Gram-Negative Rods
advertisement
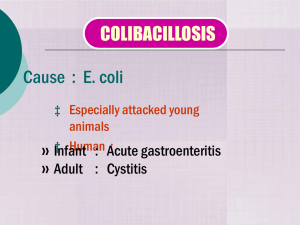
Gram-Negative Rods General Classification Based on source or site of infection 1. Enteric tract 2. Respiratory tract 3. Animal sources Source or site of infection Enteric tract Primarily within: Shigella, vibrio, Campylobacter Both within and outside: Escherichia, Salmonella Enteric but outside only: Klebsiella, Enterobacter, Serratia, Proteus, Providencia, Morganella, Pseudomonas, Bacteroides Source or site of infection (continued) Respiratory tract: Haemophilus, Legionella, Bordetella Animal sources: Brucella, Francisella, Pasteurella, Yersinia Classification Based on morphology, biochemical traits and genetic (phylogenetic) relationship Cocobacilli Vibrionaceae Pseudomonaseae Enterobacteriaceae Enterobacteriaceae A heterogenous family Mostly found in colon of human and other animals Different pathogenetic mechanisms Facultative anaerobic Glucose fermentation None have cytochrome oxidase Reduce nitrates to nitrites Most important genuses in Enterobacteriaceae family Escherichia Shigella Salmonella Klebsiella Enterobacter Serratia Proteus Yersinia In contrast to Enterobacteriaceae Pseudomonaceae Gram negative rods: Non-fermenting (Strict aerobic) Not reduce nitrate Oxidase-positive General structure of cells in Enterobacteriaceae All have Endotoxin Some have Exotoxins, mostly called enterotoxins Three surface antigens: O antigen: outer polysaccharide portion of the lipopolysaccharide (repeating 3-4 oligosaccharide sugars 15-20 times). A basis for the serologic typing (about 2000 types of Salmonella and 150 types of E. coli). H antigen: on the flagellar protein (in E.coli and Salmonella and not in Klebsiella and shigella). Unusual H antigens in Salmonella called phase 1 and phase 2. The organism can reversibly change in antigenicity to evade the immune response. K polysaccharide antigen: In encapsulated organisms such as Klebsiella. Identified by quellung (capsular swelling) reaction in the presence of specific antisera used for epidemiologic purposes. In S. typhi, it is called Vi (or virulence) antigen. Quellung (capsular swelling) reaction Coliforms That part of this family which are normal inhabitants of the colon: E. coli Enterobacter Klebsiella Citrobacter So, E.coli is the indicator for fecal contamination of water supply: Coliforms Lactose fermentation, Acid and gas production, growth at 44.5 C and typical colony on EMB. 4 colony count per dL in drinking water is indicative of unacceptable fecal contamination. Antibiotic therapy Must be individually tailored to the antibiotic sensitivity test (Antibiogram). Penicillin and cephalosporin families. Aminoglycosides (Gentamicin, amikacin, kanamycin, streptomycin …), Chloramphenicol, tetracyclines, quinolones and sulfonamides. Laboratory diagnosis Culture for isolation Suspected specimens are inoculated onto 2 media: 1. Blood Agar 2. A selective differential medium (MacConkey’s agar or Eosin-methylene blue, EMB agar. The differential ability is based on lactose fermentation as the most important criterion in identification of these organism. Non lactose fermenters form colorless colonies. Selective effect is exerted by bile salts or bacteriostatic dyes. Laboratory diagnosis (continued) Culture for identification Screening biochemical tests for a final definitive identification: Array of 20 or more biochemical tests to identify the species. Serology Usually in Salmonella, Shigella and E.coli the final detection is by serotyping using agglutination Ag+Ab test. Triple Sugar Iron Agar Almost enough to identify the genus Indicator : Phenol red Components: Iron or Ferrous sulfate FeSO4 (ferrous sulfate) + Solfate reductase SH2 Sodium tiosufate Ferrous sulphide (FeS) Black FeS indicates the production of SH2 3 sugars: glucose (0.1%), lactose (1%), and sucrose (1%) Pepton and yeast extract Different observations for TSI Reactions Slant Button Ga s H2 Representative genera S Acid Acid + - Escherichia, Enterobacter, Klebsiella Alkaline Acid - - Shigella, Serratia Alkalin Acid + + Salmonella, Proteus Alkalin Alkali n - - Pseudomonas Kligler Iron Agar can be used as alternative with two sugers: glucose & lactose Urea Agar Indicator: Phenol red Component : Urea If the bacterium Produces