1.1 Background information on Shigella
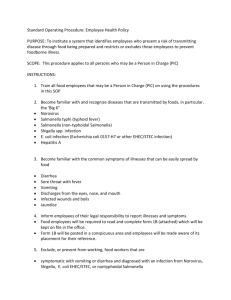
advertisement
UNIVERSITY OF SOUTH AFRICA DEPARTMENT OF LIFE AND CONSUMER SCIENCES SCHOOL OF AGRICULTURE AND LIFE SCIENCES COLLEGE OF AGRICULTURE AND ENVIROMENTAL SCIENCE The burden of shigellosis and antibiotics resistance trends in Richmond area of Johannesburg, South Africa. By: Lawrence John Zulu Submitted in fulfillment of the requirements for the degree of MASTER OF SCIENCE in LIFE SCIENCES at the UNIVERSITY OF SOUTH AFRICA SUPERVISOR: Dr. Monde A. NYILA June, 2014 i Declaration I declare that the study titled “The burden of shigellosis and antibiotics resistance trends in Richmond area of Johannesburg, South Africa” is my original work and that all the sources that I have used or quoted have been indicated and acknowledged by means of complete references. It has not been submitted in any form to any institution of higher learning for the award of any degree. Signature of Student Date ii List of Abbreviations Amp Ampicillin AIDS Acquired Immune Deficiency Syndrome ATCC American Type Culture Collection AUG Augmentin AZM Azithromycin °C Degrees Celsius CDC Centers for Disease Control and Prevention CIP Ciprofloxacin CLSI Clinical and Laboratory Standards Institute CRO Ceftriaxone HIV/AIDS Human Immunodeficiency Virus/ Acquire Immune Deficiency Syndrome MDR Multi Drug Resistance SXT Co-trimoxazole TE Tetracycline WHO World Health Organisation iii TABLE OF CONTENTS PAGE DECLARATION ........................................................................................................................ ii LIST OF ABBREVIATION ..................................................................................................... iii LIST OF FIGURES .................................................................................................................. vii LIST OF TABLES .................................................................................................................. viii ACKNOWLEDGEMENT ........................................................................................................ ix DEDICATION ........................................................................................................................... x ABSTRACT .............................................................................................................................. xi Chapter One .........................................................................................................1 Introduction 1.1 Background information on Shigella .............................................................................. 2 Literature Review ............................................................................................................. 5 1.2 The Genus Shigella .......................................................................................................... 6 1.3 Classification of Shigella ................................................................................................. 7 1.4 The epidemiology of Shigella .......................................................................................... 9 1.5 Growth and survival characteristics of Shigella ............................................................. 12 1.6 Shigella as a water borne pathogen ................................................................................ 14 1.7 Shigella as food borne pathogen .................................................................................... 15 1.8 Transmission of Shigella ................................................................................................ 16 1.9 The disease shigellosis ................................................................................................... 18 1.10 Pathogenicity of Shigella .............................................................................................. 18 1.11 Diagnosis of Shigella ..................................................................................................... 20 1.11.1 Chromogenic media ................................................................................................ 24 1.11.2 VirulenceTest for Shigella………………………………………………………...25 1.11.3 Molecular Techniques ............................................................................................. 25 iv 1.11.4 Immunological Tests……………………………………………………………...26 1.11.5 Enzyme Immune Assay .......................................................................................... 27 1.11.6 Other Laboratory Diagnostic test…………………………………………………28 1.12 Treatment of Shigella ...................................................................................................... 29 1.12.1 Mode of Drug Resistance of Shigella ..................................................................... 31 1.13 Shigellosis and HIV/AIDS ............................................................................................. 34 1.14 Prevention management of Shigella infection .............................................................. 35 1.15 Problem statement .......................................................................................................... 36 1.16 Objectives of the study ................................................................................................... 37 1.6.1 Main objective .............................................................................................................. 37 1.6.2 Specific objective .......................................................................................................... 37 1.16.3 Significance of the study............................................................................................. 37 Chapter Two ........................................................................................................................ 38 Materials and Methods Material and Methods..................................................................................................... 39 2.1 Study Laboratory ............................................................................................................ 39 2.2 Experimental design ....................................................................................................... 39 2.3 Sample area (Johannesburg)........................................................................................... 39 2.4 Sampling, handling and transport of specimen .............................................................. 40 2.5 Ethical considerations ................................................................................................... 40 2.6 Microbiological Culture ................................................................................................. 41 2.7 Characterisation of Shigella ........................................................................................... 41 2.7.1 McFarland Turbidity Testing ......................................................................... 41 2.7.2 VITEK 2 system ID-GNB card...................................................................... 43 2.7.3 The API 20E .................................................................................................. 46 2.7.4 Serological assays .......................................................................................... 47 v 2.8 Antimicrobial susceptibility testing ................................................................................. 48 2.8.1 Detection of extended-spectrum β-lactamase ................................................ 48 2.9 Statistical analysis ............................................................................................................ 49 Chapter Three ....................................................................................................50 The Results The Results........................................................................................................................... 51 3.1 Colonies.......................................................................................................................... 51 3.2 Serological results .......................................................................................................... 52 3.3 Isolates and species distribution ..................................................................................... 52 3.5 Susceptibility Test Results ................................................................................................. 55 Chapter Four ..........................................................................................................57 Discussion Discussion ........................................................................................................................... 58 4.1 Prevalence ...................................................................................................................... 58 4.2 Conclusion...................................................................................................................... 60 4.3 Limitation ....................................................................................................................... 61 4.4 Recommendation ............................................................................................................ 61 Chapter Five .............................................................................................................63 References 5.0 References ..........................................................................................................64 Appendix .....................................................................................................................79 6.1 Appendix I ..........................................................................................................80 6.1.1 Publication and Conference Presentation ......................................................80 6.2 Appendix II ...........................................................................................................81 6.1.1 Lancet Laboratories Ethics Approval .......................................................81 6.1.2 University of South Africa Ethics Approval.............................................81 vi LIST OF FIGURE FIGURE PAGE 2.1 Faecal sample in standard stool container ....................................................................... 41 2.2 The DensiCheck Plus equipment (BioMérieux, France) .................................................. 42 2.3 The grey carrier container and ID-GNB card (BioMérieux, France). .............................. 45 2.4 API 20E strip .................................................................................................................... 47 3.1 Non-lactose fermenting colonies on MacConkey Agar plate (A) and reddish (B) colonies on XLD (B) ...................................................................................................................... 51 3.2 Model basis of antigen-antibody reaction (A) and Slide agglutination test results (B) .. 52 3.3 Monthly isolates distribution during the month of study .....……………………………..54 3.4 Disc diffusion result……..…………………………………………………………….…55 vii LIST OF TABLES TABLES PAGES 1.1 Global incidences of shigellosis........................................................................................ 11 1.2 Species, serogroups and geographic distribution of Shigella ............................................ 11 1.3 Selected food and water borne outbreaks involving Shigella ............................................ 14 1.4 Biochemical substrates for characterising Shigella ......................................................... 23 3.1 Monthly and gender infection distribution of Shigella serogroups isolated from human stool specimens from January to April 2013 ................................................................. 53 3.2 Distribution of Shigellosis cases according to age-group ………….……………………54 3.3 Antimicrobial resistance test results for Shigella strains .................................................. 56 3.4 Monthly distributions of antibiotic resistant Shigella strains ………………………..…..56 viii ACKNOWLEDGEMENTS “Many discouraging hours will arise before the rainbow of accomplished goals will appear on the horizon.” King Haile Sellassie. I would like to acknowledge all who were around through my discouraging hours and my rainbow of achievements especially: My heads of Microbiology Laboratory, Dr H.T. Booker and Dr J. Smit who allowed the use of the facilities. My manager, Mrs Sharee Bezuidenhout for helping me find necessary direction in the Laboratory. The Publication Committee of Lancet Laboratories for granting permission for this work to be undertaken. All colleagues who wittingly and unwittingly contributed to this research project. Utmost appreciation and lifelong thank you go to my supervisor Dr Monde A. Nyila for professional advice, support and encouragement throughout this work, without him this would not have been a success. I am indebted to all microbiology staff that encouraged me to reach for my dreams. My greatest appreciation goes to my sons, Dalubuhle, Thabiso, Mxolisi and Manqoba, my wife, Ntombi maZulu, for your undying love, support and sacrifice. Prof. Leslie A. Greyveenstein for the English language editing. Finally, to almighty God for blessing me with endurance to stand steadfast during the many discouraging hours. ix Dedication This dissertation is dedicated to: My late father and mother, Mr John P. Zulu and Mrs Monica Zulu, for their strong belief in education and encouragement to seek education at any age. My sons Dalubuhle, Thabiso, Mxolisi and Manqoba. I hope this inspires you to reach the summit in all you undertakings. All who believe in the richness of learning. x Abstract Diarrhoea, particularly infectious diarrhoea, in children below five years of age is recognised as one of the leading cause of morbidity and mortality throughout the world. This is especially true in residential areas of developing countries where there is substandard sanitation and overcrowding which are reservoirs for farther transmission. Shigellosis is endemic in developing countries and in Sub-Saharan Africa, including South Africa, a region where unique geographic, economic, political, sociocultural, and personal factors interact to create distinctive continuing challenges to prevention and control. Our study was undertaken to establish baseline information on incidences of Shigella, its serotype and resistant pattern of isolates from human faeces from residents of Johannesburg, South Africa. All stools received from January to April 2013 from the private health care system were cultured on standard media for isolation of Shigella and confirmed by standard biochemical reactions and serological method. Antibiotic sensitivity test was determined by the agar diffusion method. 