Outcome of Non Trauma Cardiac Arrest Patients without Return of
advertisement
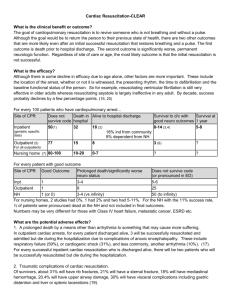
Why Emergency Physicians Don’t Care about Cardiac Arrest and Should. Robert Swor, DO Professor, Emergency Medicine Oakland University William Beaumont School of Medicine Objectives Epidemiology of Cardiac Arrest Survival Relative impact of interventions Relative impact of Phases of Care Where do Emergency Physicians Make a Difference Emergency Physician Perspectives of Cardiac Arrest Resuscitation It’s Futile We just bring back patients to a vegetative state The Only people that arrest are Gomers at the end of Life This One’s comatose-He’s Toast It’s a poor use of Health Care Dollars My Question Are physician attitudes a self fulfilling prophecy? i.e Do post arrest patients do poorly because we’re not aggressive with them in ED and hospital? Emergency Department Patient Scenarios Field Cardiac Arrest Post-Arrest- CPR in Progress Post Arrest-DefibrillatedChest burns, alert Post arrest-ResuscitatedSTEMI Post Arrest- Comatose Pre-Arrest-Crumps in the ED Cardiac Arrest Outcomes Out of Hospital Cardiac Arrest 225,000/yr 20-25% survival To Admission (40-45% of Admitted Survive to Discharge) Overall 5-10%Survival In Hospital Cardiac Arrest 75,000/yr ROSC 44% (38.6% of ROSC Survive to Discharge) 17% Survive to Discharge Neurologic Outcome Out of Hospital Arrest Neurologic Death 25-30% If survive to discharge Excellent QOL if Early Defib 5 Year survival Similar to age and health matched controls OPALS-Good quality of life for survivors at 1 year* Bunch TJ, NEJM 2003:348:2626-2633 Steill, Circ 2003:108:1939 Field Cardiac Arrest CPR not Transported to Hospital CPR in Progress on ED Arrival Futile? 1 What Happens to Field Cardiac Arrest CARES Registry 27,675 OHCA events 18,541 (67.0%) with no field ROSC. 12095 (65.2%) were pronounced in the field 5618 (30.3%) had resuscitation terminated in the ED 828 (4.5%) survived to admission Variation in Field Pronouncement after Failed Resuscitation-CARES 80 % Field Pronouncement 70 60 50 40 30 20 10 0 3 12 17 19 27 30 34 EMS Agency 36 40 55 58 Median Field Termination without ROSC-ROC Consortium 100% 90% % Termination 80% 70% 60% 50% 40% 30% 20% 10% 0% Alab Iowa Ottawa Pitt Port Site Seattle Toronto Vanc Mean Survivors To Admission 828 (14.7% of transported) Survive to Admission 128 survived to discharge (15.4%) 81 (9.8%) survived with good cerebral performance. Termination of Resuscitation in Field-Decision Rules ALS No ROSC No Bystander CPR Not witnessed arrest No shock Delivered BLS No ROSC No witnessed No AED shock Clinical Decision Rules for TOREvidence Based Review – Sherbino J. Em Med 2009:10:1016 Literature Review 4 Decision Rules 3 BLS: 1 ALS 6 Validation Studies BLS Rule –PPV 99.5% (98.9%,99.8%) Decreases transport 62.6% ALS rule-no good quality validation study Cardiac Arrest Patients are All Gomers at the End of Life? Need better work on who shouldn’t get CPR Decreased Survival with Age End of Life Planning and Care Unwanted or Not Indicated Resuscitation King County 1994 (Dull) 7% had undocumented DNR 25% Severe Chronic Disease Possible Predictors of Outcomes After Cardiac Arrest Clinical presentation Arrest factors Age Diapers Neuro exam HCT EEG N-100 Enolase Impact of Therapeutic Hypothermia Nielson Acta Anaes Scan 2009; 53:926-934 Scandinavian Registry 238 pts with Hypothermia - 7 Countries Good Neurological Outcome 22% Non VF 56% VF Neurologic Outcome Out of Hospital Arrest Neurologic Death 25-30% If survive to discharge Excellent QOL if Early Defib 5 Year survival Similar to age and health matched controls OPALS-Good quality of life for survivors at 1 year* Bunch TJ, NEJM 2003:348:2626-2633 Steill, Circ 2003:108:1939 Inability to Predict Outcomes Obstacle to initiating Aggressive Care No reliable data on predictors of outcome in first 3 days Consistent with AHA 2010 Guidelines Predicting Outcomes-Post Hypothermia ECMO To Support CPR in Adults 1992-2007 ELSO Database Adults>18 years Mean Age 52 Survival in 27% Brain Death in 29% Ann Thoracic Surg 2009:87:778-785 Case Study Refractory Cardiac Arrest 53 y/o male, severe 3 vessel ds Post op CABG-refractory VF post op day 4 65 minutes CPR during attempted resuscitationcannulation ECMO for 4 days Neuro intact, ICD placed, waiting for transplant Cost Effectiveness of Out of Hospital Cardiac Arrest Care Cost Effective Public Access Defibrillation Nichol-$56,000 (IQR $44,000,$77,000) Walker-$68,000 (Scotland) Police AED $2,000-$15,000/year of life saved Advanced Life Support Valenzuela-$8,800/year of Life saved (1990) Money Mechanics of L1CAC Survival Average Revenue Per Patient Direct Cost Per Patient Direct Margin Per Patient Discharged Alive $57,783 $37,099 $20,684 Died in Hospital $12,014 $8,686 $3,329 Lick et al. Crit Care Med 2011;39(1):26-33. 26 Conclusion CPR in progress Ominous prognosis Resuscitated arrest VF-Good outcome Non-VF- Uncertain Prognostication-Fool’s game Time’s they’re a changin’ Hypothermia Aggressive therapy