Procalcitonin Update
advertisement

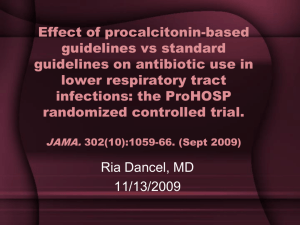
A Service Evaluation of Procalcitonin after PRORATA Daniel Cottle DICM John Butler, Tony Dunne, Sanchia Pickering Manchester Royal Infirmary 2011 Antimicrobial resistance in ICU CPC MRSA Antimicrobial resistance in ICU • Major factor affecting patient outcome and resources. • Insufficient infection control measures. • Selective antibiotic pressure. • Reducing antibiotic use may contain the emergence of multi-drug resistance bacteria in ITUs. • Stop inappropriate prescribing. • Shorten duration of treatment of antibiotics. Procalcitonin • Normally produced by the C-cells of the thyroid • Normally undetectable • Unknown role in sepsis • Multiple sources in sepsis • Analgesic Procalcitonin – in relevant bacterial infection produced and released into circulation from the whole body Calcitonin in healthy persons PCT in bacterial infection Calcitonin Müller B. et al., JCEM 2001 www.procalcitonin.com PCT Procalcitonin- Kinetics Fast increase of PCT after bacterial challenge Brunkhorst FM et alIntens Care Med 1998; 24:888-892 • Fast increase (after 3-4 hours), high dynamic range • Wide concentration range < 0.05 ng/ml - 1000 ng/ml • Short half-life time (~ 24 h) independent of renal function • Easy to measure in serum and plasma - stable in vivo and in vitro PRORATA Lancet 2010 • Multicentre, randomised, controlled trial. • 311 procalcitonin, 319 control. • Days without antibiotics: – 14.3 days PCT : 11.6 control. • The mean duration of the first episode of antibiotics was reduced from 9.9 days to 6.1 days, AR 3.8 days; 95% CI 2.7-4.8, p<0.0001 • No increase in mortality Figure 3 Source: The Lancet 2010; 375:463-474 (DOI:10.1016/S0140-6736(09)61879-1) Terms and Conditions Methods • • • • • • • • • Baseline data collection Protocol Introduction of protocol Promote protocol Reinforce protocol Data collection Analysis Mean (standard deviation) Student’s t-test Exclusions • • • • • Post bone marrow transplant Pregnancy TB, PCJ, toxoplasmosis Neutropenia Expected to die Example Patient 38 25 350 300 20 15 200 WBC CRP PCT & WBC 250 150 10 PCT CRP 100 5 50 0 0 1 2 3 4 5 6 7 Days Date Clinical events Antibiotics CRP WBC PCT Microbiology culture Temp Lactate Highest or Lowest Ventilated Y/N Antibiotic Changes 8/12/2011 coamoxyclav, clari 331 14.2 15 y 8/13/2011 coamoxyclav, clari 310 20.8 11 y 8/14/2011 coamoxyclav, clari 225 19.5 6.5 y 8/15/2011 coamoxyclav, clari 13.4 3.2 y 8/16/2011 coamoxyclav, clari 33 11 1.4 y y 8/17/2011?chest sepsis Tazocin 51 13.1 y n Results 60 antibiotic episodes 8 to the ward 4 died 6 exclusions 42 analysed 42 analysed 29 stopped early 8 no difference 1 escalated because 4 escalated despite Overall Course length prePCT 8.6 (5.3) Course length post PCT 6.5 (2.9) Difference 2.1 days p=0.05 CI 0.0 - 4.2 Chest Abdominal Others Overall Course length prePCT 8.6 (5.3) Course length post PCT 6.5 (2.9) Difference 2.1 days p=0.05 CI 0.0 - 4.2 Chest Abdominal Others Overall Chest Course length prePCT 8.6 (5.3) 7.7 (1.8) Course length post PCT 6.5 (2.9) 5.5 (1.6) 2.1 days p=0.05 2.2 days p<0.0001 CI 0.0 - 4.2 CI 1.2 – 2.8 Difference Abdominal Others Overall Chest Course length prePCT 8.6 (5.3) 7.7 (1.8) Course length post PCT 6.5 (2.9) 5.5 (1.6) 2.1 days p=0.05 2.2 days p<0.0001 CI 0.0 - 4.2 CI 1.2 – 2.8 Difference Abdominal Others Overall Chest Abdominal Others Course length prePCT 8.6 (5.3) 7.7 (1.8) No data No data Course length post PCT 6.5 (2.9) 5.5 (1.6) 7.9 6.0 2.1 days p=0.05 2.2 days p<0.0001 CI 0.0 - 4.2 CI 1.2 – 2.8 Difference Chest sepsis • • • • Mean course length 5.5 days PRORATA: CAP 5.5 days, VAP 7.7 days 8 had a starting PCT <0.5 3 could have stopped earlier Abdo sepsis • • • • Mean course length 7.9 days PRORATA: 8.1 days 4 escalated despite PCT 1 could have stopped earlier Conclusions • PCT reduced antibiotic use on our unit • Definite end-point • More structured approach • Could this be reduced further? • PCT <0.5 as a rule out? QUESTIONS?