11009 stool samples were assayed from patients aged between 22 days to 94 years with a 110 Shigella isolates yield, of which 47 (43%) were S. flexneri, 61 (55%) S. sonnei and 1 (1%) of S. dysentriae and S. boydii respectively. Majority of patients 76 (69%) were children between < 1 to 5 years old followed by those between 6 to 10 years 13(12%). Of the four species isolated from children of up to 10 years old, S. sonnie was confirmed in 52 cases (59%) and S. flexneri in 36 cases (41%). A total of 53 (48%) males and 57 (52%) females were infected. However, a hundred per cent susceptibility to ciprofloxacin and ceftriaxone but high levels of resistance to Co-trimoxazole (83%), tetracycline (72%), and ampicillin (26%) was noted. From the 110 isolates, 96 (87%) were resistant to one or more drugs while 14 (13%) were fully susceptible. These results show that S. sonnei followed by S. flexneri as predominating aetiology of shigellosis and Ceftriaxone and ciprofloxacin as effective drugs against all four Shigella species. xi CHAPTER ONE Introduction 1 Chapter One Introduction 1.1 Background information on Shigella Diarrhoeal disease, particularly infectious diarrhoea, is a major cause of morbidity and mortality particularly in young children, the elderly and immune compromised and/ or HIV/AIDS individuals (Mandomando et al., 2007). The World Health Organisation (WHO) (2009) defines diarrhoea to be the passage of three or more loose or liquid stools per day. This results from defective fluid and electrolyte transport in the intestine. Absorption and secretion of water and electrolytes occur throughout the intestine. Normally absorption is greater than secretion, therefore, only a small amount of fluid is excreted each day in formed stools. However, when there is increased secretion, decreased absorption or both then a reduction in net absorption follows and an increased volume of fluid enters the large intestine. This anal excretion of excessive fluid is known as diarrhoea (Hodges and Gill, 2010). Two forms of diarrhoea are known. The osmotic diarrhoea results from the flow of fluid from the lumen to maintain osmotic balance between the bowel contents and the blood while secretory diarrhoea is the abnormal secretion of fluid into the small bowel. This occurs when absorption by the villi is impaired while the secretion in the crypts continues or is increased. In infectious diarrhoea, reduced absorption and increased secretion may result from damage of the villi (bowel mucosa) or inflammation (colitis or gastroenteritis) from toxins, bacterial, viral, fungi and parasitic organism’s actions. Shigellosis is the infectious diarrhoea caused by the infection with bacteria of the genus Shigella (WHO, 2009; CIDAAP, 2009; Hodges and Gill, 2010; CDC, 2013). The WHO estimates 165 million diarrhoeal cases occur each year globally of which 163 million cases occur in developing countries. About 1.1 million deaths occur each year with the highest incidences in children less than 5 years of age (WHO, 2009). Shigellosis is an infectious diarrhoeal disease that continues to be a major public health concern. About 125 million cases of Shigella infection occur annually in Asia, of which about 14 000 are fatal (Bardhan et al., 2010). Many African countries are infested with shigellosis with fatality reported in Rwanda, Central African Republic, Sierra Leone, Lesotho, Liberia and Sudan 2 (Opintan and Newman, 2007; Asrat, 2008; Keddy et al., 2010; Efuntoye and Adenuga, 2011; WHO, 2012). Shigella serogroups distribution may differ from country to country and within a region but exacerbated by its low infectious dose of 10 to 100 bacteria plus the ease with which person to person and faecal-oral transmission occurs makes it a potential biological weapon tool worthy of monitoring (WHO, 2009). Shigellosis is one of the acute enteric diseases for which antibiotic treatment is required to manage infection and eradicate faecal excretion of bacteria thus preventing further disease transmission. The bacterium’s progressive acquisition of resistance to widely-used antimicrobials (Mamatha et al., 2007; Pazhani et al., 2008; WHO, 2012) makes infection management difficult. The disease is associated with grouping of people such as day care centres, primary schools, military barracks (WHO, 2012) but due to faecal contamination of environment, flies (Ugbogu et al., 2006), water (Wose and Mbewe, 2010), food and kitchen towels (Castillo et al., 2006) and men having sex with other men (Daskalakis and Blaser, 2007) makes vulnerability to infection to reach wider boundaries and is not limited to crowded and impoverish communities. UNAIDS (2012) reported 34.2 million people worldwide living with HIV in 2011, two-thirds (69 %) of these were in Sub-Saharan Africa. About 3.2 million (91%) children in Sub-Saharan lived with HIV in 2011. HIV infection is, therefore, an important risk factor for Shigella infection. Its association with shigellosis may lead to extensive illness, Shigella septicaemia increases fatality rate and increases health-care expenditures particularly in South Africa (Obi et al., 2007; Keddy et al., 2012). Laboratory-based surveillance of food, water, human and environmental specimens provides crucial information about pathogen trends. Healthcare or pathology and food-water laboratories routinely assay samples for enteric and other pathogens and electronically store data for many years. In pathology laboratories, routine antibiotic susceptibility testing offers additional valuable guidance to clinicians as to therapy management of patients. The data gathered through routine work can be useful for surveillance to identify trends in isolates, serotypes, antibiotic susceptibility/resistance patterns and infested areas (Gupta and Polyak, 2004). In the United States of America, Shigella surveillance systems are active in all its states to report on notifiable pathogens such as Shigella and avail valuable information on its infection foci and drug 3 susceptibility (CDC, 2013). The contagious micro-organism surveillance system in South Africa places an emphasis on the public health care sectors while it is optional in the private sector laboratory (Brink et al., 2007). Effective laboratory-based surveillance may enhance early outbreak detection and also allow a constantly updated epidemiological and disease burden database on diarrhoeal diseases, particularly for shigellosis. South African shigellosis data may aid in evaluating disease patterns and determining whether these follow global trends or whether they have their own unique evolutionary profile. Studies show tropical, Sub-Sahara and subtropical parts of the world to be where living standards are low with access to safe drinking water and proper excreta disposal systems often limited and, therefore, are focal areas of disease (WHO, 2009). The World Health Organisation reports show up to 80% of diarrhoeal episodes in travellers to be bacterial in nature and are caused principally by enterotoxigenic Escherichia coli (ETEC) strains and quite commonly, by Shigella, Campylobacter and Salmonella species (WHO, 2005). South Africa geographically lies in subtropical and Sub-Sahara region where it faces unique economic, political, socio-cultural and personal factors that interact to create distinctive continuous challenges that impede control and prevention of shigellosis. Laboratory confirmed isolates have been reported in outbreaks in Delmas, a town 40 kilometres east of Johannesburg, in 1993, 2005 and 2007 (Moselakgomo, 2007; Nealer et al., 2009) and on 25th April 2012, the Paul Jungnickel Rehabilitation Centre in Tshwane/ Pretoria three deaths from 140 habitants were reported (Makhubu, 2012) and in 1994 in KwaZulu Natal (Pillay et al., 1997). Shigella has also been isolated from surface waters (Wose and Mbewe, 2010). Johannesburg, South Africa’s largest city is situated in the country’s most populous province, Gauteng. As the financial and manufacturing centre of South Africa, the city offers employment to people within South Africa, Southern Africa, the rest of Africa, as well as from overseas. Tourism functionalities of the city and being a gateway route to within South Africa and abroad, offer additional reason(s) for movement of people. 4 LITERATURE REVIEW 5 Literature review 1.2 The Genus Shigella Shigella was discovered in 1896 by a Japanese scientist, Dr Kiyoshi Shiga as bacteria causing dysentery in humans and primates (Niyogi, 2005; CDC, 2013). Shigella flexneri was described by Dr Simon Flexner in 1900. Shigella boydii was first isolated in India 1931 and was described by American bacteriologist and epidemiologist, Mark Frederick Boyd while Shigella sonnei was first isolated in 1904, but it was in 1915 that its pathogenicity was recognized by Dr Carl Olaf Sonne (Cheesbrough, 2006; Washington et al., 2006; Todar, 2010) and it was in 1950 that the Congress of the International Association of Microbiologists Shigella Commission adopted as the generic name Shigella and that species subgroups be designated A (Shigella dysenteriae), B (S. flexneri), C (S. boydii) and D (S. sonnei) (Hale, 1991). Based on 16S rRNA sequencing, Shigella is from gamma proteobacteria in the family Enterobacteriaceae phylum Proteobacteria (Cheesbrough, 2006; Washington et al., 2006) and is gram-negative, non-spore forming, nonpigmented rod-shaped bacteria. The rod is 2.0-6.0 μm in length and 1.1.-1.5 μm in width with round ends (Cheesbrough, 2006; Washington et al., 2006). Catalase positive (with exceptions in Shigella dysenteriae), oxidase negative, ferments sugars without gas production (a few exceptions produce gas), salicin, adonitol, and myo-inositol are not fermented. Strains of Shigella sonnei ferment lactose and sucrose on longer incubation, however, other species do not utilize these substances in conventional medium. Shigella does not utilize citrate, malonate, or sodium acetate (with exceptions in Shigella flexneri form sodium acetate) as a sole carbon source nor does it grow in KCN (potassium cyanide) or produce H2S. It reduces nitrates to nitrites (Cheesbrough, 2006; Washington et al., 2006). Phylogenetically studies relate Shigella and Escherichia coli to be very close (Lan and Reeves, 2006; Hao et al., 2012). In contrast to Escherichia coli, Shigella is non-motile, generally nonlactose fermenting, no gas from glucose and does not decarboxylate lysine or hydrolyse argininie. They do not liquefy gelatin but are facultative anaerobic and chemo-organotrophic that have both respiratory and fermentative type of metabolism (Zafar et al., 2005; Washington et al., 2006). The serogroups of the genus Shigella with a total of 46 serotypes (Li et al., 2009) are highly adapted to humans and primates, the only known natural hosts, and are grouped among 6 enteric pathogens that can cause acute and bacillary dysentery only in man and apes (CDC, 2013). 1.3 Classification of Shigella The International Committee on Systematics of Prokaryotes (formerly the International Committee on Systematic Bacteriology) set the hierarchy of bacteria based on the carbohydrate composition of their (somatic) O-antigen, the polysaccharide part of the lipopolysaccharide (LPS), the major bacterial surface antigen and biochemical analysis. Shigella has been classified into four subgroups. Serotypes are further divided into sub-serotypes based on their possession of group factors. Subgroups are classified using letters of the English alphabet and serotypes use a combination of numbers and letters of the English alphabet system as follows: Subgroup A: S. dysenteriae contains 13 distinct antigenic serotypes, subgroup B: S. flexneri (14 serotypes), subgroup C: S. boydii (18 serotypes) and subgroup D: S. sonnei (1 serotype). Groups A, B and C are physiologically similar but the S. sonnei (group D) can be differentiated on the basis of biochemical metabolism assays (Niyogi, 2005; Washington et al., 2006; Todar, 2010). Antigenic characterisation relies exclusively on their somatic (O) antigens because they produce neither flagellins (H) nor capsular antigens (K). Biosynthesis of the O antigen is carried out by genes located in the galF and gnd clusters. These genes are classified into three different groups being genes for the synthesis of nucleotide sugars specially used as O antigen residues, genes encoding sugar transferases and O unit processing genes normally consisting of O unit flippase gene (wzx) and polymerase gene (wzy). Based on their antigenic properties, about 46 Shigella serotypes have been recognized. Serotyping of Shigella strains is only based on their distinct O antigens (Tao et al., 2004; Niyogi, 2005; Zafar et al., 2005; Li et al., 2009; Todar, 2010). According to Peng et al. (2006), molecular analysis of the gene for DNA gyrase B (gyrB) and 16S rRNA established a phylogenetic tree in which other bacteria such as Salmonella forms a separate cluster from closely related Shigella and Escherichia coli (E. coli). Other phylogenetic studies indicate that Shigella is more appropriately treated as subgenus of Escherichia and that certain strains generally considered E. coli such as E. coli O157:H7 are better placed in Shigella 7 (Lan and Reeves, 2002). Also according to Lan and Reeves (2002), studies using multilocus enzyme electrophoresis (MLEE), ribotyping and a combination of MLEE and sequence of the mdh gene have elucidated the evolutionary relationships of all 46 serotypes of Shigella showing that most serotypes fall into three clusters within E. coli. All clusters include strains from different subgroups and each represents a very successful pathogenic E. coli clone that has developed some biochemical and substantial antigenic diversity. The genus Shigella, therefore, belongs to the family Enterobacteriaceae. Among the significant pathogenic genera of the Enterobacteriaceae family are Escherichia, Enterobacter, Klebsiella, Proteus, Providentia and Salmonella while other members include Arizona, Citrobacter, Edwardsiella, Erwinia, Hafnia, Serratia, and Yersinia (Cheesbrough, 2006). Cheesbrough (2006) and Washington et al. (2006) describe the taxonomy of Shigella to be as follows: Shigella fits into the Kingdom Bacteria (Eubacteria) because members of this group are unicellular, do not possess a nucleus and have peptidoglycan in their cell walls. They belong to the phylum Proteobacteria because they are gram-negative with the outer membrane is mainly composed of lipopolysaccharides. Shigella is classified in the class Gamma Proteobacteria because it is comprised of facultative anaerobic and fermentative gram negative bacteria, with the order of Enterobacteriales because it is comprised of rod-shaped, facultative anaerobic, gram negative bacteria occurring as plant or animal parasites or as saprophytes. It fits into the family Enterobacteriaceae because members of this group grow well at 37 degrees Celsius, oxidase negative, catalase positive and reduces nitrates. It belongs to the genus Shigella because it causes disease in primates and no other animals. The species classification is based on biochemical metabolism assays such as positive β-D galactosidase and ornithine decarboxylase biochemical reactions for which only Shigella sonnei is positive. 