ASCO Update 2012:
Gastrointestinal Malignancies
Thomas J. Semrad MD, MAS
Assistant Professor of Medicine
Division of Hematology/Oncology
Disclosure
• Speaker’s Bureau: Novartis
• Consulting: Amgen, Genomic Health
• Research Funding: Novartis, Millenium, NCI
ASCO 2012: Non-Colorectal Topics
Esophagogastric Cancer
– Locoregional Disease: Alternative to cisplatin / 5fluorouracil chemoradiation
– Advanced Disease: Another negative trial of a
biologic in unselected patients
Anal Cancer
– Timing of response assessment
HCC
– Optimizing supportive care
Phase III randomized trial of definitive
chemoradiotherapy (CRT) with FOLFOX or cisplatin
and fluorouracil in esophageal cancer (EC): Final
results of the PRODIGE 5/ACCORD 17 trial.
Abstract #LBA4003
Thierry Conroy, Marie-Pierre Galais, Jean Luc Raoul, Olivier Bouche, Sophie Gourgou-Bourgade, Jean-Yves Douillard, PierreLuc Etienne, Valérie Boige, Isabelle Martel-Lafay, Pierre Michel, Carmen Llacer-Moscardo, Jocelyne Berille, Laurent Bedenne,
Antoine Adenis
J Clin Oncol 30, 2012 (suppl; abstr LBA4003)
Chemoradiation in Esophageal Cancer
RTOG 85-01
• median survival
– 14 months vs. 9 months
• 5 year survival
– 27% vs. 0%
• Local failure 45%
• Major toxicity 20%
NEJM 1992; 326: 1593-8.
Prodige 5 – ACCORD 11 Study Design
Unresectable Esophageal
Cancer
• AdenoCa or SCCa
• No Prior Treatment
• No weight loss > 20%
• No tracheal invasion or TE
fistula
N = 267
Stratified By:
Histology
Weight Loss (+/- 10%)
PS
Center
FOLFOX + 50Gy
Then
FOLFOX x 3 cycles
5FU/cisplatin + 50Gy
Then
5FU/cisplatin x 2 cycles
Primary Endpoint:
Progression Free Survival
Secondary Outcomes
1. CR rate
2. Toxicity
3. Time to treatment
failure
4. OS
5. QOL
90% Power to detect 20% increase in 3-year PFS
N = 266 planned (144 events)
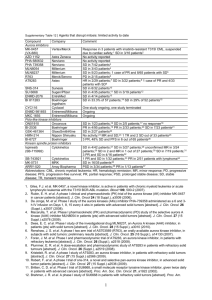
[TITLE]
[TITLE]
[TITLE]
Prodige 5 – ACCORD 11 Efficacy
PFS
OS
Conclusion
• FOLFOX is not superior to 5-FU/cisplatin for
definitive chemoradiation treatment for
unresectable esophageal cancer
• This trial will be used to demonstrate clinical
efficacy of definitive FOLFOX chemoradiation
• How does this compare to weekly carboplatin /
paclitaxel?
Which Regimen?
• Carbo/Taxol – CROSS
– Neoadjuvant Study
(reduced radiation dose)
– pCR rate ~30%
– Effective in both SCCa and
adenoCa
– What is the systemic
efficacy?
• FOLFOX – Prodige 5
– Inoperable study
– Not superior to cisplatin/5FU
– Mostly SCCa, but used
often in advanced adenoCa
– More systemic therapy
Reality of practice – neoadjuvant CRT used to
select operable patients
NEJM 2012; 388:274-284
J Clin Oncol 30, 2012 (suppl; abstr LBA4003)
A randomized, multicenter trial of epirubicin,
oxaliplatin, and capecitabine (EOC) with or without
panitumumab in advanced esophagogastric cancer
(REAL3).