urease: Urea (NH2)2CO is hydrolyzed to NH3 and CO2 light orange changes to reddish purple (in Proteus and K pneumoniae Amonium citrate (Simmons Citrate) Indicator: Bromothymol blue If the bacterium can utilizes ammonium dihydrogen phosphate (a salt of ammonium) and sodium citrate as sole source of nitrogen and carbon, the indicator turns to blue at alkalin pH due to releasing ammonia. Motility SIM medium: SH2, Indole, Motility Proteus: Swarms Differentiation between Enterobacter cloacae (motile) from Klebsiella pneumoniae (Non motile) Indole (in SIM) Tryptophan + Tryptophanase Deamination Intermediate products: Indole + …. Detection: 5 drops Kovac’s reagent (contains paradimethyl-amino-benzaldehyde = PDAB) is added Benzyl pyrol Red ring MR-VP 1. Methyl Red MR-VP medium Components: Glucose, Phosphate After 48 hours Methyl-red (1 droplet to 1 ml of medium) : I. If pH < 4.4 Mixed acidic fermentation (Red color). II. If pH ≥ 5 Butylen glycol fermentation (Yellow color). MR-VP 2. Voges Proskauer Butylen glycol fermentation MR-VP medium: After 24-48 hours Alcoholic alpha naftool (15 droplets to 1 ml medium) + KOH 40% (10 droplets) (may come along cratin) 15-30 min: I. Red (If Acetoin “Acetyl methyl carbynol” exists.) II. No color change (If no Acetoin exist) API 20E system A plastic strips consist of 20 small wells containing dehydrated media components 1. The bacterium is suspended in sterile saline and added to each well. 2. The strip is incubated for 16-24 hours. 3. The colour reactions are noted as either positive or negative. 4. The test results can be entered into a computer programme to identify the bacterium. API 20E system Escherichia coli Diseases 1. Diarrhea or dysentery 2. UTI 3. Sepsis (The most common cause among negative rods) 4. Neonatal meningititis (One of the 2 important agents. The other is the group B streptococci due to colonization of vagina by these organisms in about 25% of pregnant women ). 5. Nosocomial infection UTI Sepsis Neonatal meningititis Virolence factors: Pili Capsule Endotoxin Two exotoxins (enterotoxins). Pathogenesis E. coli attaches to the surface of jejunum and ileum by Pili Bacteria synthesize enterotoxins (exotoxins determined by plasmids) Diarrhea The toxins are strikingly cell-specific. Cells of colon are lack of receptors for the toxins. E. coli pili (fimbriae) mannose galactose glycolipids glycoproteins 43 Most important sub species of pathogenic E. coli Enteropathogenic E. coli (EPEC) Enterotoxigenic E. coli (ETEC) Enteroinvasive E. coli (EIEC) Enterohemorrhagic E. coli (EHEC) Enteropathogenic E. coli (EPEC) destruction of surface microvilli Gut lumen fever diarrhea vomiting nausea non-bloody stools Diarrhea is self-limited and short duration (1-3 days) 45 Enterotoxigenic E. coli Travellers diarrhea Diarrhea like cholera but milder Diarrhea is self-limited and short duration (1-3 days) 46 Enterotoxigenic E. coli (ETEC) Heat labile toxin (LT) like choleragen Activation of Adenylate cyclase Cyclic AMP concentration Secretion water/ions (potassium and chloride) Heat stable toxin (ST) Activation of Guanylate cyclase Cyclic GMP concentration Uptake water/ions (Sodium and Chloride) 47 Enterohemorrhagic E. coli (EHEC) Produce verotoxin which works like Shiga toxin Hemorrhagic bloody, copious diarrhea few leukocytes Hemolytic-uremic syndrome thrombocytopenia (low platelets) hemolytic anemia kidney failure Enterohemorrhagic E. coli Usually O157:H7 Flagella Transmission electron micrograph 49 Enteroinvasive E. coli (EIEC) Very similar to shigella species (in biochemical and morphological traits) Invades to epithelial mucosal cells Cause enteric inflammation Non lactose fermentative Non motile E. coli Transmission By: Meat products or sewage-contaminated vegetables 51 UTI The most common agent for UTI and nosocomial UTI. (Cystitis, pyelonephritis): fever, chills, flank pain Occurs primarily in women Systemic infection Capsule and endotoxin play a prominent role Capsular polysaccharide interferes with phagocytosis (Serotype having K1 causes neonatal meningitis). LPS during sepsis causes fever, hypotension and disseminated intravascular coagulation. Treatment Antibiogram for most infections A combination of ampicillin and gentamicin in neonatal meningitis Rehydration for diarrhea