8 1.4 The Epidemiology of Shigella Shigella is highly adapted to human as the only known natural hosts and incidences of shigellosis have been reported worldwide. According to Ram et al. (2008), the average world annual incidences are estimated to be 80-165 million cases with 99% occurring in developing countries. About 1.1 million people die from Shigella infection each year of which 60% occur in children below 5 years of age. In endemic areas of the developing world, shigellosis is predominantly a paediatric disease (Mandomando et al., 2007; CIDAAP, 2009; Le Faou, 2010). The urban impoverished communities globally are hardest hit due to overcrowding, substandard sanitation, hygiene and lack of clean water. Institutions such as day-care centres, prisoners, military recruits and travellers are especially at high risk. Shigellosis has also be demographical classified according to the new sexual habits population concentration of men who have sex with other men (WHO, 2009). In developed countries shigellosis occurs erratically as outbreaks, while in developing countries reported incidences are probably 20 times more than in developed countries, yet a significant number of cases go unreported (CDC, 2009; WHO 2009). Global disease rates increase somewhat occur during summer, rainy season and shortly thereafter especially in tropical regions (WHO, 2009). Perhaps due to increased water run-off therefore faecal contamination of (drinking) water and crops. Also period of swarming flies has contributed to the incidences of shigellosis (Farag et al., 2013). Surveillance system networks of the CDC (2009) estimated global annual incidences as follows; in 1978 to 2003, about 17,000 cases, about 14,000 cases in 2004 and about 20,000 in 2007. However, it is suspected that a significant number of shigellosis cases exist in each country globally. South Africa (CDC. 2012) has the highest laboratory confirmed Shigella cases in Sub-Sahara Africa. The geographical distribution and predominant serogroup of Shigella circulating in a community appears to be related to the level of socioeconomic development. Attempts have been made to summarize published studies which enumerate the proportion of isolates from hospitalized patients, presumed to be the most severe cases, throughout the world, recognizing that 9 considerable difference exists among studies. S. flexneri is the main serogroup found in developing countries (median 60% of isolates), with S. sonnei being the next most common (median 15%). S. dysenteriae has high incidences in Asia and Sub-Saharan Africa and S. boydii occurs commonest in India (Kotloff et al., 1999b). The Tiruneh (2009) study in Ethiopia reflects serotype distribution of S. flexneri 72.2%, S. dysenteriae 10%, S. boydii 8.9% and S. sonnei 8.9%. In contrast, studies from Europe, Israel, Spain, and the United States demonstrate that S. sonnei is the most common serogroup found in industrialized countries (median 77%), followed by S. flexneri (median 16%), S. boydii (median 2%) and S. dysenteriae (median 1%) (Kotloff et al., 1999b). A study conducted in Belgium during the period 1990 to 2007, from 7307 strains of Shigella species isolated, 4951 were serotyped as S. sonnei (67.8%), 1856 as S. flexneri (25.4%), 244 as S. boydii (3.3%), and 163 as S. dysenteriae (2.2%). A total of 72 isolates (1%) were nonagglutinable but were biochemically confirmed as Shigella species (Vrints et al., 2009). The wide variations in these distributions together with the rather limited number of countries for which serotype distributions have been studied call for the need for more studies on this topic. S. dysenteriae type1 (Sd1) causes endemic or epidemic dysentery with high death rates. It is the most common cause of large-scale, regional outbreaks of dysentery. S. dysenteriae type1 has caused epidemic dysentery in Central America, Asia and Central and Southern Africa (WHO, 2012). The epidemic in Central America from 1969 to 1973 had more than 500,000 cases and 20,000 deaths. Central and Southern Africa began in 1979 and it affected eastern Zaire (Democratic Republic of Congo, now), Rwanda and Burundi. In the 1990s, epidemic dysentery spread southward, affecting Zambia, Malawi, Mozambique, Zimbabwe and Lesotho. An increase in mortality cases was associated with refugee camps seen in central Africa in 1994 (WHO, 2012). Of the nomadic diarrhoea, studies have shown that Shigella is one of the important pathogen causing traveller’s diarrhoea (Drews, et al., 2010). The Table 1.1 attempts to condense laboratory confirmed cases. 10 Table 1.1 1999 Global Incidences of Shigellosis Region Extrapolated Incidence Population Estimated Used (number of cases) 526 8,174,762 18,915 293,655,405 2,094 32,507,874 83,665 1,298,847,624 3,882 60,270,708 5,309 82,424,609 68,606 1,065,070,607 10,254 159,196,336 1,337 20,757,032 1,143 12,5750,356 4,595 71,336,571 707 10,978,552 105 1,639,231 2,863 44,448,470 710 11,025,690 75 1,169,241 236 1,2671,860 Austria USA Canada China United Kingdom Germany India Pakistan Ghana Nigeria Ethiopia Angola Botswana South Africa Zambia Swaziland Zimbabwe Source: CDC, 2012 Despite being endemic and for unclear reasons, the four species and serotypes of Shigella have different geographical dominance (Table 1.2). Table 1.2 Species, Serogroups and Geographic distribution of Shigella Organism Serogroup S. dysentariae S. flexneri S. boydii S. sonnei A B C D Number Serotypes 13 14 18 1 of Geographic location Epidemic outbreaks Developing world Limited foci in India U.S. and other industrialized countries Source: Source: BIO Ventures for Global Health (2011). Three species are the major disease-causing, namely, S. flexneri, the most frequently isolated species worldwide and accounts for 60% of cases in the developing countries, S. sonnei causes 11 77% of cases in the developed world as compared to 15% of cases in the developing countries while S. dysenteriae causes epidemics of dysentery particularly in confined populations like camps or schools (WHO, 2009). The WHO (2012) estimates a yearly occurrence of 450, 000 cases of shigellosis in Unites States of America with 72% of the cases caused by S. sonnei while S. dysenteriae type 1 infection has 5-15% fatality rates in Africa and Central America. S. dysenteriae type 1 is believed to account for all major outbreaks in Africa’s Sierra Leone, Central African Republic, Liberia and Sudan. However, Shigella species have also been isolated in economical richer Africa countries such as Ghana (Opintan and Newman, 2007), Nigeria (Efuntoye and Adenuga, 2011), Ethiopia (Asrat, 2008) and South Africa (Keddy et al., 2010), perhaps with less fatality. The reports of African isolates differ from general geographic distribution by showing the presence of all species sometimes in the same region. 1.5 Growth and survival characteristics of Shigella Despite public health significance of Shigella, its presence and persistence in the environment is less documented. The growth and survival of Shigella species is influenced by a number of factors such as temperature, pH, salt content and the presence of bactericidal agents. For example, survival of S. flexneri has been shown to increase with decreasing temperature, increasing pH and decreasing sodium chloride concentration (Zaika and Phillips, 2005). Warren et al. (2006) has reported survival of Shigella under frozen (-20°C) or refrigerated (4-8 °C) conditions. Shigella species grow in a pH range of 5–9 (Zaika and Phillips, 2005). Zaika (2001) demonstrated that S. flexneri is tolerant to acid and can survive at pH 4 for 5 days in broth when incubated at 28°C while survival at lower pH conditions at reduced temperatures was demonstrated with S. flexneri and S. sonnei being able to survive for 14 days in tomato juice (pH 3.9–4.1) and apple juice (pH 3.3–3.4) stored at 7°C (Bagamboula et al., 2002). Shigella species have also been shown to survive on various surfaces. S. sonnei has been isolated from fingers (skin) several hours after hand contamination (WHO, 2008). A study by Nakamura (1962) reported S. sonnei being able to survive on cotton, glass, wood, paper and metal with survival times ranging from 2 days on metal to 28 days on paper at 15 °C. S. dysenteriae serotype 1 has also been shown to survive on surfaces including plastic, glass, aluminium, wood and cloth 12 (Islam et al., 2001). S. flexneri is salt tolerant and is able to grow in media containing 7% Sodium Chloride at 28°C (Zaika, 2002a). Shigella also has capabilities to survive in river (Wose and Mbewe, 2010) and clean (CDC, 2012) water and also adopts a viable but non-culturable (VBNC) state when exposed to various hostile environmental conditions. The VBNC cells survive in a dormant state while culturable cells die (Islam et al., 2001; Nicolo et al., 2011). Molecular studies have also enhanced the human understanding of bacteria survival, including Shigella. Bacteria survival strategies are imbedded in their genome and are expressed according to the bacteria survival needs governed by the surface on which they settle. Since genome consists of core and accessory genomes of which the core genome contains all genes vital to cell survival, such as genes encoding molecules involved in metabolism, DNA and RNA synthesis and replication, whereas the accessory gene pool represents the diversity within bacterial species by encoding proteins required for adaptation of bacteria in different ecological niches (RoweMagnus et al., 2002; Zhang and Lin, 2012). Some investigators described mobile genetic elements (MGEs) as being involved in survival. MGEs are fragments of DNA that encode a variety of virulence and resistance factors, as well as the enzymes that mediate their own transfer and integration into new host DNA. MGEs may consist of insertion sequences, transposons, phages, plasmids, pathogenicity islands, and chromosome cassettes that facilitate horizontal gene transfer occurring between prokaryote-to-prokaryote, prokaryote-to-eukaryote, and or eukaryoteto-eukaryote with vertical gene spread of transmission of genetic information from parent to progeny cell (Rowe-Magnus et al., 2002; Domingues et al., 2012). Genes carried on 180 to 240 kb plasmids are responsible for full expression of virulence (Hale, 1991). Virulence determinants affect the ability of Shigella to survive in the intestinal tissues. For example, the aerobactin siderophore (iucABCD and iutA), superoxide dismutase (sodB) and somatic antigen expression (rfa and rfb) and cytotoxins, such as Shiga toxin (stx), contribute to the severity of disease while other plasmid genes, for example, ompR-envZ mediate response to changes in osmolarity and virR (osmZ) mediates response to changes in temperature (Hale, 1991; Schroeder and Hilbi, 2008). Clearly virulence in Shigella is dependent on its genetic expression. 13 1.6 Shigella as water borne pathogen The presence of disease-causing enteric microorganisms such as Shigella in tap water typically results from poor water quality at source, lapses in disinfection and filtration treatment processes or compromised distribution systems. Bacteria and viruses have the capability to contaminate both surface and groundwater. In developing countries contamination of water typically occurs if the toilets or defecation sites are near wells, sewage pipes or systems are broken and or feed directly into lakes that feed these wells and water sources. Waterborne epidemics also originate from the contamination of surface waters used for recreational purposes. Bacterial pathogens commonly implicated include Salmonella, Shigella, Campylobacter, Vibrio cholera, enterovirulent Escherichia coli, Aeromonas, Yersinia and Clostridium perfringens, while viruses such as the enteroviruses, rotaviruses, parvoviruses, adenoviruses, caliciviruses and astroviruses are major concerns (WHO, 2005; Cheesbrough, 2006; Washington et al., 2006). Table 2.3 attempts to condense research that show Shigella and water or food source association. Table 1.3 Selected food and water borne outbreaks involving Shigella Year Serogroup Food or product Reference implicated 2002 Shigella species Greek-style pasta salad TPH, 2002 2007 S. dysenteraie type 1 and ready-to-eat salads, Ghosha et al., 2007 S. flexneri 2a coconut slices, coriander sauce 2009 Shigella sonnei Sugar peas Heier et al., 2009 2010 Shigella species raw meat Hassan Ali et al., 2010 2010 Shigella species water Wose and Mbewe, 2010 2011 Shigella sonnei water Godoy et al., 2011 2012 Shigella flexneri water He et al., 2012 14 1.7 Shigella as food borne pathogen. Changes in eating habits, mass catering, complex and lengthy food supply processes and poor hygiene practices are major contributing factors to food and food products contamination with bacteria. Food has a complex chemically matrix that supports the bacterial growth. Numerous factors encourage, prevent or limit the growth of microorganisms in foods and the most important include pH, energy source factors and temperature. Bacteria require energy sources that include organic carbon, nitrogen, phosphorus, sulphur and metal ions, including iron. These growth supporting elements are essential to human and are commonly found in their food (Cheesbrough, 2006; Washington et al., 2006). Food provides necessary growth nutrients for bacteria to multiple in number and/or produce toxin in food to cause food poisoning. It is common for clinicians or epidemiologists to suspect food poisoning as a primary cause in case of sudden onset of disease in a well-defined community after consuming the same food. Symptoms caused by different food poisoning microbes include nausea, vomiting and diarrhoea and their specific aetiology is diagnosed by traditional methods of bacteriological culture. Common food contaminating bacteria include Shigella, Salmonella, Staphylococcus aureus, Yersinia enterocolitica, Clostridium perfringens and Clostridium botulinum (Cheesbrough, 2006; Washington et al., 2006). Little published surveillance data on the presence of Shigella in food exists in South Africa. However, Shigella species have been found in many foods elsewhere. For example, Ghosha et al. (2007) have isolated Shigella from coconut slices, ready-to-eat salads and coriander sauces from Indian street vendors in Pakistan and Hassan et al. (2010) demonstrated Shigella species in raw meat from retail outlets. In Mexico, Shigella species have been isolated from freshly squeezed orange juice samples, oranges sampled and wiping cloth (Castillo et al., 2006). While FoodNet studies have demonstrated associations between illness and consumption of foods such as undercooked ground beef, chicken and eggs while some outbreak investigations have identified novel food and non-food vehicles such as jalapeno peppers these findings are also common for shigellosis (CDC, 2010). 