Abstract #LBA4000
Tom Samuel Waddell, Ian Chau, Yolanda Barbachano, David Gonzalez de Castro, Andrew Wotherspoon, Claire Saffery, Gary
William Middleton, Jonathan Wadsley, David Raymond Ferry, Wasat Mansoor, Tom David Lewis Crosby, Fareeda Y Coxon, David
Smith, Justin S. Waters, Timothy Iveson, Stephen Falk, Sarah Slater, Alicia Frances Clare Okines, David Cunningham
J Clin Oncol 30, 2012 (suppl; abstr LBA4000)
REAL-3 Background
NEJM 2008;358:36-46.
Gastric Cancer 2012;15:252-264.
[TITLE]
Counterintuitive Observations:
OS outcome more extreme than PFS outcome
EOX
mEOX-P
(n=238)
(n=254)
RR in opposite direction of OSCR results
2%
3%
PR
40%
43%
SD
21%
18%
PD
8%
12%
Not evaluable
29%
24%
ORR
42%
46%
[TITLE]
[TITLE]
Dose Intensity
Median Number of Cycles
EOX
EOX-P
6
5
Dose intensity
Epirubicin
89.9%
89.1%
(% of expected dose)
Oxaliplatin
89.9%
89.6%
Capecitabine
91.0%
86.9%
Panitumumab
-
88.1%
Dose reductions for toxicity
36%
39%
Treatment cessation for toxicity
18%
18%
J Clin Oncol 30, 2012 (suppl; abstr LBA4000)
[TITLE]
Take Home Points
• No evidence of benefit for the addition of
panitumumab to EOX
• Inferior OS may be due to inferior dose intensity
of the experimental regimen
• RR was not a good surrogate for survival
outcomes, and OS worse than PFS
Optimum time to assess complete clinical
response (CR) following chemoradiation (CRT)
using mitomycin (MMC) or cisplatin (CisP), with or
without maintenance CisP/5FU in squamous cell
carcinoma of the anus: Results of ACT II.
Abstract #4004
Robert Glynne-Jones, Roger James, Helen Meadows, Rubina Begum, David Cunningham, John Northover, Jonathan A.
Ledermann, Sandra Beare, Latha Kadalayil, David Sebag-Montefiore
J Clin Oncol 30, 2012 (suppl; abstr 4004)
ACT II Factorial Design
N=940
MMC + 5-FU + XRT
No Maintenance
MMC + 5-FU + XRT
Maintenance
CisP + 5-FU + XRT
No Maintenance
CisP + 5-FU + XRT
Maintenance
1. MMC vs. Cisplatin
2. Maintenance vs. No Maintenance
[TITLE]
[TITLE]
Timing of CR Assessment
[TITLE]
[TITLE]
[TITLE]
Message: Be patient with response assessment
A randomized controlled phase II study of the
prophylactic effect of urea-based cream on the
hand-foot skin reaction associated with sorafenib
in advanced hepatocellular carcinoma.
Abstract #4008
Zhenggang Ren, Kangshun Zhu, Haiyan Kang, Minqiang Lu, Zengqiang Qu, Ligong Lu, Tianqiang Song, Weiping Zhou, Hui
Wang, Weizhu Yang, Xuan Wang, Yongping Yang, Lehua Shi, Yuxian Bai, Sheng-Long Ye
J Clin Oncol 30, 2012 (suppl; abstr 4008)
[TITLE]
HFSR Grading
CTCAE v3.0
Grade
1
2
3
4
Rash:
hand-foot skin
reaction
Minimal skin
changes or
dermatitis (e.g.,
erythema)
without pain
Skin changes
(e.g.,
peeling, blisters,
bleeding,
edema) or pain,
not interfering
with
function
Ulcerative
dermatitis or
skin changes
with pain
interfering with
function
_
[TITLE]
ASCO 2012: Colorectal Topics
Maintenance
– Combining Anti-VEGF and Anti-EGFR therapy
Anti-Angiogenic Therapy
– Bevacizumab Beyond Progression
– Aflibercept in Second Line
– A new multi-targeted agent in advanced disease
Bevacizumab (Bev) with or without erlotinib as
maintenance therapy, following induction first-line
chemotherapy plus Bev in patients with metastatic
colorectal cancer (mCRC): Efficacy and safety results of the
International GERCOR DREAM phase III trial.
