FOLFOX - Oncology
advertisement

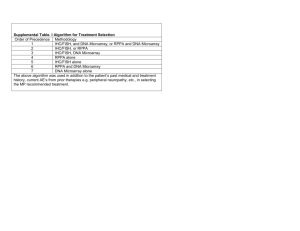
Chemotherapy for Metastatic Colon Cancer Scott Berry Sunnybrook Health Sciences Centre Where Were We Until 2000? O F HN O N H 5-FU bevacizumab oxaliplatin NH2 O C FOLFIRI Pt NH2 O C O cetuximab Panitumumab PTK 787 FOLFOX irinotecan CH3 CH2 N O N N C O IFL Capecitabine O N O HO O CH2C H3 OS for 1st line Combinations 5-FU/LV (Saltz) 5-FU/LV (Douillard) 5-FU/LV (de Gramont) IFL (Goldberg) IFL (Saltz) FOLFIRI (Douillard) FOLFOX (de Gramont) FOLFOX (Goldberg) IFL+ Bevacizumab 0 5 10 15 Median OS (months) 20 25 Overview/Objectives • Review key evidence from randomized trials evaluating the chemotherapies and chemotherapy strategies that have emerged for metastatic colorectal cancer looking at both: • Efficacy • Safety • Key Strategies and Questions: • • • • • Which doublet should be used? ? Should we be using triplet therapy Can capecitabine replace infusional 5FU in doublets? Can sequential monotherapy replace initial doublet therapy? Can toxicity be reduced and efficacy maintained with “on/off” chemotherpay strategies? Chemotherapy Case • 50 yo woman with no history of medical problems presents with bilobar liver and bilateral lung metastases – ECOG 1 – some RUQ pain and cough • What is the optimal chemotherapy choice for her? • • • • • • CAPECITABINE FOLFOX FOLFIRI CAPE IRI CAPE OX FOLFOXIRI Efficacy of Chemotherapy in FirstLine CRC: Phase III Trial Results Regimen RR (%) Median OS (mo) 5-FU/LV 21 12.6 IFL (Saltz trial) 39 (P<0.001) 14.8 (P=0.04) 5-FU/LV 22 14.1 FOLFIRI (Douillard trial) 35 (P<0.005) 17.4 (P=0.031) 5-FU/LV 22 14.7 FOLFOX4 (de Gramont trial) 51 (P=0.0001) 16.2 (P=0.12) Saltz et al. N Engl J Med. 2000;343:905; Douillard et al. Lancet. 2000;355:1041; de Gramont et al. J Clin Oncol. 2000;18:2938 • • • • • • CAPECITABINE FOLFOX FOLFIRI CAPE IRI CAPE OX FOLFOXIRI Phase III Intergroup N9741 Study (Goldberg JCO, 2004) R A N D O M I Z A T I O N IFL FOLFOX 4 Irinotecan + Oxaliplatin Phase II Sequential, Randomized CrossoverStudy FOLFIRI FOLFOX 6 Tournigand et al JCO 2004 N9741/Tournigand Trial: Results N9741 Tournigand IFL FOL FOX Pvalue FOL FOL PFIRI FOX value RR % 31 45 .03 56 54 .26 TTP mos 6.9 8.7 .009 8.5 8.0 .26 OS mos 15 19.5 .0002 21.5 20.6 .99 Tournigand Trial: Results Curative Surgery Rate: 22% FOLFOX , 9% FOLFIRI Tournigand Toxicity grade >3 % 40 P>0.05 for Comparisons marked by arrows FOLFIRI 34% FOLFOX 30 20 14% Alopecia Any grade 60% vs 28% 13% 11% 10 0% 0 10% 7% 3% 3% 3% 60-day Mortality: 4% vs 3% Combination Chemotherapy Summary • Combination chemotherapy with FOLFIRI or FOLFOX are both acceptable first line chemotherapy regimens for people with metastatic colorectal cancer • Follow by alternate combination (or single agent Irinotecan after FOLFOX) • Considerations: – Toxicity profile – ? Considering surgery : FOLFOX based on “circumstantial” evidence • • • • • • CAPECITABINE FOLFOX FOLFIRI CAPE IRI CAPE OX FOLFOXIRI Overall survival Estimated probability Capecitabine (n=603) 5-FU/LV (n=604) 1.0 0.8 0.6 0.4 0.2 13.1 13.1 0 0 5 10 15 20 Time (months) 25 30 Integrated CRC