15 Clearly Shigella is isolatable from a vast number of foods mainly those that involve much hand contact in their preparation, whereas vegetables contamination occurring in the field is presumably from faecal containing runoff water and faecal use as manure. In order to develop tangible control measures that will address transmission of shigellosis, food consumption patterns of specific communities and food industry processing methodologies must be understood. Table 1.3 above attempts to condense research incidences involving Shigella as a foodborne pathogen have been made. 1.8 Transmission of Shigella Water is essential to life, however, faecal contaminated water is a vehicle of bacterial, viral and parasitic pathogens. Shigella infection is often acquired through drinking faecal contaminated water and/or by eating food/vegetables washed in contaminated water (Cabral, 2010; CDC, 2010; Jiménez et al., 2010). Survival of Shigella in water (WHO, 2008; Wose and Mbewe, 2010) and in foods (Warren et al., 2006) is a significant mode of transmission especially in developing countries where inadequate sanitation mostly prevails. Food-borne infections occur worldwide though mostly occur in developing rather than developed countries (CDC, 2013) because of discrepancy in sanitation adequacy. In addition to faecal contamination by food handlers with poor hygiene, flies have proved to be important vectors (Ugbogu et al., 2006; Farag et al., 2013) in sanitary poor environment. Shigella infections can also be acquired through contaminated kitchen towels, ingesting faecal contaminated swimming pool water and “coitus” between men (Castillo et al., 2006; Daskalakis and Blaser, 2007), the most vulnerable to Shigella infection are toddlers/children especially in day care centres due to their behavioural habits that promote person to person transmission and acquisition from fomite (CDC, 2013). Even in meticulous adult, Shigella infection has been reported supposedly transmitted through poor hygiene. For example, Singh (2009) reported Shigella as one of the commonly laboratory acquired infections despite the meticulous nature of laboratory workers. From the USA microbiology laboratories 15 cases were reported in 2002 to 2004. Natural disasters and wars are associated with shigellosis. This is because encampments creates overcrowding, encourages sharing or consumption of water and food from the same utensil, and 16 direct personal contact. The reductions of facilities invariably impact on optimal hygiene conditions and, therefore, create perfect breeding places. The fatalities experienced in Rwanda during the 1994 genocide (WHO, 2012) is an example. About 20 000 Rwandan refugees who fled genocide into a camp in the North Kivu region of Zaire died in the first month from dysentery caused by a strain of Shigella that was resistant to all commonly used antibiotics (WHO, 2012). WHO (2009) advocated the source of Shigella infection to be chiefly from excreta (stool) of infected individuals or convalescent carries. Carriers are of particular concern because of lack of symptoms. Food handlers in domestic and commercial settings are an insidious source. Presence and/or isolation of pathogens such as Shigella in freshly squeezed orange juice, fresh oranges and wiping cloth (Castillo et al., 2006) and in lettuce (Jiménez et al., 2010) are typical examples of food handlers’ involvement in transmitting Shigella. Adaptability of the bacteria to hostile conditions and loss of cultivability in some media such as grapefruit juice yet viable on suitable resuscitating media (Nicolo et al., 2011) could be significant in transmission of shigellosis. Seasonal prevalence of shigellosis in tropical areas has not only been enhanced by faecal contamination water sources caused by water run-off in the rainy season but dust and flies play a significant role in propagation. Farag et al. (2013) and Ugbogu et al. (2006) studies correlate the transmission significance of flies. Significant to Shigella transmission is the minute infectious dose (10 to 100 bacterial cells) that make it easy to carry from object or person to the other (Todar, 2010; Washington et al., 2006; Cheesbrough, 2006). Paper and coin currency is used in exchange for goods and services globally. Circulation of currency from one individual to another potentially spreads microorganisms. In South Africa, Shigella is equally transmitted through currency as evidenced in Igumbor et al. (2007) study in the Limpopo province. A total of 96% of the assayed currencies were contaminated and enteric pathogens compositions were E. coli (9.2%), Enterobacter (5.8%), Salmonella species (2.5%) and Shigella (1.7%). 17 1.9 The disease Shigellosis The hallmark of shigellosis is diarrhoea. After ingestion of bacteria, incubation period of shigellosis varies from 24 hours to a week with sudden onset or insidious. It normally presents as simple diarrhoea but may be varied in its severity, especially in Shiga toxin producing, S. dysenteriae type 1, where an acute fulminating attack may occur (Mandomando et al., 2007). The disease is established in human intestine when the bacteria log in the large intestine causing enteritis. Clinical manifestations include fever, vomiting, abdominal pain, tenesmus (painful straining to pass stools) and stools containing blood and mucus resulting from invasion of the intestinal mucosa by the pathogen. Many cases present with only a watery bloody diarrhoea but enteritis without diarrhoea is not uncommon (CIDAAP, 2009; Todar, 2010). Illness is usually self-limited and lasts an average of 4 to 7 days in healthy individuals. However, severity and fatality rate are functions of the age and pre-existing nutritional and immunity state of the host as well as the infecting Shigella serotype. Life-threatening complications are often seen in malnourished infants and young children below five years old (WHO, 2010). These include metabolic derangements such as dehydration, hyponatremia and hypoglycaemia. Also common are intestinal complications like toxic megacolon, rectal prolapse and sometimes intestinal perforation, but sepsis is rare (Mandomando et al., 2007; CDC, 2010). Reactive inflammatory arthritis (Reiter’s syndrome) plus haemolytic-uremic syndrome are additional complications associated with S. flexneri and S. dysenteriae respectively. Shigella bacteraemia has been reported as an opportunistic infection and/or associated with HIV/AIDS and other immune-compromised patient’s conditions where its pathogenicity is devastation (Obi et al., 2007; CDC, 2010; Keddy et al., 2012). 1.10 Pathogenicity of Shigella Shigella causes disease by invading and replicating in cells lining the colonic mucosa. Epithelial cells of the colonic mucosa are the primary targets used by these bacteria and a key step in the pathogenesis of Shigella infection. Ray et al. (2009) elucidate the process of cell infection to be aided by the bacterial DNA encoding a number of plasmid and chromosomal proteins that 18 assisted in adhesion of bacterial cells to epithelial cells with subsequent invasion through the M cells. M cells are specialized epithelial cells which continuously sample material from the gut lumen and deliver them to the underlying mucosal lymphoid tissue, where immune responses can be initiated. This in turn facilitates transportation of bacteria (Man et al., 2004; Winkler et al., 2007). Shigella species appear unable to attach to differentiated mucosal cells rather than the M cells located in Peyer's patches. The type III secretion system mediates secretion of four proteins (IpaA, IpaB, IpaC, IpaD) into epithelial cells and macrophages. These proteins induce membrane ruffling on the target cell, leading to engulfment of the bacteria. Intracellular multiplication and intra- and intercellular actin-based motility mechanisms allow bacterial spreading from cell to cell and eventual host cells death (apoptosis). Apoptosis is accompanied by the release of the pro inflammatory cytokines interleukin-1β (IL-1β) and IL-18 which are critical mediators of acute and massive inflammatory response partially accounting for presence of polymorph neutrophils in dysentery. Shigella infection is characterized by degeneration of the epithelium and inflammation of the lamina propria resulting in desquamation and ulceration of the mucosa with eventual leakage of blood and mucus into the lumen of the intestine. During infection, water absorption by the colon is negligible and this exacerbates diarrhoea. It is possible that prostaglandin interactions induced by the inflammatory response to bacterial invasion contribute to intestinal electrolytes and fluid movement resulting in colitis and diarrhoea (Lehmann et al., 2005; Todar, 2010; Hodges and Gill, 2010; Romero et al., 2011). Central to its mechanism of virulence, Shigella expresses a type III secretion system (T3SS) that is responsible for the conveyance of a series of bacterial effectors into host cells, aimed at diverting host cellular processes that result in direct bacterial colonization and subsequent dissemination within the mucosal epithelium via subjugation of the host inflammatory response (Lehmann et al., 2005; Todar, 2010). The lipopolysaccharide (LPS) layer of Gram-negative bacteria is an important component of the cell surface and contributes to the virulence of many pathogens by providing resistance to certain host defences such as opsonization, phagocytosis and intracellular or serum killing and phagocytosis (Schroeder and Hilbi, 2008). The pathogenesis of Shigella is also attributed to the possession of the potent endotoxin which is associated with Lipopolysaccharide. S. dysenteriae, 19 in addition, contains thermomolabile toxin shiga toxin (verotoxins) which is known to cause paralysis, diarrhoea and death, when injected to rabbits, mice, or guinea pigs and haemolytic uremic syndrome, inhibit protein synthesis in eukaryotic cells, play a role in haemorrhagic colitis, damage endothelial cells in both kidney and brain, causing renal failure and neurological and or other life-threatening extra intestinal complications in human beings (Keenan et al., 1986; Todar, 2010). Shiga toxin is composed of two subunits (subunit A and B). Subunit B (32-kd) possesses the main biological activities which are responsible for binding to cell-surface receptors and are responsible for entero-toxicity, neurotoxicity and cytotoxicity (Pieper et al., 2009). The enterotoxin 1, ShET1 and ShET2, is produced by several Shigella strains and has been found to induce fluid secretion into the intestine, thus accounting for the watery phase of diarrhoea (Schroeder and Hilbi 2008; Pieper et al., 2009). 1.11 Diagnosis of Shigella The procedure for collection of stool and rectal swabs for laboratory confirmation of Shigella is relatively simple and cheap. Where delay in transportation to the laboratory is foreseen samples are ideally kept in appropriate transport medium and in controlled cool temperatures to keep the organism viable (Cheesbrough, 2006). Successful treatment of shigellosis is dependent on correct detection of the causative agents particularly in clinical samples. The two forms of dysentery exist namely amoebic and bacillary are distinguishable by macroscopic and microscopic examination of the stool. The traditional diagnosis of bacillary dysentery was based upon microscopic examination stool. Examination of the mucus stained faeces in acute bacillary dysentery show an increased number of cells predominance of polymorph nuclear cells and red cells, was once an essential tool to diagnose shigellosis (Cheesbrough, 2006; Washington et al., 2006). Definitive diagnosis of Shigella infection relies largely on traditional microbiological culture techniques of demonstrating the presence of the microbe, in line with Koch’s postulates (CDC, 2013). The organisms are usually present in mucus or the faeces in the early stages. Freshly passed stools should be examined, although rectal swabs showing marked blood-mucus faecal staining may be used. Cary-Blair transport media is commonly used to preserve viability of 20 bacteria when delay in the specimen reaching the laboratory or simply as a way of sending specimen to the laboratory (Cheesbrough, 2006; Washington et al., 2006; Todar, 2010). Isolation and identification of Shigella is enhanced when optimal laboratory media and techniques are employed. Two media are generally used: a general purpose plating medium of low selectivity, such as MacConkey agar (MAC) and a more differential and selective agar medium, such as Xylose Lysine Desoxycholate (XLD) agar. Desoxycholate Citrate Agar (DCA) and Hektoen Enteric (HE) agar are suitable alternatives to XLD agar, as media of moderate to high selectivity. Salmonella-Shigella (SS) agar is not a suitable alternative as it frequently inhibits Shigella dysenteriae type 1 and S. sonnei (Cheesbrough, 2006; Washington et al., 2006). Cheesbrough (2006) and Washington et al. (2006) describe MAC, XLD and DCA media as containing bile salts which inhibit the growth of other gram-negative bacteria and pH indicators for differentiation of lactose fermenters such as E. coli (coliforms) from non-lactose fermenters such as Shigella. MacConkey agar (MAC) is an example of a differential plating medium used in the isolation and differentiation of lactose-non-fermenting gram-negative enteric bacteria from lactose-fermenting organisms. Hektoen Enteric Agar is a differential selective agar that is useful for isolation of Salmonella and Shigella. It has, Hydrogen Sulphide, H2S-indicator system for selecting H2S-producing Salmonella, which produce blue-green colonies with a black centre while Shigella does not. Desoxycholate citrate agar (DCA) is a differential selective plating medium for the isolation of enteric pathogens, particularly Shigella and Salmonella. Colonies of non-lactose fermenting strains are colourless. Xylose lysine desoxycholate agar (XLD) is a selective differential medium developed for isolating and differentiating gram-negative enteric bacilli, especially Shigella and Providencia. It is suitable for isolation of Shigella and Salmonella from stool specimens. Differentiation of these two species from non-pathogenic bacteria is accomplished by xylose and lactose fermentation, lysine decarboxylation and hydrogen sulphide production. SalmonellaShigella Agar (SS Agar) is used for isolating Salmonella and some Shigella. In SS Agar, bile salts and brilliant green inhibit gram-positive bacteria, most coliform bacteria, and the swarming phenomenon of Proteus species. Salmonella and Shigella species are non- lactose fermenters and 21 form colourless colonies. SS Agar is a highly selective medium and some Shigella strains may not grow, particularly Shigella dysenteriae type 1, therefore, it is not recommended as the sole medium for primary isolation of Shigella (Cheesbrough, 2006; Washington et al., 2006). In parallel, samples can be enriched for example in selective and or enrichment broth and further cultured on solid media. A liquid enrichment medium such as Hajna Gram-Negative Broth (HGNB) may also be inoculated with the stool specimen and subcultured onto the selective/ differential agarose media after a short growth period. Bacto Selenite Broth or Selenite F (Faecal) Broth is used for enriching especially Salmonella species and some species of Shigella that may be present in small numbers and competing with intestinal flora during isolation procedures and for isolating Salmonella in foods. Sodium selenite temporarily inhibits the growth of gram-positive bacteria, for 8 to 12 hours. However, culturing Shigella may be rather difficult because of its sensitivity in their growth requirements and, therefore, more fastidious (Cheesbrough, 2006; Washington et al., 2006). Shigella appears as small about 2 to 3 mm in diameter, translucent and colourless or slightly pink colonies on DCA and about 1 to 2 mm diameter pink or red in colour colonies as lysine is decarboxylated producing alkaline end products which raises the pH and cause the agar to turn into deep red colour on XLD. Shigella does not produce hydrogen sulphide (H2S) on the XLD, HEK and SS agar. A few strains grow poorly on inhibitory media, and it is advisable to use MacConkey agar and to examine any non-lactose-fermenting colonies after overnight incubation (Cheesbrough, 2006; Washington et al., 2006). Identification of Shigella species involves both biochemical and serologic testing. Shigella strains are oxidase-negative, non-motile, lysine-decarboxylase negative, and urea is not hydrolysed. Triple Sugar Iron (TSI) Agar and Kligler Iron Agar (KIA) are commonly used biochemical tests to exclude bacteria from Enterobacteriaceae. Bacteria that ferment glucose are detected by observing the reaction they produce when grown on TSI or KIA. For example, if an organism cannot ferment glucose an alkaline slant and butt is observed. Based on the organism’s inability to produce acid and ferment any of the sugars present it is excluded from Enterobacteriaceae. However, the Corporation of beef and yeast, peptone and protease peptone 22 nutritionally rich but the lack of inhibitors permits the growth of all, especially fastidious bacteria. It is for this reason that TSI and KIA are used to test bacteria selected from a single colony, therefore, limits the method to screening only (Washington et al., 2006). The reaction of Shigella strains to biochemical sugar-markers (Table 2.4) is useful for prescreening. Table 1.4 Biochemical substrates for characterising Shigella Substrates Visual reaction API 20E positive Shigella Shigella Shigella Shigella dysenteriae flexneri boydii sonnei A B C D negative ONPG(β-alatosidase) Yellow colourless - - - + Ornithine Red- yellow - - - + decarboxylase orange Urease red yellow - - - - H2S production Dark ring colourless - - - - Voges-Poskauer red colourless - - - - Indole production Red-ring yellow +/- +/- +/- - + + + + - - - - - - - + - - - - + + + + - - - -/late Methyl Red Christensen citrate Dark blue Light green Lysine Decarboxylase red/orange yellow (LDC) Gas production from glucose Fermentation of: Glucose yellow Bluegreen Lactose 23 Mannitol yellow Blue- - + + + V v V + - + + + green Arabinose inositol yellow Bluegreen V= Different species give different results; - Negative reaction; + Positive reaction. Adopted from BioMérieux, 2010. Recent diagnostic methods detect pathogens on the basis of features that differentiate them from normal flora present in clinical samples. According to the level of expression, these approaches fall into chromogenic media, virulence test, molecular methods, and immunological detection. 