Abstract #LBA3500^
Christophe Tournigand, Benoit Samson, Werner Scheithauer, Gérard Lledo, Frédéric Viret, Thierry Andre, Jean François
Ramée, Nicole Tubiana-Mathieu, Jérôme Dauba, Olivier Dupuis, Yves Rinaldi, May Mabro, Nathalie Aucoin, Ahmed Khalil, Jean
Latreille, Christophe Louvet, David Brusquant, Franck Bonnetain, Benoist Chibaudel, Aimery De Gramont
J Clin Oncol 30, 2012 (suppl; abstr LBA3500^
Combined anti-VEGF and anti-EGFR
• CAIRO2
N Engl J Med 2009;360:563-72.
• PACCE
JCO 2009;27:5672-5680
[TITLE]
OPTIMOX3 – DREAM Schema
Bevacizumab 7.5 mg/kg
q21 days
+
Erlotinib 150 mg daily
Inclusion/Exclusion
Metastatic CRC
Not suitable for surgery
No PD
Front-line Treatment
mFOLFOX7 + bev (6-12)
XELOX2 + bev (6-12)
FOLFIRI + bev (12)
Stratified By:
Treatment Regimen
Bevacizumab 7.5 mg/kg
q21 days
Primary Endpoint:
PFS on Maintenance
Secondary Outcomes
1. OS
2. OS from maintenance
3. Duration without
chemotherapy
4. RR
5. OS according to KRAS
80% Power to detect PFS increase 4.5 to 6.5 mo
Anticipated 40% dropout
N = 700 (418 evaluable)
[TITLE]
[TITLE]
Conclusion
The combination of EGFR- and VEGF-targeted
agents is not dead*
*But should not (yet) be used in routine clinical practice
Bevacizumab (BEV) plus chemotherapy (CT) continued beyond
first progression in patients with metastatic colorectal cancer
(mCRC) previously treated with BEV plus CT: Results of a
randomized phase III intergroup study (TML study).
Abstract #CRA3503
Dirk Arnold, Thierry Andre, Jaafar Bennouna, Javier Sastre, Pia J. Osterlund, Richard Greil, Eric Van Cutsem, Roger Von Moos,
Irmarie Reyes-Rivera, Belguendouz Bendahmane, Stefan Kubicka
J Clin Oncol 30, 2012 (suppl; abstr CRA3503
BRiTE Registry
No BBP
BBP
Median OS
19.9 months
31.8 months
OS Beyond PD
9.5 months
19.2 months
JCO 2008; 26:5326-5334.
TML Study Design
(AIO KRK 0504, ML18147)
Metastatic CRC
• Front line chemo (either
oxaliplatin- or irinotecanbased) + bevacizumab
• Progression within 4 wks
• Not surgical candidate
• Front-line PFS > 3 months
• PD within 3 months of bev
N = 820
Stratified By:
First line chemotherapy
First line PFS +/- 9 months
Time from last bev dose +/- 45 days
PS
Standard Second Line
Chemo
+
Bevacizumab
2.5 mg/kg/wk
Standard Second Line
Chemo
Primary Endpoint*:
OS from randomization
Secondary Outcomes
1. PFS
2. RR
3. Safety
90% Power to detect 30% increase in median OS
N = 810*
* Increased from 572 with endpoint change PFS->OS
[TITLE]
[TITLE]
OS
PFS
[TITLE]
[TITLE]
[TITLE]
TML Discussion
TOP LINE RESULTS
OS 9.8 -> 11.2 months (+1.4 months), HR 0.81 (95% CI 0.69 – 0.94)
PFS 4.1 -> 5.7 months (+1.6 months), HR 0.68 (95% CI 0.59 – 0.78)
RR low (~5%) in both arms
Toxicity is as expected
Select Patient Group
UNANSWERED QUESTIONS
?
1. Is it worth it?
2. Third line? Thirteenth line?
3. Aflibercept? -> See next abstract
?
