What Is Physiatry? - University of Toledo
advertisement

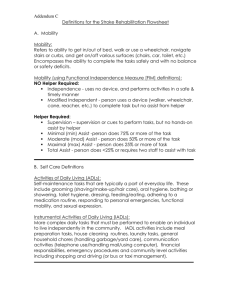
What Is Physiatry? Steven J. Farrell, MD Associate Professor and Chief Physical Medicine and Rehabilitation University of Toledo College of Medicine Who The Heck Gets Into Rehab? Disclaimer I am married to Dr. Gottwald I know nothing about skin disease I cannot get you a derm appointment sooner Objectives Give a basic overview of PM&R Discuss the principles of inpatient rehabilitation Discuss admission criteria for inpatient rehab facilities (IRF) Physiatrist Practices in the field of Physical Medicine and Rehabilitation Works with patients who posses functional disabilities History of PM&R Comes from physikos (physical) and iatreia (art of healing) Principles started during World War I Physiotherapy and reconstruction hospitals to treat war vets History of PM&R 1936 first program founded at the Mayo Clinic with the support of the War Dept and US Navy 1941 World War II broadens the scope of the field 1945 section of PM&R established in the AMA History of PM&R 1946 twenty five residencies established 1952 nearly 58,000 cases of polio become a prime focus of treatment President Franklin Roosevelt brings spotlight disabled Americans 1965 Medicare and Medicaid established 1972 Medicare expands coverage to include disabled and inpatient rehabilitation PM&R Now 78 training programs Over 1300 positions of training (350 per year) Over 8000 Board Certified Physiatrists Estimated significant need upcoming due to longer lifespan, more active elderly population, baby boomers entering the mid 60’s Toledo and PM&R Accredited residency program 21-27 bed rehab unit 6 total residents in training 50% of training slots filled by UT COM graduates 75% of practicing physiatrists graduates of UT PM&R Residency Program UT COM is in top 20 medical schools in training Board Certified Physiatrists But What Do We Do? Inpatient Rehabilitation Physiatrist is part of a team of health care professionals that work to reintegrate the disabled patient into the home and community environments Multidisciplinary approach can be very effective The Team Physical therapist Occupational therapist Speech and language therapist Counselor Nursing Therapeutic recreation specialist Social worker Physiatrist Physical Therapist Works on tasks – Mobility – Transfers – Gait – Car skills – Pain control – Education Exercise, modalities Occupational Therapist Works on tasks of upper extremities – Activities of daily living – Functional transfers – Splinting – Modalities and motor control tasks May specialize in hand therapy Speech/Language Therapists Speech and language assessment and treatment Cognitive evals and treatment Swallowing assessment and treatment – Bedside – Modified barium swallow testing Counselor May be social worker, psychologist Adaptation to disability Nursing Different than acute care floor Patients are mobile and active Education Bladder and bowel programs Decubutis care Social Worker Discharge planning Procure equipment Follow up arrangements Therapeutic Recreation Specialists Works with avocational tasks Hobbies and interests Field trips Physiatrist Follow patient’s medical and rehabilitation needs Try NOT to call medicine unless really necessary because they are our friends Medical/Rehabilitation Issues We Encounter Pulmonary Very important in cases of tetraplegia Teach respiratory techniques Wean trachs Some IRF will take vents; we do not due to staff training issues Bowel Neurogenic bowel very common and important to treat Can inhibit rehab and social progress Will start with the 3-2-1 program – Colace 100 mg TID – Senna two tabs at noon – Dulcolax suppository at night Bladder Neurogenic – Unhibited bladder Stroke Babies – Spastic TBI or SCI – Flaccid Cauda equina syndrome – Dysynergic Higher level SCI Bladder Programs Timed voids – CVA – Brain injury Intermittent straight caths – SCI Suprapubic catheter Avoid long term foley unless absolutely necessary – Reason to keep a foley??? Skin/Pressure Ulcers Direct pressure Friction Shearing Moisture Malnutrition Anemia Spasticity Can help or hurt functional recovery Treatments – Therapy – Modalities: cold – Medication: baclofen, zanaflex – Botox – Baclofen pumps – Surgical tendon release: messy and avoided if possible Who Is Eligible? Ability to participate in therapy 3 hours per day in meaningful way – Medically and motivation wise Home goal – Should have good home support or be reasonably sure they can go home alone; judgment call by the PM&R consult team INSURANCE – IRF is not the same as an acute care hospital; elective admission – Each insurance company can have their own criteria – Can take away our decision making – Until they pass health care reform then who knows? Likely not even congress Medicare Funding PPS: prospective payer system 75% rule (now 60%) Not cheap: $1000/ day 60% Rule 60 % of our patient are required to have one of the following diagnosis 60 % Rule CVA SCI Congenital deformity Amputation Hip fracture Brain injury Neurological disorders – Parkinson's, MS Burns Active RA, psoriatic arthritis Seronegative spondyloarthropathies Systemic vasculitis active 60 % Rule Joint replacement – BMI > 50 – Active weight bearing polyarthritis – Bilateral joint replacements – Age > 85 Physical Medicine Works with patients that have musculoskeletal injuries – Sports injuries – Occupational injuries – Spine – Pain Electrodiagnosis Non-operative treatment Musculoskeletal Injuries Shoulder: tendonitis Elbow: tennis elbow Hand and wrist: CTS Hip: bursitis Knee: cartilage or ligament injury Ankle: Sprains Back/Neck: strains, disc injury, nerve root Fields of Overlap Orthopedics Internal medicine Neurology Neurosurgery Rheumatology Case Quiz 82 year old with significant dementia lives with family with new onset CVA Left hemiplegia and dysphagia Otherwise in good health Acute care therapists note difficulty with patient in carryover with teaching tasks Are they a good IRF candidate? Case Quiz 66 year old female with new onset major MI; workup leads to CABG Post op patient develops pneumonia requiring IV abx Are they a good rehab candidate? Case Quiz 72 year old patient with Parkinson's Disease admitted to Med I with pneumonia and UTI On admission notes that tremors have greatly worsened and neurology consulted; they change meds but tremors are slow to respond and you are concerned about safety Are they a good rehab candidate?? Questions?