What About Capecitabine As a Partner? Capecitabine + Irinotecan BICC-C study n=430 1st line mCRC FOLFIRI +/- celecoxib mIFL +/- celecoxib CAPIRI (Cape 1000mg/m2 d1-14) +/- celecoxib FOLFIRI mIFL CAPIRI Median OS (mos) 23.1 17.6 (p=0.1) 18.9 (p=0.42) Median PFS (mos) 8.2 6.0 (p=0.01) 5.7 (p=0.01) g3/4 nausea 6.6 6.6 18.4 g3/4 vomiting 5.8 6.6 15.6 g3/4 diarrhea 13.9 16.8 47.5 g3/4 dehydration 5.8 6.6 19.1 0 0 9.9 3.6 12.4 7.1 G3/4 HFS Febrile neutropenia Slide Courtesy D Jonker from data presented at ASCO 2007 EORTC 40015 study n=85 1st line CRC FOLFIRI +/- celecoxib CAPIRI (Cape 1000mg/m2 bid x14d)+/- celecoxib FOLFIRI CAPIRI Req dose adjustment (%) 33% 53% g3/4 diarrhea 13% 37% 5 (10w) 3 (9w) Dose intensity irinotecan 85% 83% Median OS (mos) 19.9 14.8 Median PFS (mos) 9.6 5.9 Median number cycles Celecoxib vs Placebo : No Survival difference Slide Courtesy D Jonker What About Capecitabine As a Partner? Capecitabine + Oxaliplatin Capecitabine + Oxaliplatin Randomized Trials : Efficacy First Line Regimen RR (%) Median OS (mo) Capecitabine (1000 bid) + 42 19.9 Ox (130 q 3wks) 46 20.5 (p=NS) FOLFOX 6 (oxali 100 q 2wks) Non-Inferior (Ducreux ASCO 2007 N=306) Capecitabine + Ox NR FOLFOX 4 19.6 19.8 (p=NS) (Cassidy ASCO 2007 N=2034) Second Line Capecitabine+ Ox 15 13.2 FOLFOX 4 12 12.8 (p=NS) (Rothenberg ASCO 2007 N= 627) Capecitabine + Oxaliplatin Randomized Trials : Toxicity First Line Regimen Toxicity Capecitabine (1000 bid) + Ox (130 q 3wks) FOLFOX arm had significantly more Gr 3/4: FOLFOX 6 (oxali 100 q 2wks) Neuropathy (25 v 11%), Feb Neut (6 v 0%) (Ducreux ASCO 2007 N=306) Capecitabine + Ox FOLFOX arm had more Gr 3/4: FOLFOX 4 Feb Neut (5 v <2%) (Cassidy ASCO 2007 N=2034) CapeOx arm had more Gr 3/4: Diarrhea (20 v 12%) and HFS (6 v 1%) Second Line Capecitabine + Ox FOLFOX arm had more Gr 3/4: FOLFOX 4 Feb Neut (Rothenberg ASCO 2007 N= 627) CapeOx arm had more Gr 3/4: Diarrhea (20 v 7) and HFS (4 v <2%) Can Capecitabine Replace Infusional 5FU in mCRC? • Capecitabine and Irinotecan – At doses studied CapeIri is more toxic and less effective than FOLFIRI • Capecitabine and Oxaliplatin – CapeOx has same efficacy as FOLFOX – Differential toxicity profile between CapeOx and FOLFOX • • • • • • CAPECITABINE FOLFOX FOLFIRI CAPE IRI CAPE OX FOLFOXIRI Triplet Therapy 5-FU/IRI vs FOLFOXIRI: Falcone et al N = 244 5-FU/Iri Douillard Randomization FOLFOXIRI Slide Courtesy of R Goldberg FOLFOXIRI Schedule Day 1 Day 2 Day 3 CPT-11 165 mg/m2 Oxaliplatin 85 mg/m2 L-LV 200 mg/m2 1 hour 2 hours 5FU flat continuous infusion 3200mg/m2 48 hours Repeated every 14 days Slide Courtesy of R Goldberg Efficacy Response rate (%) PFS (mos) OS (mos) 5-FU/IRI N=122 41% FOLFOXIRI N=122 66% P-value 6.9 (BICC = 8.3) 16.7 9.9 0.0009 23.6 0.042 ? Slide Courtesy of R Goldberg Post-ChemoRx Resections (patients with liver mts only) FU/IRI (42 pts) R0 12%* (5 pts) FOLFOXIRI (39 pts) 36%* (14 pts) * p=0.017 Slide Courtesy of R Goldberg Grade 3-4 Toxicity 100% 100% 75% FOLFIRI (N=122) FOLFOXIRI (N=122) 75% p =0.0006 50% 50% 50% 5 28% 25% 25% 3% 5% 1% 2% 1% 3% 20% 12% 0% 20% 2% Neutropenia Febrile Neutropenia Thrombocytopenia Anemia 7% 3% 5% 3% 6% Stomatitis Asthenia Neurotoxicity 0% 0% Diarrhea Vomiting Slide Courtesy of R Goldberg Survival improves with availability of three active drugs * FOLFOXIRI P=0.0001 Grothey A, Sargent D. J Clin Oncol. 