Effects of prior bevacizumab (B) use on outcomes from
the VELOUR study: A phase III study of aflibercept (Afl)
and FOLFIRI in patients (pts) with metastatic colorectal
cancer (mCRC) after failure of an oxaliplatin regimen.
Abstract #3505
Carmen Joseph Allegra, Radek Lakomy, Josep Tabernero, Jana Prausová, Paul Ruff, Guy Van Hazel, Vladimir Mikhailovich
Moiseyenko, David R Ferry, Joseph J McKendrick, Eric Van Cutsem
J Clin Oncol 30, 2012 (suppl; abstr 3505
Aflibercept
KEY FEATURES
Aflibercept
Fusion Protein
VEGFR-1
Binds all VEGF-A isoforms,
VEGF-B, and PlGF
IgG
VEGFR-2
Fc
High Affinity: binds VEGF-A
and PlGF more tightly than
native receptors
t1/2 ~ 17 days
VELOUR Study Design
Metastatic CRC
• Front line oxaliplatinbased chemo
• Relapse within 6 months
adjuvant FOLFOX
• Not surgical candidate
• Front-line PFS > 3 months
• PD within 3 months of
last bevacizumab
FOLFIRI
+
Aflibercept 4 mg/kg
Q2 weeks
FOLFIRI
Q2 weeks
Primary Endpoint*:
OS from randomization
Secondary Outcomes
1. PFS
2. RR
3. Safety
N = 1200
Stratified By:
PS
Prior Bevacizumab
90% Power to detect OS HR 0.8
N = 1200
[TITLE]
[TITLE]
[TITLE]
[TITLE]
[TITLE]
[TITLE]
[TITLE]
Velour Discussion
TOP LINE RESULTS
OS 12.1 -> 13.5 months (+1.4 months), HR 0.82 (95% CI 0.71 – 0.94)
PFS 4.7 -> 6.9 months (+2.2 months), HR 0.76 (95% CI 0.58 – 0.99)
No apparent interaction with prior bevacizumab treatment
RR trends higher (up to 23.3%)
Toxicity is increased
UNANSWERED QUESTIONS
?
1. Is it worth it?
2. How to sequence with bevacizumab?
-> See prior abstract
?
Phase III CORRECT trial of regorafenib in
metastatic colorectal cancer (mCRC).
Abstract #3502
Eric Van Cutsem, Alberto F. Sobrero, Salvatore Siena, Alfredo Falcone, Marc Ychou, Yves Humblet, Olivier Bouche, Laurent
Mineur, Carlo Barone, Antoine Adenis, Josep Tabernero, Takayuki Yoshino, Heinz-Josef Lenz, Richard M. Goldberg, Daniel J.
Sargent, Frank Cihon, Andrea Wagner, Dirk Laurent, Axel Grothey
J Clin Oncol 30, 2012 (suppl; abstr 3502)
[TITLE]
CORRECT Study Design
Metastatic CRC
• Chemorefractory
(oxaliplatin, irinotecan, 5FU)
• EGFR Ab refractory (KRAS
WT)
•PS 0-1
N = 760
Stratified By:
Time from diagnosis to mets
Prior anti-VEGF therapy
Geographic Region
Regorafenib 160 mg daily
3 weeks on, 1 week off
+
BSC
2:1
Placebo
3 weeks on, 1 week off
+
BSC
Primary Endpoint:
OS from randomization
Secondary Outcomes
1. PFS
2. ORR
3. DCR
90% Power to detect 33.3% increase (HR 0.75)
1-sided alpha 0.05
N=690 planned, with 2 interim analysis
OS
PFS
[TITLE]
[TITLE]
The Evolving Anti-Angiogenic Landscape in CRC
Challenges for Integration into Practice
The overall benefit of each of these new observations is modest
Is there a subset with greater benefit?
There is no comparison between them
Bevacizumab versus Aflibercept?
Is regorafenib extended anti-VEGF therapy?
The Way Forward
A predictive biomarker
Alternate targets