1.11.1 Chromogenic Media The use of chromogenic substrates (chromogens) in media formulations has immensely transformed culture media and reduced the number of preliminary biochemical identification tests of pathogens. Chromogens when broken down by specific bacterial enzymes result in coloured colonies. Most commercially available chromogenic media have exploited indoxylic substrates. Indoxyl and its halogenated derivatives can be differentiated into a range of esters. Release of indoxyl through hydrolysis by a specific bacterial enzyme results in the formation of brightly coloured indigo dye. This is due to spontaneous dimerisation of indoxyl molecules in the presence of oxygen. Halogenation of the indoxyl molecule has a dramatic effect on the colour and intensity of this chromogen. For example, 5-bromo-4-chloro-indoxyl forms a bright green/blue dye whereas 5-bromo-6-chloro-indoxyl forms a magenta dye. Indoxylic glycosides including glucoside, galactoside and glucuronide derivatives are widely used because of their high sensitivity, low toxicity and availability from a number of commercial sources (Cheesbrough, 2006; Washington et al., 2006; Perry and Freydierre, 2007). HardyCHROM SS media is one such primary screening medium for the isolation and differentiation of both Salmonella and Shigella species from non-pathogenic enteric bacteria (both lactose and non-lactose fermenting organisms). Differentiation is accomplished by three mechanisms namely chromogenic reactions, carbohydrate fermentation and hydrogen sulphide 24 production. According to Perry and Freydierre (2007), this media provides better differentiation of colonies from clinical samples hence resulting in less secondary screening of isolates and less false-positive results. 1.11.2 Virulence Tests for Shigella The Virulence tests depend on full or partial expression of virulence. For Shigella, a guinea pig eyes (Serény) test was developed in which virulent Shigella strains inoculated into the conjunctival sac of the guinea pig elicit keratoconjunctivitis within three days. The Sereny/ virulence eye test has since been applied on mice and rabbits with successful results (Murayama et al., 1986; Ramos-Moreno et al., 2009) and testing the invasion of the bacteria employed Henle intestinal epithelial cells in tissue culture (Hale and Bonventre, 1979). These tests have in part contributed to the understanding of the pathogenesis of Shigella. Despite these methods being highly specific their application in routine diagnostic laboratories may present challenges due to their complex special requirements such as an animal-house, the availability of cell culture and high level of education to interpret results accurately. 1.11.3 Molecular techniques The scale of shigellosis cannot, therefore, be accurately be ascertained by culture methods only that are mostly used in developing countries. The introduction of rapid and reliable molecular assays to detecting and identifying Shigella in food, environmental and clinical samples should be easily available. Those molecular based techniques are in practice in developed countries where they demonstrate decreased diagnostic time, which is essential in clinical diagnostic (Peng et al., 2006; Warren et al., 2006; Pazhani et al., 2008; Li et al., 2009; Ojha et al., 2013). The molecular assays aim to detect the genes coding certain virulence markers directly in the sample or after isolating the bacteria. There are DNA hybridisation and polymerase chain reaction (PCR) procedures. In PCR a virulence specific region is amplified to an amount that allows for detection. Virulence specific region of the target DNA in the sample hybridises with the known homological sequences. For example, many investigators have described the usefulness and accuracy of assays for invasion plasmid antigen H (ipaH) and ial genes (Jiménez et al., 2010), O serotype-specific genes (Li et al., 2009), gene sequence for invC of the genus 25 Shigella and gene sequences for invC, rfc, wbgZ, and rfpB of S. flexneri, S. sonnei, and S. dysenteriae respectively (Ojha et al., 2013). However, these methods do not yield the microbe but demonstrate the aetiological pathogen’s presence and, therefore, antibiotic susceptibility testing methods recommend by CLSI and commonly used to monitor susceptibility and development of resistance pattern changes pertinent for patient management are not possible. 1.11.4 Immunological Tests Immunological methods such as latex agglutination (LA), enzyme immunoassay (EIA) or immunomagnetic separation (IMS) have been employed for the detection of food and water borne bacterial pathogens such as Shigella. LA, EIA and IMS methods use monoclonal or polyclonal antibodies to bind to specific antigens present on the surface of bacterial cells. For this reason, development of antibodies with sufficient specificity is crucial for the performance of immunological methods. Like other bacterial infections, Shigella infection also induces humoral immune cell mediated response against protein and LPS antigens which are induced and harvested for use (Taneja et al., 2011). The LA tests use latex particles coated with antibodies specific for target bacteria. Binding that occurs causes a visible clumping of the latex particle-bacteria complexes that are seen with the naked eye. LA methods require prior isolation, on solid media, and correct biochemical identification of suspect colony. For this reason LA methods cannot be used for detection directly from faecal, food or environmental specimens but as confirmatory aid in characterization of suspected Shigella colonies (Metzler and Nachamkin, 1988). Several kits for Shigella are commercially available, however, only one kit will be discussed in this review. The Wellcolex Colour Shigella Test (WCT-Shigella, Remel Inc., Thermo Scientific) allows the identification of isolates to species level using only two reagents, each consisting of a mixture of red and blue latex particles coated with antibodies specific for each of the four different Shigella serogroups. Each reagent is added to one of two identical sample spots of the suspect isolate. The presence of homologous antigen results in the agglutination of one colour coupled with a change in background colour. Colour change combinations due to any of the four Shigella serogroups are easily distinguishable as is the negative reaction in which the particles remain in smooth 26 purple suspension. Non-specific agglutination results in a purple agglutination with a clear background (Cheesbrough, 2006). Generally, Shigella group and serotype are identified by slide agglutination using antisera. Both polyvalent and monovalent Shigella antisera are commercially available. Polyvalent antisera contain antibodies to multiple serotypes of Shigella. For example, most commercially available polyvalent antisera for Shigella flexneri will react with all serotypes of S. flexneri while monovalent antisera are used to detect serotype. For example, S. dysenteriae Type 1 antiserum will only react with of S. dysenteriae type 1 strain (Lefebvre et al., 1995; Cheesbrough, 2006; Washington et al., 2006). 1.11.5 Enzyme Immunoassay (EIA) EIA tests use enzyme-labelled antibodies to bind antigens and detection is through colorimetric reaction. Enzyme label and Microplate generally readers are used to record these colorimetric signals. In brief, immunoassays rely on the ability of an antibody to recognize a specific site (epitope) on an antigen and bind to form complex mixture of macromolecules. In these tests the analyte may either be an antibody or antigen. Through the use of colour coated substrates bound to the antibody-antigen complex mixture presence or concentration of analyte is spectrophotometrically measured. There are many different EIA methods that have been developed for diagnosis of shigellosis. For example, commercially available Shigel Dot A, B, C, and D test kits, a monoclonal antibody-based Enzyme-Linked Immunosorbent Assay (ELISA) and an enzyme immunoassay for stx is used to detect S. dysenteriae type 1 in the stool (Warren et al., 2006). The format in dot-enzyme immunoassay test is that specific antigens or antibodies are immobilized on a membrane (usually nitrocellulose) and the reaction is observed by enzyme activity. ELISA techniques have been used for detection of serum and urine antibodies of various immunoglobulin classes developed against Shigella serogroup specific LPS. Kits that detect the levels of serum IgA to Shigella LPS and base their interpretation on that increase in the level of serum IgA to Shigella LPS indicate recent infection. Also other ELISA methods based on 27 purified recombinant IpaD protein for identification of Shigella species is commercially available (Warren et al., 2006; Todar, 2010). Immunomagnetic separation (IMS) is a laboratory method that efficiently isolates and quantifies pathogenic or target cells out of body fluid, cultured cells, food or faeces. IMS involves beads coated with antibodies against the surface antigens of target bacterial cells. Paramagnetic beads exhibit magnetic properties when placed within a magnetic field but no magnetism when removed. This technique has been used as a preliminary concentration method for further test such as PCR and DNS based assay (Warren et al., 2006; Yue-Ying et al., 2012) and assay for enteric foodborne pathogens including Shigella. With the growing use of molecular techniques in determining pathogens, simplicity in equipment and methodology has become common. Equally, agglutination and ELISA methods are common and technically simpler to use with rapid result. These qualities have enhanced laboratory recovery of Shigella and other food borne pathogens from variable sample sources. 1.11.6 Other Laboratory diagnosis of Shigella The pathophysiology changes caused by Shigella infection are a guide in employing screening tests for diagnosis. Shigella infection results in direct effects on intestinal epithelial ion transport processes, inflammatory or cytokine secretion and activation of enteric nerves through neuropeptides. Acute phase responses always develop in bacterial infection such as shigellosis. This condition causes the release of interleukin-6 and other cytokines that trigger the synthesis of C-reactive protein (CRP) and fibrinogen by the liver. Levels of CRP during acute phase response rapidly increase within 2 hours of infection, reaching peak at 48 hours. With resolution of the acute phase response, CRP declines with a relatively short half-life of 18 hours. Measurement of CRP level is a screen for infectious and inflammatory diseases. An elevated CRP level does not diagnose a specific disease but provides support for the presence of an inflammatory disease (Hale and Bonventre, 1979; Schroeder and Hilbi, 2008; Hodges and Gill. 2010). Haemoglobin may be influenced by the loss of blood and its assay is significant on the general oxygen transportation. Cellular responses to various steps of the invasion process are the primary 28 cause of inflammation. The release of IL-1β attracts Neutrophils which consequently release secretagogue adenosine and activation of Chlorine secretion is important in electrolyte balance (Schroeder and Hilbi, 2008; Hodges and Gill. 2010). Sodium, potassium, chlorine and carbon dioxide assays help understand plasma osmolality in diarrhoeal conditions. The chemotaxis of poly neutrophils may shift differential well count. However, in some cases, leucopoenia, anaemia and thrombocytopenia may occur particularly in Haemolytic Uremic Syndrome conditions (Mandomando et al., 2007). 1.12 Treatment of shigellosis An antimicrobial agent (antibiotic) is defined as a drug, chemical or substance which kills or inhibits the growth of a microbe (BioMérieux, 2008). There are several classes of antibiotics which are used to treat infectious diarrhoeal diseases caused by bacteria. These include the following: aminoglycosides, β-lactams, glycopeptides, fluoroquinolones, macrolides, streptogramins, sulphonamides, and tetracyclines. Bactericidal antibiotics are useful to eradicate bacterium, reduce severity of symptoms, shorten the length of infection and prevent live bacterium being defecated (BioMérieux, 2008; Todar, 2010). They effectiveness is based on varying modes of action such as Amingolycosides targeting the 30S subunit of the bacterial ribosome and interferes with protein synthesis. Beta lactams target enzymes necessary for bacterial synthesis of the peptidoglycan layer so interfere with synthesis of the cell wall. In the Penicillin combinations such as Amoxicillin/clavulanate, the second component (clavulanate) prevents bacterial resistance to the first component (BioMérieux, 2008; Todar, 2010). Glycopeptides interfere with the synthesis of the bacterial cell wall by targeting the D-alanyl-Dalanine terminal dipeptide and preventing the reaction used to link peptidoglycan precursors while Fluoroquinolones inhibit the bacteria synthesis of DNA gyrase or the topoisomerase IV enzyme, thereby inhibiting DNA replication and transcription. DNA gyrase or topoisomerase IV enzyme is responsible for negative supercoiling of double-stranded DNA which balances the positive supercoiling of DNA replication. In the absence of negative supercoiling permanent 29 breakages occur in the DNA strands. Macrolides target the 50S subunit of the bacterial ribosome and block the exit of the peptide chain (BioMérieux, 2008; Todar, 2010). Streptogramins are similar to macrolides in that they also target the 50S subunit inhibiting protein synthesis. Sulphonamides target the para-aminobenzoic acid molecule which is used to synthesize folic acid by the bacteria and blocks the synthesis of folic acid. Folate synthesis inhibition is a competitive inhibitor of the enzyme dihydropteroate synthetase which catalyses the conversion of para-aminobenzoate to dihydropteroate, a key step in folate synthesis. Folate is essential for the cell to synthesize nucleic acids (building blocks of DNA and RNA) and in its absence cells cannot divide (BioMérieux, 2008; Todar, 2010). Tetracyclines target the 30S subunit of the bacterial ribosome and inhibit protein synthesis by preventing transfer of amino acids to the ribosome. They inhibit the binding of aminoacyl-tRNA to the mRNA-ribosome complex mainly by binding to the 30S ribosomal subunit in the mRNA translation complex (BioMérieux, 2008; Todar, 2010). From the working assay card at Lancet microbiology Laboratories Richmond, South Africa, depicts the classes of antibiotics commonly tested for, which in turn is assumed as the commonly used antibiotics are as follows: The aminoglycoside class include gentamicin and amikacin, macrolides include azithromycin. Encompasses in beta-lactam are penicillin, ampicillin, amoxicillin and amoxicillin-clavulanic acid while third generation cephalosporins are ceftriaxone and ceftazidime. The sulphonamide class contains sulphamethoxazole and potentiated sulphonamides such as trimethoprim and sulphamethoxazole. The tetracycline class includes chlortetracycline, oxytetracycline, tetracycline, limecycline, and doxycycline while fluoroquinolones include ciprofloxacin, ofloxacin, norfloxacin, lomefloxacin, levofloxacin, enoxacin and sparfloxacin. The choice of effective antibiotics should be based on recent surveillance data that monitor trends in antimicrobial use and antimicrobial resistance in Shigella strains from human, animal and food sources in the area, across the country or neighbour countries. Broad-spectrum activity against gram-negative, such as Ceftriaxone, Ciprofloxacin and Azithromycin, because of its inhibition of bacterial protein biosynthesis by binding reversibly to the 50S subunit of the 30 bacterial ribosome, thereby inhibiting translocation of peptidyl tRNA, are recommended (WHO, 2010; CDC 2013). While antibiotics eradicate bacteria, hydration is an important concern of infectious diarrhoeal patients particularly those infected with Shigella. Oral rehydration is necessary to prevent severe dehydration, electrolyte imbalances and metabolic acidosis caused by fluid loss (Mandomando et al., 2007). 