2005;23:9441-9442. Is FOLFOXIRI more active than 5-FU/IRI? Yes, including better resection rates But is comparator arm inferior? More toxic Monotherapy Overall survival Estimated probability Capecitabine (n=603) 5-FU/LV (n=604) 1.0 0.8 0.6 0.4 0.2 13.1 13.1 0 0 5 10 15 20 Time (months) 25 30 Integrated CRC Monotherapy versus doublets • ? Have 3 active chemo agents in mCRC • Lead with combination • ? Can we use agents sequentially and maintain efficacy and reduce toxicity • FOCUS and CAIRO – Do both have fatal flaws? FOCUS Lancet, 2008 FOCUS UK MRC CR08 2,135 Untreated Stage IV patients R A N D O M I S A T I O N A: 5 FU/LV (de Gramont) IRI B: 5 FU/LV (de Gramont) FOLFOX or FOLFIRI C: FOLFOX vs FOLFIRI FOCUS UK MRC CR08 • Breaks allowed – Not before 3 mos – Only 4 weeks in 2nd 3 mos – After that – allowed with re-start of previous regimen as long as progression hadn’t occurred within 12 weeks of stopping FOCUS UK MRC CR08 • Up to Dec 02 , recommended salvage in all groups Infusional 5FU and Mit-C • Since Dec 02, "balanced salvage" with CapOx or CapIri • Primary Endpoint: Survival Survival OS (mos) 5FU TO IRI 13.9 5FU TO FOLFOX 15.2 5FU TO FOLFIRI 15.0 FOLFOX 15.4 FOLFIRI 16.7 (p=0.01) Table 4 FOCUS QOL • Mean overall QOL : varied little between arms and regimens • In particular, no differences seen at 3 and 6 mos FOCUS • Conclude that sequential strategy is a valid option • Median Survivals of all arms inferior to FOLFOX arm of N9741 and both arms of Tournigand trial • ? Seeing an effect of restricting access to all 3 drugs Percentage of Patients Receiving All 3 Active Drugs OS (mos) A B 5FU TO IRI 5FU TO FOLFOX 5FU TO FOLFIRI 16% 19% FOLFOX 33% C FOLFIRI FOCUS Grothey, JCO, 2004 CAIRO Randomized study of sequential versus combination chemotherapy with capecitabine, irinotecan and oxaliplatin in advanced colorectal cancer a study of the Dutch Colorectal Cancer Group (DCCG) CJA Punt, M Koopman, J Douma, J Wals, AH Honkoop FLG Erdkamp, RS de Jong, CJ Rodenburg, L Mol, NF Antonini ASCO 2007 CAIRO study CKTO 2002-07 Randomize Arm A Arm B capecitabine capecitabine + irinotecan 2nd line irinotecan capecitabine + oxaliplatin 3rd line capecitabine + oxaliplatin 1st line Dose/schedule of drugs all cycles given 3 weekly • • • • Capecitabine monotherapy: 1250 mg/m2 b.i.d. day 1-14 Irinotecan monotherapy: 350 mg/m2 day 1 CAPIRI1: capecitabine 1000 mg/m2 b.i.d. day 1-14 + irinotecan 250 mg/m2 day 1 CAPOX2: capecitabine 1000 mg/m2 b.i.d. day 1-14 + oxaliplatin 130 mg/m2 day 1 Rea et al. Ann Oncol 2005 2 Borner et al. J Clin Oncol 2002 1 Trial profile Randomize Arm A 1st 2nd Arm B line capecitabine N=397 capecitabine + irinotecan N=398 line irinotecan N=251 (62%) capecitabine + oxaliplatin N=213 (53%) 3rd line capecitabine + oxaliplatin N=143 (36%) Median overall survival Combination treatment 17.4 months (15.2-19.2) ----------- Sequential