Prevention No passive or active immunization Prompt withdraw of catheters and intravenous lines Caution regarding uncooked food and unpurified water while traveling. Klebsiella Klebsiella ozaenae - Ozena (the atrophy of nose with bad smelling) K. rhinoscleromatis - Rhinoscleroma (A granulomatosis in nose and pharynx) Klebsiella penomoniea - 5% in upper respiratory and GI systems - Nosocomial infection Klebsiella oxytoca - Nosocomial infection Lab detection Large mocoidal colonies. Lac pos. Not motile Proteus P. mirabilis UTI (Alkalic environment in urinary tracts) due to urease kidney stone P. vulgaris Nosocomial infection Shigella Species: S. dysenteriae S. sonnei S. flexeneri S. bouedi There are more than 40 shigella serotypes. Important properties - Non lactose fermenting - Distiguishable from Salmonella by: no gas, no H2S, nonmotile. - Having an enterotoxin called Shiga toxin Shigellosis Only a human disease Transmitted from person to person by asymptomatic carriers (oral-fecal transmission) 4 F’s – fingers, flies, food, feces Food-born outbreaks outnumber water-born outbreaks by 2 to 1. In mental hospitals and day-care nurseries Children <7 accounts for half of shigella positive stool culture Shigella disentery type 1 (Shiga bacillus): - Labile Exotoxin (effective both on intestine and CNS works like verotoxin in E.coli) Pathogenesis Exclusively in gastrointestinal tract Bloody diarrhea (dysentery): Invading the mucosa of the distal ileum and colon. Local inflammation accompanied by ulceration occurs The organisms rarely penetrate the wall or enter the bloodstream unlike salmonellae. Invasion to epithelial cells (M cells) spreading to next cells microabcess formation in the wall of colon and distal ileum necrosis of mocusal layer ulcer bleeding psudomemberane. Clinical findings Incubation period: 1-2 days Symptoms: Fever, abdominal cramps, followed by diarrhea (watery at first but later contains blood and mucus). Mild or severe disease depending: - The species of Shigella - The age of the patient Most invasive species S. dysenteriae causes the most severe disease S. sonnei causes mild disease but more frequent Shiga toxin neurotoxic effects Shiga toxin CNS abnormalities can include lethargy disorientation paralysis coma Neurotoxicity occurs most often in children and the elderly and is often fatal. Clinical findings Resolves in 2-3 days but antibiotic can shorten the course. Serum antibodies appear after recovery but are not protective. Most patients spread bacteria only short time after recovery but few people stay chronic carriers. Most shigellosis cases are in children less than 10 years. Treatment In 50% cases self recovery is in 2-5 days. The main treatment: Fluid and electrolyte replacement. No antibiotic in mild cases Antibiogram test: Trimethoprim - sulfamethoxazole or Ampiciln. Prevention Interruption of fecal-oral transmission by proper sewage disposal, chlorination of water and personal hygiene. No vaccine Antibiotic prophylactic is not recommended. Lab diagnosis Samples: feces, rectal swabs Culture and biochemical tests: Non-lactose fermenter Serology tests: Slide agglutination to detect its species Lab diagnosis Invasive enteric infections: Shigella, Salmonella or Campylobacter Toxin-producing organism: V. cholerae, E. coli, Clostridium perfringens or certain viruses or Entamoeba histolytica Methylene blue stain of a fecal sample to determine whether PMNs are present. Salmonella Important properties Not lactose - fermentive Produce H2S, Gas, motile Salmonella nomenclature Is complicated. Currently there are two recognized species: S. enterica and S. bongori S. enterica has 5 main subspecies. S. enterica enterica is relevant with human infections (specific or zoonotic). Naming the salmonella S. enterica enterica: 1. S. typhi 2. S. paratyphi (A, B, C…) 3. S. typhimurium 4. S. choleraesuis 5. S. enteritidis (1500 serotypes) Diseases Enterocolitis (S. typhimurium & S. enteritidis) Enteric fever (typhoid fever) (S. typhi and S. paratyphi) Septicemia with metastatic abscesses (S. choleraesuis) Diseases Enterocolitis (S. typhimurium & S. enteritidis) An invasion of epithelial and subepithelial tissue of small and large intestines. Penetration both through and between the mucosal cells: Inflammation and diarrhea. PMN response limits the infection to the gut and the adjacent mesenteric lymph nodes. The dose of Salmonella required: at least 105 - 108 while for Shigella: 103 organisms. Clinical findings of Enterocolitis Incubation period: 6-48 hours Symptoms: Nausea, Vomiting, Abdominal pain and diarrhea with or without blood The disease is self-limited. Treatment only in very young and very old. S. Typhimurium & S. enteritidis : the most common cause of enterocolitis. S. typhimurium colonies Typhoid or Enteric fever Typhoid or Enteric fever caused by S. typhi and S. paratyphi (A, B and C). The illness is slow, with fever and constipation rather than vomiting and diarrhea. After the first week, bacteremia becomes sustained. High fever, tender abdomen, and enlarged spleen occur. Typhoid (Enteric fevers) Infection begins in small intestine but few gastrointestinal symptoms occur. The organisms multiply in the mononuclear phagocytes of peyer’s patches, then spread to the phagocytes of the liver, gallbladder and spleen leading to bacteremia and then fever. Typhoid (continued) Rose spot (rose-coloured papules) on the abdomen are associated with typhoid fever but occur only rarely. The disease begins to resolve by the third week but intestinal hemorrage or perforation can occur. 3% of typhoid fever patients become chronic carriers. The carrier rate is higher among women. Septicemia S. choleraesuis: most often cause septicemia. Symptoms: Fever Little or no enterocolitis Focal symptoms: bone, lung, or meninges. Septicemia (S. choleraesuis) Accounts for only about 5-10% of Salmonella infections and occurs: More common in patients with chronic disease or children with enterocolitis. It leads to seeding of many organs commonly: osteomyelitis, pneumonia, and meningitis Typhoid vaccine Two types: Live vaccine Subunit vaccine (a vi capsular polysaccharide vaccine) Transmission of salmonella Ingestion of food and water contaminated by human and animal wastes. S. typhi, transmitted only by humans, but other species have a significant animal reservoir. Human sources: 1. Temporarily excrete the organism during or shortly after enterocolitis 2. Chronic carriers Transmission The most frequent animal source is poultry and eggs, but meat products that are inadequately cooked have been implicated as well. Dogs and other pets including turtles are additional sources. Lab. diagnosis Enterocolitis: isolated from stool Enteric fever: blood culture during first 2 weeks of illness. Septicemia: Blood culture Lab. diagnosis MacConkey, EMB, Hekton Enteric agar, XLD, Endo agar Lactose -, other biochemical tests Gas and H2S (S. type: no gas) Serological tests by their O, H and Vi antigens Serological detection for Ab if culture is negative: Vidal test Treatment Enterocolitis: Self-limited. Fluid and electrolyte replacement. Antimicrobial agents are indicated only for neonates or persons with chronic disease who are at risk of septicemia and disseminated abscesses. Treatment Enteric fever and Septicemia: Ampicillin or chloramphenicol Ampicillin: in patients who are chronic carriers of S. typhi. Cholecystectomy may be necessary to abolish the chronic carrier state. Focal absesses should be drained. Prevention Public health and personal hygiene measures. Proper sewage treatment A chlorinated water supply Cultures of stool samples from food handlers Two vaccine confer protection against S. typhi but no common Proper cooking of poultry and meat Pasteurization of milk Genus: Yersinia Species: Yersinia pestis and Yersinia enterocolitica Small gram negative bacillus, bipolar staining (like a safety pin) Capsule in freshly isolated organism but lost with passage Plague or black death None motile Disease Virulence factors Capsule antigen (F-1) which protects against phagocytosis. Endotoxin Exotoxins (block beta adrenergic receptors) Coagulase Fibrinolysin Pesticin I (a bacteriocin) V antigen protein W antigen protein Pathogenesis Urban cycle Transmission of the bacteria among urban rats with the rat flea as vector to human. This cycle predominates during times of poor sanitation, eg. Wartime, when rats proliferate and come in contact with the fleas in the sylvatic cycle. Sylvatic cycle Humans are accidental hosts and cases of plague