1.12.1 Mode of Drug Resistance in Shigella It is widely accepted that antibiotics are the “magic wand” and their use in human medicine, veterinary/animal or poultry medicine and agriculture is undoubtedly widespread. Excessive antibiotics usage is perhaps the most important factor stimulating the emergence, selection and dissemination of resistant organisms in both veterinary and human medicine. The effect of widespread use of antibiotics and subsequent dissemination of resistant bacteria, multi drug resistance (MDR) has been documented worldwide in both human and veterinary medical settings. To circumvent the bactericidal effects of drugs, Shigella, also common to Enterobacteriaceae, has developed variable mechanisms. Intrinsic and acquired are two forms of antibiotic resistance in bacteria (Cheesbrough, 2006; Washington et al., 2006; BioMérieux, 2008; Todar, 2010). Intrinsic or natural resistance results from evolutionary adaptations of bacteria to the environment. The failure of an antibiotic to penetrate a bacterial cell, lack of target sites for the antimicrobial agent to act against and coupled with efflux pump are natural bacterial adaptations which result in resistance (Todar, 2010). Acquired resistance may result from single or multiple mutations or from the lateral transfer of resistance traits between bacteria of the same species or different species, or acquired from the environment. There are three horizontal gene transfer mechanisms in bacteria namely transformation, transduction and conjugation. The most common horizontal gene transmission 31 mechanism among bacteria especially from a donor bacterial species to different recipient species is conjugation (Todar, 2010; Domingues et al., 2012). Development of MDR strains is due in part to the ability of bacteria to acquire and disseminate exogenous genes or extra chromosomal DNA through mobile genetic elements such as plasmids, integrons, transposons, insertion sequences and genomic islands (Rowe-Magnus et al., 2002; Guo et al., 2011; Domingues et al., 2012). Integrons are genetic elements, implicated in dissemination of resistance that acquire and exchange exogenous DNA known as gene cassettes by a site-specific recombination mechanism. The most notable gene cassettes identified within integrons are those conferring resistance to antibiotics (Guo et al., 2011). The essential component of an integron is a gene cassette which encodes a site-specific recombinase belonging to the integrase family composed of a 5’ conserved sequence which includes the integrase gene (intI1), the adjacent recombination site (attI1), the promoter (Pc) and 3’ conserved sequence (3’CS), that contains the qacE∆1 gene (encoding an incomplete version of a quaternary ammonium compound resistance), the sulI (encoding resistance to sulfonamides) and the orf5 (Boucher et al., 2007; Gillings et al., 2008). Integron gene cassettes can be deleted, rearranged and duplicated within the integron. Class 1 integrons are the most widely disseminated type in commensals and pathogens of human and animal and have also been found in soil and in aquatic (Gillings et al., 2008). Madiyarov et al. (2010), reported the presence of integron in the most commonly isolated Shigella species in the developing (S. flexneri) and developed (S. sonnei) countries. Plasmids are circular bodies of double stranded DNA which are separate from the chromosome and carry genes that encode various traits such as virulence and MDR (Cheesbrough, 2006; Washington et al., 2006). Of the two transfer methods, namely conjugative and non-conjugative, conjugative plasmids transfer resistance via their sex pilli whereas non-conjugative plasmids must have direct contact for transfer to occur. In non-conjugative transfer, both the donor bacteria and the recipient bacteria have a copy of the transferred plasmid. Conjugative transfer is an important mechanism in MDR because transfer can occur in a wide range of bacterial species and can be spread to unrelated organisms. Moreover, a single plasmid can contain multiple genes conferring resistance to multiple classes of antimicrobials (Cheesbrough, 2006; Washington et al., 2006). 32 Transformation occurs when bacteria pick up free DNA from the environment especially after death and lysis of another bacterium (Todder, 2010). A transposon is a genetic element that contains an insertion sequence at each end. The insertion sequences allow the gene to “jump” to different positions on the chromosomal DNA from plasmid to plasmid or from chromosome to plasmid (Cheesbrough, 2006; Washington et al., 2006). This gene transposition is an important facet of MDR transfer because resistance genes can be moved from a non-conjugative plasmid or chromosome to a conjugative plasmid and hence transferred to other bacteria (Cowley and Oakey, 2013). The chemotherapeutical medication of shigellosis has a discouraging history due to the continual development of drug resistance. Apart from physiological changes in bacterium and consequently its antibiogram change, these changes are never stable and often change rapidly, especially in places where antimicrobials are used excessively, particularly in developing countries where socioeconomic and behavioural factors may influence excessive antibiotic use, therefore, bacterial acquisition of resistance (Yismaw et al., 2006). Furthermore, the use of antibiotics inevitably leads to some resistance (Fhogartaigh and Edgeworth, 2009). The development and spread of antibiotic resistance continues to grow daily and is currently viewed as a major threat to global public health (WHO, 2009), drug specific resistance mechanism have been modelled. According to Cheesbrough (2006) and Washington et al. (2006), a variety of mechanisms have been studied and classified into the following. In beta lactam, ineffective treatment is due to antibiotic failure to cross cell wall membrane, to bind to altered penicillin-binding proteins and enzymatic hydrolysis. Those that Inhibition of Protein Synthesis (Translation) on 30S ribosome site are attributed to mutation of ribosomal binding sites, decreased antibiotic uptake, enzymatic modification of antibiotic and active efflux of antibiotic out of cell. Tetracycline blocks the tRNA binding to 30S ribosome-mRNA complex to be effective. Effectiveness of Azithyromycin is methylation of 23S ribosomal RNA subunit, however, enzymatic hydrolysis and cleavage of the macrolactone ring catalyzed by erythromycin esterases, EreA and EreB and the active efflux ensure its effectiveness. Quinolones ineffectiveness is through alteration of alpha subunit of DNA gyrase (chromosomal) and 33 decreased uptake by alteration of porins. While Sulfonamides experience permeability barriers and in Trimethoprim inhibition of dihydrofolate reductase prevents synthesis of folic acid. Over the years Shigella has developed some reistance to Ampicillin, Cephalosporins, Cotrimoxazole, Chloramphenicol, Fluoroquinolones, Gentamicin, Nalidixic acid and Tetracycline, therefore, the need for robust laboratory based surveillance to monitor patterns of antibiogram for this organism cannot be over emphasized. 1.13 Shigellosis and HIV/AIDS Human Immunodeficiency Virus (HIV) is a lentivirus, a group of retroviruses that causes slow development of acquired immunodeficiency syndrome (AIDS) which results in immune system failure and increased suscepibility to life-threatening infections. This immunosuppression leads to the development of severe opportunistic infections which are otherwise rare in uninfected individual (UNAIDS, 2012). This defect in immunity is in both the cell-mediated and humoral immunity (Chakrabarti, 2010). Gastrointestinal opportunistic infections are very common in patients with HIV/AIDS and diarrhoea is a mainstay hallmark presentation of both infections. Bacterial, viral, fungal and protozoan infections are commonly reported opportunistic pathogens. Of the bacterial pathogens, the three most common are Salmonella, Campylobacter and Shigella and their severity is associated with the level of CD4 count with lowest count experiencing worse symptoms (UNAIDS, 2012). There is increasing evidence that shigellosis is a predominantly sexually-related transmitted disease among men who have sex with other men (Daskalakis and Blaser, 2007) and that infection with HIV is a risk factor due to profound diarrhoeal effects of the two pathogens. Since HIV/AIDS is endemic (UNAIDS, 2012) and global burden of shigellosis (Nigoyi, 2005) there is a significant interaction between HIV/AIDS and Shigella infection among adults or children. Therefore, incorrect diagnosis of shigellosis in persons with compromised immunity may have extended carriage of Shigella species or prolonged shedding with high titer. 34 Worrisome in South Africa is evidence of increase of shigellosis among patients with HIV/AIDS (Obi et al., 2007; Keddy et al., 2012). This is threatening, when considering that by year 2020, because of absences of the AIDS vaccine and limited access to anti HIV/AIDS treatment, nearly half a billion people globally will be living with HIV/AIDS (UNAIDS, 2012). Also in view of emerging ESBL Shigella strains, the combination of HIV/AIDS and shigellosis will be difficult to control, treat and or eradicate. 2.14 Prevention management of Shigella infection The laboratory-based surveillance of Shigella is important for identifying trends in infection in a population so that policies and punitive measures are evaluated. Development of Shigella vaccine has been attempted to offer serotype specific protection, unfortunately, no effective formula has been discovered yet (WHO, 2009; Todar, 2010). For now, interventions should target measures that stop the spread of bacteria. WHO (2009) recommends the following measures: Appropriate hand washing practices with soap to remove bacteria especially from finger nails after use of a toilet. All diaper-changing practices must be followed by hand washing. Proper faecal and diaper disposal to prevent flies from carrying bacteria from stool to food. All waste disposal bins must be fitted with a lid to prevent flies from being vectors. Appropriate measures to ensure safety of drinking water should be taken. Caring for children in smaller groups helps monitor and supervisor children individually, therefore, control transmission from fomite and person to person. Infected individuals shall be treated with known effective antibiotics and retested to ensure complete cure. Food must be properly cooked and where raw vegetables must be consumed properly washing with clean water prior is a pertinent preventative measures. 35 Bacteriophage, despite less popular, is useful to control pathogens such as Shigella from the surroundings. In bacteriophages science, bacterial viruses are used as antimicrobial agents or therapeutically tool (phage therapy) to reduce or eliminate populations of bacteria in animals, surfaces, fomites and/or inorganic and organic matter (Kutateladze and Adamia, 2010; Goodridge, 2013). These methods could be useful to control Shigella bacteria especially on food. Zhang et al.’s (2013) illustration of this “phage based bio-control” on ready-to-eat spiced chicken eliminating Shigella is a useful eye opener. The report showed a significant reduction of the initial bacteria inoculum after application of bacteriophage. This phage therapy application was shown to be safe in animals and including human (Burrowes et al., 2011), therefore, phage therapy has a therapeutic potential or as an adjunct to antibiotics especially where antibiotic resistance is high as is observed in Shigella. There are a wide range of bodies globally involved in monitoring and researching microbial activities associated with food, water and health. Bodies such as Food and Drug Administration (FDA), WHO, Food Standards Agency (FSA) in USA, the Institute of Food Research (IFR) in the UK, Medical Research Council and Council for Scientific Research in South Africa establish food and water safety programmes derived from extensive research that highlight incidences of food and water borne disease. 1.15 Problem Statement Shigellosis is a global public health problem associated with food and water-borne infectious diarrhoeal disease caused by bacteria of the genus Shigella which has been implicated in many outbreaks and sporadic cases globally (WHO, 2009). In South Africa, infectious diarrhoea such as shigellosis accounts for about 17% mortality (Stat SA, 2012) especially in children below 5 years old. High levels of antibiotic resistance among Shigella isolates (Brink et al., 2007; Crowther-Gibson et al., 2011) exacerbate the disease management. Infection with Shigella in immunocompromised patients such as in HIV/AIDS worsens the disease condition and arguably accelerates patient mortality. Effective laboratory surveillance systems employed in public health care systems are useful in disease prevention and management, however, surveillance in private health care system is optional and in some areas obscure. The purpose of this study, therefore, was to investigate the 36 organism’s prevalence and its antibiotic resistance patterns in private health care system and compare with global patterns and/or concluded that Johannesburg, South African patterns are unique. 