treatment 16.3 months (14.3-18.2) p= 0.33 Efficacy results Sequential N=401 Combination N=402 p value Median overall survival (months) 16.3 17.4 0.33 Hazard ratio for death 1.08 One-year survival rate (%) 64 67 Median PFS (months) 1st line 5.8 7.8 Overall response rate (CR + PR)* 1st line 2nd line 3rd line 77 (20%) 23 (10%) 5 (4%) 139 (41%) 24 (12%) - Disease control rate (CR + PR + SD)* 1st line 2nd line 3rd line 280 (74%) 162 (71%) 72 (57%) 297 (87%) 121 (63%) * Percentages are based on patients evaluable for response 0.0002 Grade 3-4 toxicities in first line Arm A capecitabine N = 397 Arm B capiri N = 398 p value Hand-foot syndrome 12% 6% 0.002 Diarrhea 11% 26% <0.001 Nausea 4% 10% 0.004 Vomiting 3% 9% 0.0002 Stomatitis <1% 2% 0.16 Thrombosis/embolism * 7% 10% 0.20 Febrile neutropenia <1% 7% <0.001 Toxicity * All grades Quality of life • • • Participation to this part of the study was proposed to the first 620 patients entered in the study (QLQ-C30 questionnaire of the EORTC) 403 patients were evaluable for quality of life Quality of life scores were comparable between the two arms, except for diarrhoea which was reported more frequently in combination treatment Conclusions • • • • Combination treatment is not superior in terms of efficacy to sequential treatment in patients with advanced colorectal cancer Our results on median overall survival for sequential treatment are the highest reported when a fluoropyrimidine is administered as monotherapy in 1st line Sequential treatment is a useful alternative for combination treatment Our results may be useful for strategies in which chemotherapy is combined with targeted agents What about use of CapeIri? 62 Back to CAIRO • PFS Capeiri in CAIRO similar to FOLFIRI in BICC-C – But OS of 17 mos is less than we’ve come to expect in sequential doublets – Cross trial comparisons – CapeIri in CAIRO better tolerated than CapeIri in BICC-C or EORTC trial except for high rates of diarrhea (~ double that seen with FOLFIRI in Tournigand or BICC-C) • Would Combination arm in CAIRO have done better if FOLFIRI used? – No one knows. 63 ? Reasons for Results • ? Geographic differences in capecitabine metabolism – Similar results in Europe • ? Celecoxib – Results not published for BICC-C • ? Different dose of cape do better – Maybe but not used in this trial 64 Summary • Both CAIRO and FOCUS validate a sequential approach within the context of their study parameters • ? Would they have done so if FOCUS had allowed better access to all 3 chemo drugs and CAIRO had used FOLFIRI? 65 Is Less Chemo More? Case • 50 yo woman with no history of medical problems presents with bilobar liver and bilateral lung metastases – ECOG 1 – some RUQ pain and cough She agrees to chemotherapy but asks if there is anyway she can take a break during chemo without reducing the benefits of chemo? Which of the following strategies has been shown to reduce toxicity without impacting on efficacy? • Induction of FOLFOX for 3 mos followed by infusional 5FU maintanence then reintroduce FOLFOX • Induction of FOLFOX for 3 mos followed by no maintanence (complete