occur as a result of being bitten by a flea that is a part of the sylvatic cycle. Event within the flea The flea ingests the bacteria while taking a blood meal from a bacteremic rodent. The blood clots in the flea’s stomach owing to the action of the enzyme coagulase made by the bacteria The bacteria are trapped in the fibrin and proliferate to large numbers. The mass of organisms and fibrin block the proventriculus of the flea’s intestinal tract. During its next blood meal the flea regurgitates the organisms into the next animal Because the proventriculus is blocked, the flea gets no nutrition. becomes hungrier loses its natural host selectivity for rodents more readily bites a human The bacteria inoculated by bite spread to the regional lymph nodes become swollen and tender called buboes and this plague is called bubonic plague. The organisms can reach high concentrations in the blood and disseminate to form abscesses in many organs including lungs. The endotoxin-related symptoms, including disseminated intravascular coagulation and cutaneous hemorrhages, probably were the genesis of the term ‘black death’. Respiratory droplet transmission Respiratory droplet transmission of the organism from patients with pneumonic plague can occur. Clinical findings Bubonic plague, is the most frequent form, begins with pain and swelling of the lymph nodes draining the site of the flea bite and systemic symptoms such as high fever, myalgia, and prostration. The buboes are an early characteristic finding. Septic shock and pneumonia are the main lifethreatening subsequent events. Epidemiology Endemic in the wild rodents of Europe and Asia for thousands of years. 99% of cases of plague occur in Southeast Asia. Enzootic (sylvatic) cycle consists of transmission among wild rodent by fleas. Rodents are relatively resistant to disease. Humans are accidental hosts and cases of plague occur as a result of being bitten by a flea that is a part of the sylvatic cycle. Pneumonic plague can arise either from inhalation of an aerosol or from septic emboli that reach the lung. Untreated bubonic plague is fatal in approximately half of the cases. Untreated pneumonic plague is invariably fatal. Lab. diagnosis The best procedure: Smear and culture of blood or pus from the bubo. Giemsa’s or Wayson’s stain reveals the typical safety-pin appearance of the organism better than does Gram’s stain. Fluorescent-antibody staining can be used to identify the organism in tissues. A rise in antibody titer to the capsule antigen can be useful. Treatment The treatment of choice is a combination of streptomycin and tetracycline. Due to the rapid progression of the disease, treatment should not wait for the results of the bacteriologic culture. Incision and drainage of the buboes are not usually necessary. Prevention Prevention Controlling the spread of rats in urban areas. Preventing rats from entering the country by ship or airplane. Avoiding flea bites Avoiding contact with dead wild rodents. A patient with plague must be placed in strict isolation (quarantine) for 72 hours after antibiotic therapy is started. Only close contacts need to receive prophylactic tetracycline. There is no vaccine for citizens normally. But a killed organism vaccine protecting bubonic but not pneumonic plague was used by USA forces during Vietnam wars. Yersinia enterocolitica Motile: flagella are present at 22 c. No capsule Primarily a zoonotic disease (cattle, deer, pigs, and birds) Yersiniosis : Incubation 1-2 days. Acute Y. enterocolitica infections produce severe diarrhea in humans, along with Peyer's patch necrosis, chronic lymphadenopathy, and hepatic or splenic abscesses. Fever and right-sided abdominal pain. Lab diagnosis Culture: Cold enrichment Culture on blood Sample: Feces Y. pseudotuberculosis Motile: flagella are present at 22 c., No capsule. Culture on blood. Primarily a zoonotic disease (cattle, deer, pigs, and birds). In animals, can cause tuberculosis-like symptoms, including localized tissue necrosis and granulomas in the spleen, liver, and lymph node. In humans, symptoms of Pseudotuberculosis (Yersinia) are similar to those of infection with Yersinia enterocolitica (fever and right-sided abdominal pain), except that the diarrhea is often absent.