1.16 Objectives of the study 1.16.1 Main objective To establish the burden of shigellosis in townships in Johannesburg, South Africa. 1.16.2 Specific objectives To determine the monthly prevalence of Shigella in varying age groups To ascertain the antibiotic resistance profiles of isolates To provide updated data 1.16.3 Significance of Study Baseline information on prevalence, predominant serotypes and antimicrobial resistance profiles of Shigella is important in management strategies, prioritization and potential encouragement of policy dialogue on optimization of interventions 37 CHAPETR TWO MATERIALS and METHODS 38 Chapter Two MATERIALS AND METHODS 2.1 Study Laboratory The Lancet corner Medical Microbiology Laboratory is situated in the Richmond suburb areas of Johannesburg, Gauteng province, South Africa on Longitude 28.0143 and Latitude -26.18377. The referral Laboratory is accredited by South Africa National Accreditation System (SANAS) and adheres to international criteria set out according to ISO Standard 15189 to culture human stool samples for isolation of enteric pathogen and test their antibiotic response for clinic therapy, scientific communication, scholastic and planning purposes. 2.2 Experimental Design In this study, patients who presented with acute, bloody mucus diarrhoea, stomach discomfort to their clinicians and all others, regardless of the clinical reasons for which stool culture was indicated were included. All patients’ faecal specimens from 1st January to April 2013 collected from clinics located in the Johannesburg area were sent to the Laboratory for culture in the period January to April 2013 and were assayed. Confirmation of shigellosis was based on laboratory culture and isolated of Shigella organism from faeces and antibiotic susceptibility on disc diffusion method. 2.3 Sample Area (Johannesburg) According to the Johannesburg municipal web site, Johannesburg also known as Jozi, Joburg or eGoli, is the largest city in South Africa with a total population of 4,434,827 on a total area 1,645 km2 (635 square mile) with metropolitan area of 7,151,447 resulting in a population density of 2,364 /km2 (6,120 /square mile) racially blacks 64.2%, coloured 13.9%, Indian/Asian 6.7 %, White 13.9% others 1.3%. It is the commercial city of South Africa with location coordinates of 26°10’S 28°E as the provincial capital of Gauteng in Province. Johannesburg is arguably the most technologically advanced city in South Africa and one of the 50 largest metropolitan cities 39 in the world. The city is the source of a large-scale gold and diamond trade, due to its location on the mineral-rich Witwatersrand range of hills. The township used to be, in the apartheid era, underdeveloped location or living areas but to date the word township represents land demarcation and carries no racial connotations. Johannesburg is divided into more than a hundred human (township) dwelling areas and Lancet Laboratories offer services to many private hospitals, clinics and doctor’s consultation rooms that exits in these townships. 2.4 Sampling, handling and transport of specimen The study included all private health care centre settings serviced by Lancet Laboratories. All stool specimens were each received in a standard labelled container with a leak proof lid (Fig 2.1) and placed in a zipper leak proof plastic bag which in turn was put in a cooler bag with ice blocks to contain temperatures at 4°C and were transported to the laboratory. Each bag contains two pockets one for the specimen and the other for laboratory request form. All samples were not collected from bed pans or from containers priory disinfected but into sterile clean containers and used for the first time. Rectal swabs were collected from debilitated patients and other situations where voided stool sample were not feasible. Rectal swabs were transported in Cary-Blair medium media. All specimens reached the laboratory within two hours of collection. 2.5 Ethical considerations This manuscript has received the approval of the LANCET Publications Committee based on a review of its scientific content and data interpretation and the Research Ethics Review Committee of the College of Agriculture and Environmental Sciences, University of South Africa (Ref. Nr.: 2013/CAES/039). 40 Fig 2.1: Faecal sample in standard stool container. 2.6 Microbiological Culture In this study, the method described by Washington et al. (2006) for isolating enteric pathogens from stools was adopted. In brief, firstly, about a gram of stool sample was inoculated on Selenite F broth and incubated at 35 - 37°C for 18 to 24 hours or overnight, thereafter, a loop full of overnight bacteria growth was seeded and plated for isolation on XLD Agar and MacConkey Agar plates. Secondly, with a sterile swab, a stool inoculum of about 2cm diameter areas was seeded and plated for isolation on XLD Agar and MacConkey Agar plates and aerobically incubated at 35 - 37°C for 18 – 24 hours or overnight. Overnight plates were examined for typical growth. 2.7 Characterisation of Shigella 2.7.1 McFarland Turbidity Testing In 1907 McFarland developed a series of barium sulphate solutions to estimate the numbers of bacteria in solutions of equal turbidity. This is achieved by visually comparing McFarland 41 standards turbidity to that of test bacterial suspension. Because the McFarland turbidity is known an approximate number of bacteria in a suspension are then derived. McFarland standard of 0.5 corresponds approximately to homogeneous Escherichia coli suspension of 1.5 x 108 bacterial cells / mL (CLSI, 2012). McFarland standard tubes and machinery are today commercially available. An estimated bacterium inoculum to known substrate is today used to understand bacterial metabolisms and activities scientifically. Interpretations and performance of susceptibility testing and bacteria characterisation by substrates require the use of standard inoculum. In this study turbidity was measured using DensiCheck Plus. The instrument was blanked with saline and quality control performed with three known tubes of 0.0, 0.5 and 3.0 McFarland (BioMérieux, France) before a homogenous solution of normal saline bacterial suspension in a 12 x 75 mm clear plastic polystyrene test tube was determined. Recommended turbidity was attained by drop wise adding of normal saline to the bacteria-saline suspension. Recommended turbidity for VITEK 2 automated system, API characterisation and disc susceptibility testing was adjusted using the DensiCheck Plus equipment (BioMérieux) (Fig. 2.2). Fig. 2.2: The DensiCheck Plus equipment (BioMérieux, France). 42 2.7.2 VITEK 2 system ID-GNB card Pincus (2006) described the VITEK 2 system as an automated microbiology system utilizing growth-based technology to characterize bacteria. The system uses a 64 well reagent card, for identifying gram negative organisms. Also included are inoculated substrates including positive and negative control wells. Each card has a pre-inserted transfer tube for inoculating the wells with test organisms from a 12 x 75 mm clear plastic polystyrene test tube, a bar code where product type, lot number, expiration date and a unique identifier linkable to the sample either before or after loading the card onto the system is coded. The reagent card is inoculated with microorganism suspensions using a vacuum apparatus. A test tube containing the microorganism suspension is placed into a special rack (cassette) and the reagent card is placed in the neighbouring slot while inserting the transfer tube into the corresponding suspension tube. The cassette was placed into the VITEK 2 System and then automatically transported into a vacuum chamber station. After the vacuum is applied and air is re-introduced into the station, the organism suspension is forced through the transfer tube into micro-channels that fill all the test wells. The inoculated card is transferred mechanically and the instrument cuts off the transfer tube and seals the card prior to loading into the carousel incubator. The card is incubated on-line at 35.5 + 1.0 0C for 18-24 hours and removed from the carousel incubator once every 15 minutes, transported to the optical system for reaction readings and then returned to the incubator until the next reading. Data are collected at 15 minute intervals during the entire incubation period. A transmittance optical system allows interpretation of test reactions using different wavelengths in the visible spectrum. During incubation, each test reaction is read every 15 minutes to measure either turbidity or colour products of substrate metabolism. Additionally, a special algorithm is used to eliminate false readings due to small bubbles that may be present. Calculations are performed on raw data and compared to thresholds to determine reactions for each test. Each reagent card incubated in the machine is transferred to incubation and colorimetric reading sections and results interpreted automatically. The databases of the VITEK 2 system identification products are built with large strain sets of well-characterized microorganisms tested under various culture conditions. The strains are 43 derived from a variety of universal culture collections, ATCC, public, clinical and industrial sources. The readings from the test organism are compared to the respective database to determine a quantitative value for closeness to the database taxa. If a unique identification pattern is recognized, a list of possible organisms is given or the strain is determined to be outside the scope of the database and the API 20E kit is recommended (Pincus, 2006). The following manufacturer’s method of preparing the ID-GNB card, cassette and loading into the VITEK 2 system was adopted. Procedure 1. The VITEK 2 Gram-negative identification (ID-GNB) cards were taken out the refrigerator and allowed to achieve room temperature. 2. A carrier containing room for 14 tubes and 14 cards were placed. 3. The identity numbers of the assay preparation were manually entered in the “Accession number” field. 4. Two to three pure colonies from an overnight MacConkey or XLD agar plate (Selecta Media, South Africa) were suspended in 3 ml 0.85 % Sodium Chloride (BioMérieux, France) and the turbidity was measured using a DensiCheck Plus equipment and adjusted to 0.52 – 0.63 McFarland. 5. A control spread to check for contaminants (Purity plates) on MacConkey agar were performed on each bacterial suspension and plates aerobically incubated at 35 - 37°C for 18 – 24 hours. 6. The inoculum tubes were placed at the first positions. 7. The ID-GNB card barcode labels were scanned and the cards were placed in the card positions next to the inoculum tubes. 8. The Carrier containing the inoculum tubes and ID-GNB cards were placed in VITEK 2 where each test card was automatically filled with a bacterial suspension and automatic identification. The software then analysed the data and reported the results. 44 In this study, the assemblage of a grey carrier cassette containing and ID-GNB card (BioMérieux) and homogenous bacteria saline suspension in a tube (Fig. 2.3) was used. This IDGNB card contained 64 wells with each containing an individual test substrate to characterisation based on Substrates measuring various metabolic activities such as acidification, alkalinisation, enzyme hydrolysis, and growth in the presence of inhibitory substances. An optically clear film present on both sides of the card allows for the appropriate level of oxygen transmission while maintaining a sealed vessel. In all VITEK 2 system inconclusive characterization, API 20E strips (BioMérieux) was used to characterize in accords to BioMérieux (2008). Fig.2.3 The grey carrier container and ID-GNB card (BioMérieux, France). 2.7.3 The API 20E According to BioMérieux (2010), the API 20E system is a very highly reliable system needing no sophisticate equipment but an aerobic incubator, sterile test tube and pipette. It is used in food and clinical laboratories. The API-20E strip test kit for identification of enteric bacteria (BioMerieux, France) provides an easy way to inoculate and read tests relevant to members of the Family Enterobacteriaceae and other non-fastidious Gram-negative rods. The strip contains 20 micro tubes each containing dehydrated substrates. A bacterial suspension was used to rehydrate each of the wells and some wells change colour due to pH alteration while others produced end products that were identified with additional reagents. 45 The manufacturer’s method was adopted as follows: Procedure 1. The API 20E test kit was taken out the refrigerator and allowed to achieve room temperature. 2. A suspension of pure test organism was adjusted to 0.5 McFarland was prepared. 3. API 20E plastic strip holding twenty mini-test tubes was inoculated with a saline-test bacteria suspension according to manufacturer's directives. The following miniature tubes CIT, VP and GEL were filled completely and in ADH, LDC, ODC, H2S, URE tubes anaerobic conditions were created by overlaid each miniature tube with mineral oil. 4. Couple of drops of water were placed in the plastic grooves containing the strip to humidify the chamber, thereafter incubated for 18-24 hours at 37°C. 5. Purity plate was streaked out from each saline-test bacteria suspension. 6. The colour reactions were read (some with the aid of added reagents) and the reactions, plus the oxidase reaction done separately, were converted into a seven-digit code which is called the Analytical Profile Index, from which name the initials "API" are derived. 7. The code was entered onto the manufacturer's on-line database for identification to genus and species level and or compared with the data chart provided with the kit. The code is generated from the following sets of tests ONPG ADH LDC; ODC CIT H2S; URE TDA IND; VP GEL GLU; MAN INO SOR; RHA SAC MEL and AMY ARA. This grouping of tests used to generate the code is indicated by small arrow on the API 20E strip (Fig. 2.4) 46 Fig. 2.4 API 20E strip 2.7.4 Serological assays Following manufacturer’s recommendation, all VITEK 2 and or API 20E Shigella posivite strains were confirmed by slide agglutination assay using specific polyvalent antiserum (Pro-Lab Diagnostics, UK ) against O for groups A, B, C, and D. According to Pro-Lab (2012) Polyvalent Shigella antisera are intended to confirm initial serogrouping. Serological identification of Shigella involves mixing the suspected colony with antiserum containing specific Shigella antibodies and the reaction rocked for a minute. The bacteria will agglutinate (clump) in the presence of homologous antiserum. Antisera are prepared in rabbits using reference strains Pro-Lab Shigella antisera are supplied in dropper bottles containing 2.0 ml of ready-to-use sera. A step wise manufacture’s method was adopted as follows: Procedure All reagents were allowed to reach room temperature. 1. Two separate drops of saline were placed on a clean slide. 2. Onto each drop of saline, a Shigella colony was emulsified. 3. Of the two bacteria-saline emulsification suspension on the glass slide, a drop of saline was added to one and the other undiluted antiserum was added. 47 4. Both suspensions on the slide were gently rocked back and forth for one minute and agglutination was observed under normal light. A low power objective was used to read fine agglutination reactions. A distinct agglutination (granular clumping) within 60 seconds, without agglutination in the saline control (auto-agglutination) was considered a positive result. 