chemo break) then reintroduce FOLFOX • FOLFIRI on for 2 mos, off for 2 mos Stop and Go concept - OPTIMOX1 FOLFOX4 R 6x FOLFOX7- 12x sLV5FU2 - 6x FOLFOX7 620 pts Cum. Oxali (%) FOLFOX4 RR 58.5 PFS 9.0 DDC 9.0 OS 19.3 G3/4 NTox 17.9 780 1560 FOLFOX7 58.3 8.7 10.6 21.2 13.3 Primary endpoint Tournigand et al, JCO 2006 OPTIMOX2, a large randomized phase II study of maintenance therapy or chemotherapy-free intervals (CFI) after FOLFOX in patients with metastatic colorectal cancer (MRC). A GERCOR study. F. Maindrault-Gœbel, G. LLedo, B. Chibaudel, L. Mineur, T. André, M. Bennamoun, M. Mabro, P.Artru, C. Louvet, A. de Gramont OPTIMOX Studies FOLFOX 4 until TF OPTIMOX-1 FOLFOX 7 FOLFOX 7 sLV5FU2 mFOLFOX 7 mFOLFOX 7 sLV5FU2 OPTIMOX-2 mFOLFOX 7 mFOLFOX 7 CFI Baseline Progression T size Chemotherapy-free Interval t FOLFOX FOLFOX Progression Baseline progression Progression at reintroduction Duration of Disease Control DDC = PFS 1 + PFS 2 (if no PD) T size PFS 1 PFS 2 t FOLFOX FOLFOX Progression ASCO 2001, 146a Baseline progression Progression at reintroduction Neuropathy Optimox 1 Optimox 2 Grade 1 70.7 % 2 18.1 % 3 0 % Grade 1 70.8 % 2 16.5 % 3 0 % 2 months after FOLFOX Grade 1 8% 2 21.2 % 3 2% Grade 1 6.8 % 2 15.5 % 3 3.9 % After the first reintroduction Grade 1 29.4 % 2 35.3 % 3 5.9 % Grade 1 36.8 % 2 19.2 % 3 7% During C1-C6 Chemotherapy-free Interval C h e m o th e ra p y-fre e in te rv a l 1 .0 y t i l i b a b o r P 0 .8 O P T I M O X 2 m e d ian 1 7 we e ks R 0 s urg e ry e xc lud e d 0 .6 0 .4 0 .2 0 .0 0 10 20 30 40 50 weeks 60 70 80 90 100 Duration of Disease Control D u ra tio n o f D is e a s e C o n tro l 1 .0 y t i l i b a b o r P O P T I M O X 1 m e d ian 5 2 we e ks 0 .8 O P T I M O X 2 m e d ian 3 9 we e ks 0 .6 p = 0 .3 9 0 .4 0 .2 0 .0 0 10 20 30 40 50 weeks 60 70 80 90 100 Overall Survival O v e ra ll S u rv iv a l 1 .0 y t i l i b a b o r P O P T I M O X 1 m e d ian 2 6 m o nths 0 .8 O P T I M O X 2 m e d ian 1 9 m o nths 0 .6 p = 0 .0 5 4 9 0 .4 0 .2 0 .0 0 10 20 30 m o n th s 40 50 Alternating vs continuous FOLFIRI in advanced colorectal cancer (ACC): a randomized GISCAD trial Roberto Labianca Ospedali Riuniti – Bergamo, Italy Floriani I, Cortesi E, Isa L, Zaniboni A, Marangolo M, Frontini L, Barni S, Beretta GD, Sobrero A GISCAD-Trial: Design N=336 FOLFIRI R Evaluation 4 mos • Primary endpoint: OS PFS Median f-up: 30 m Median time to PD: Arm A 6.2 m Arm B 6.5 m Cox analysis (after adjustment for gender, age and site): HR: 1.01 (0.78-1.27) OS Median f-up: 30 m Median survival time: Arm A 16.9 m Arm B 17.6 m Cox analysis (after adjustment for gender, age and site): HR: 1.03 (0.78-1.35) Toxicity • Grade 3/4 toxicities similar in both arms – This paradigm of toxicity measurement is not appropriate for this type of trial • No QOL analysis Summary • GISCAD – Equivalent DFS, OS, toxicity – ? Rationale clinical strategy • OPTIMOX2 • ? Longer induction needed • ? Shorter break before re-introduction • ? Different maintenance strategy From OPTIMOX to DREAM OPTIMOX-1 OPTIMOX-2 DREAM Efficacy = Toxicity Efficacy decresed Toxicity = Bevacizumab Erlotinib Bevacizumab