2.8 Antimicrobial susceptibility testing The disc diffusion method, according to Clinical and Laboratory Standards Institute (CLSI) (2012) was performed to test susceptibility of all Shigella isolates. In brief, a 0.5 MacFarland standardized suspension of the bacteria in 0.85% sterile saline was prepared and swabbed over the entire surface of Mueller Hinton agar, after being allowed to reach room temperature, with a sterile cotton swab. After reaching room temperature, a ring of disks each containing single concentrations of each antimicrobial agent was then placed onto the inoculated surface and were incubated aerobically at 35- 37°C for 18 to 24hours. After overnight incubation at 35- 37°C, clear zones produced by antimicrobial inhibition of bacterial growth were measured (in millimetres) using a straight line ruler. The diameter of the zone was read using an interpreting chart (CLSI, 2012). The choice of antibiotic used in this study was based on frequently prescribed drugs in the area. For the susceptibility testing, the following antimicrobial drugs and concentrations were used: Ampicillin10μg, Augmentin 30μg, Azithromycin 10μg, Ceftriaxone 30μg, Ciprofloxacin 5μg, Co-trimoxazole 25μg and Tetracycline 30μg (Davies Diagnostics, South Africa). Findings of antibiotic resistance testing were recorded as susceptible, intermediate and resistant (CLSI, 2012). A fully susceptible Escherichia coli strain (ATCC 25922) was used as quality control in each batch of assay. 2.8.1 Detection of extended-spectrum β-lactamase (ESBL) ESBL production was detected by double disk synergy test (DDST) as described by CLSI (2012). All media and antibiotics used were allowed to reach room temperature before use. Mueller Hinton agar was inoculated with standardized inoculum (corresponding to 0.5 McFarland tube) using sterile cotton swab. An Augmentin (20 μg Amoxicillin and 10 μg of 48 Clavulanic acid) (AUG) disk was placed in the centre of the plate and 3rd generation Cephalosporins (CRO) Ceftriaxone 30 μg, disks was placed at 25 mm distance from the Amoxicillin-Clavulanic acid disk prior to incubation. The plate was incubated aerobically overnight at 37°C. In accordance with CLSI guidelines ESBL production is inferred when the zone of inhibition around the ceftrioaxone disc is expanded by the clavulanate in a “Keyhole” effect, or “Clavulanic” effect. 2.9 Statistical analysis The data collected were analysed using Statistical Package Statisca 7.1 software. Tables and percentages were used to describe findings and show relationship. Cross tabulations were used to examine the levels of drug resistance to the respective antibiotics. 49 Chapter Three The Results 50 Chapter Three The Results This study consisted of three phases of research. The first phase entailed seeding the stool samples onto agar plate, incubating in optimal conditions so as to yield single colonies. Second phase involved colony characterisation on VITEK 2 automated system or API 20E strips and followed by slide agglutination and thirdly, susceptibility testing of confirmed Shigella isolates. Regardless of quantity, the isolation of Shigella species is a significant finding indicating infection with the organism, therefore, each colony was examined carefully and all suspect isolates were confirmed biochemically. 3.1 Colonies Non-lactose fermenting 2 to 3 mm round and convex colonies on MacConkey and 1 to 2 mm round red-pink colonies on XLD (Fig.3.1 A and B) were seen after overnight incubation. These were picked for characterisation and confirmed as Shigella by biochemical and immunologically methods. The colonies were agglutinated with specific antisera for species differentiation (Fig. 3.2). A B Fig. 3.1: Non-lactose fermenting colonies on MacConkey Agar plate (A) and Red-pink colonies on XLD (B). 51 3.2 Serological results Based on the model of antigen antibody reaction depicted in Figure 3.2A, sero grouping detection of somatic O antigens by an agglutination technique with polyclonal antisera specific to each of the four Shigella species (group A, B, C or D) resulted in positive tests (Figure 3.2B). The suspension on slide position 1 indicate a negative reaction and granular clumping seen in position 2 and 4 show a positive reaction. Depending on the name of group of antisera used, where agglutination occurred, colonies were named as such. Negative test. Positive test A B Fig.3.2 Model basis of antigen-antibody reaction (A) Slide agglutination test results (B) 3.3 Isolates and species distribution During the study period, from total of 11009 stool specimens examined 110 Shigella isolates were recovered. The Shigella incidences were essentially driven by S. sonnei accounting for 59% (10/17) in January, 38% (9/24) in February, 59% (27/46) in March and 65% (15/23) in April and overall accounted for 55% (61/110). This was followed by S. flexneri (43% (47/110). Single cases each of S. boydii and S. dysenteriae (1% (1/110) were recovered (Table 3.1). 52 Table 3.1 Monthly and gender infection distribution of Shigella serogroups isolated from human 17 13 Male female Male female Male Female Male Female February 2753 24 17 March 2588 46 41 April 3150 23 18 Total 11009 110 89 Shigella serogroups 1 1 1 1 S. Sonnei 2518 gender S. Flexneri January Total isolates from ≤ 10 yrs. old S. dysenteriae Total stools cultured S. Boydii Months Total isolates stool specimens from January to April 2013. 4 3 9 5 9 9 3 5 47 6 4 4 5 11 16 6 9 61 Total infected male female 10 7 14 10 20 26 9 53 14 57 The overall infection incidences between the genders showed females (n=57) to be more infected than the male (n=53). In January 59% (10/17) males compared to 41% (7/17) females and February 58% (14/24) males contrast to 42% (10/24) females were infected. However, we cannot explain the reverse in incidences count that showed a female dominancy in March 43% (20/46) males to 57% (26/46) females and April 39% (9/23) males to 61% (14/23) females. The high number of cases in March may have influenced the overall tilt to females being more infected (Table 3.1). The monthly distribution of stool specimens examined (Table 3.1) showed highest number of specimens in April while January had the lowest. The number of specimens showed a progressive increase from January to April. Monthly number of isolates was observed to be highest in March, lowest in January while nearly identical trends in February and April (Fig. 3.3). 53 50 46 45 no. of isolates 40 35 30 25 24 23 20 17 15 10 5 0 January February March April Fig. 3.3 Monthly isolates distribution during the month of study. The infection age distribution ranged from 22 days to 94 years with the median being 3 years old from children below 10 years old. Similar to other parts of the world (WHO, 2005), children below 5years have the highest incidences. In this study there were 69% (76 /110) cases followed by 6 to 10years age group 12% (3/110). All aged in this study were vulnerable to Shigella infection (Table 3.2). Table 3.2 Distribution of Shigellosis cases according to age-group Age groups S. boydii <1-5 6-10 11-20 21-30 31-40 41-60 +61 1 total 1 S. dysenteriae 1 S. flexneri S. sonnie total 29 7 2 2 47 5 2 2 2 2 1 76 13 4 4 2 9 2 61 110 7 1 47 54 3.4 Susceptibility Test Results Determination of bacterial resistance to antimicrobials is an important part of the management of infections in patients. Resistance was determined by growth around the disc and clearing of growth conforming CLSI guidelines was accepted as susceptible as depicted in Figure 3.4 Fig. 3.4 Disc diffusion results. The disc diffusion results of 110 isolates tested for antibiotic susceptibility (Table 3.3) show 13% (14/110) of strains were fully susceptible to all antibiotics. The monthly distribution of resistant and susceptible strains is shown in Table 3.4. Of the 96 strains, the following resistance patterns frequency was exhibited towards Co-trimoxazole (83%), Tetracycline (71%), Ampicillin (27%) and 5% towards Augmentin (AUG) (Amoxicillin/clavulanic acid) and 2% to zithromycin. Towards third generation cephalosporin viz. Ceftriaxone (CRO) and fluoroquinolone viz. Ciprofloxacin (CIP) we observed a nil resistance. Strains resistant to two, three and or four antibiotics are shown in Table 3.3. A significant number of strains were resistant to single drugs of Co-trimoxazole (SXT) (n=91) and Tetracycline (n=77). Likewise, 68% (n=75) strains were resistant to both Co-trimoxazole and Tetracycline, 26% (n=29) to Ampicillin (AMP), Cotrimoxazole and Tetracycline (TE) while only two strains showed resistance to four drugs viz Ampicillin, Azithromycin (AZM), Co-trimoxazole and Tetracycline The single Shigella boydii isolated in this study demonstrated a full susceptibility to all antibiotics while Shigella dysenteriae demonstrated resistance toward Ampicillin, Cotrimoxazole and Tetracycline. 55 Table 3.3 Antimicrobial resistance test results for Shigella strains Antibiotic agent Study months January February (n=17) (n=24) March (n=46) April (n=23) Total resistance (n=110) 4(24) 1(6) 1(6) 0 0 14(82) 15(88) 5(19) 2(8) 0 0 0 19(79) 15(63) 14(30) 3(7) 1(2) 0 0 40(87) 32(70) 7(30) 1(4) 0 0 0 18(78) 15(65) 30(27) 7(6) 2(2) 0 0 91(83) 77(70) SXT, TE 14(82) 15(63) AM,SXT,TE 4(24) 6(25) AM, AUG,SXT, TE 1(6) 1(4) AZM, AM, SXT, TE 1(6) 0 Fully susceptible 2 2 Note: Numbers in the parenthesis show percentage; 32(70) 14(30) 3(7) 1(2) 6 14(61) 5(22) 1(4) 0 4 75(68) 29(26) 6(5) 2(2) 14(13) Disc potency (μg) AMP AUG AZM CRO CIP SXT TE 10 20/10 10 30 5 25 30 Resistance to Ampicillin, Augmentin, Azithromycin, Co-trimoxazole and Tetracycline over the study period was largely by S. sonnei followed by S. flexneri (Table 3.4). Table 3.4 Monthly distributions of antibiotic resistant Shigella strains Months January organisms S. flexneri S. sonnie February S. flexneri S. sonnie March S. flexneri S. sonnie S. dysenteriae April S. flexneri S.sonnei SXT (n=13) 3 10 (n=19) 10 9 (n=41) 14 26 1 (n=18) 5 13 TE (n=15) 5 10 (n=15) 8 7 (n=32) 11 20 1 (n=15) 3 12 Total 91(83) 77(70) Note: Numbers in the parenthesis show percentage. 56 Antibiotic agents Aug AZM (n=1) (n=1) 0 1 1 0 (n=2) (n=0) 2 0 (n=3) (n=1) 2 0 1 1 (n=1) (n=0) 1 7(6) 2(2) AMP (n=4) 3 1 (n=5) 3 2 (n=14) 8 5 1 (n=7) 4 3 30(27) Chapter Four DISCUSSION 57 Chapter Four Discussion 4.1 Prevalence The prevalence rate of isolating Shigella 1% (110 /11009) observed in the study may be due, in part, to continuing educational programmes especially at elementary schools, aggressive infection-control measures and possibly patients being on antibiotics before submitting stools for culture. The study group involved people with medical aid schemes (paying patients) and head of house hold is anticipated to be educated. Challenges of overcrowding, poor sanitation, malnutrition and lack of clean water are not always synonymous with an educated population. No outbreak was reported during the study period. Highest Shigella yield was noticed in March. There was a shift from estimated average of 21 isolates per month to more than double (n=46) in March. The shift may be influenced by increase in stools examined from children below 10 years (Table 4.1) which contributed 81% of the studied. This endorses the fact that shigellosis is mainly a childhood disease (Niyogi, 2005). Children’s vulnerability may be attributed to immature immune system, un-programmed immune system due to lack of previous exposure and exposure to contaminated environment due to their play-related activities. Findings of predominant species have important implications for treatment and prevention strategies. In most developing countries, S. flexneri is the predominant Shigella serogroup isolated from stool of patients with infectious diarrhoea (WHO, 2009). Our findings deviate yet agree with reports where the predominant serogroup is S. sonnei (n=61) and followed by S. flexneri (n=47). All four serogroups co-exist in different proportions in our study region (Table 3.1). In contrast to global prevalence of untypeable isolates of Shigella (Zafar et al., 2009), all our isolates agglutinated with specific antisera. Dominancy of S. sonnei has been noted in other cities globally, in USA (Sivapalasingam et al., 2006) and Asian countries (Qu et al., 2012). Nevertheless, some studies suggest S. flexneri is more prevalent in tropical countries. Serogroup A (S. dysenteriae) (n=1) and serogroup C (S. boydii) (n=1) isolation frequency was low in present study. Not surprisingly, this is consistent with previous reports (Keddy et al., 2010; Smith et al., 2009) of isolates from the public healthcare system in South African. The low isolation rate could be because sero-group A is commonly associated with and cause large 58 dysentery outbreaks (WHO, 2005), however, S. boydii (serogroups C) is generally the least frequently isolated of Shigella strains. It is typically associated with individuals who have travelled to endemic areas as equally observed in other studies (Smith et al., 2009; Efuntoye et al., 2011). However, due to low isolation rate in this study, incidence of these serotypes in the private healthcare system can be ascertained by longer surveillance studies. However, it is not unusual for one serogroup to replace another in the community from time to time. The comparative dominancy of serogroups fluctuates with time, hygienic conditions and different in population. The Shigella isolates prevalence rate variation in Ethiopia (Astrat, 2008) and some parts of the world seem to alternate mainly between S. flexneri, and S. sonnie as the most active agents of shigellosis. Antimicrobial therapy is the cornerstone for treatment of shigellosis for reasons of shortening severity and duration of illness, reduce shedding of the organisms and prevent subsequent infection by family contacts, development of secondary complications and death. The guiding principle for the choice of antimicrobial in developing countries like South Africa is cost and availability of drugs. USA (Sivapalasingam et al., 2006) and studies of the public healthcare system in South Africa (Keddy et al., 2010), agree with our findings of ceftriaxone and ciprofloxacin being 100% potent over four months. Our study shows an increase in strains resistant to ampicillin, Augmentin and Co-trimoxazole while random resistance to Azithromycin was observed. Both S. flexneri and S. sonnie demonstrated resistance to azithromycin unlike Talukder et al. (2006) Bangladesh studies were 100% susceptibility was demonstrated. Tetracycline resistance pattern was constant for January, February and April while an increase in resistance for a corresponding increase in isolates was observed in March. S. flexneri and S. sonnei were resistant to Co-trimoxazole and Tetracycline. This could probably be a resultant of indiscriminate use of these antimicrobial agents for therapeutic purposes in human, veterinary science and horticulture that eventually lead to the development of antibiotic resistance. ESBL-producing Shigella pose a distinctive test to clinical microbiologists, clinicians, infection control professionals and scientists tasked in finding new drugs. ESBL-producing strains are usually found in hospitals where antibiotic use is frequent and the patients are critical. In spite of high prevalence of resistant strains, ESBL production associated with S. flexneri and S. sonnei 59 previously seen in South Africa between 2003 to 2009 (Tau et al., 2012) was not observed in our study. However, ESBL producing isolates have been observed elsewhere such as in Nigeria (Efuntoye et al., 2011). Observed in our studies, though, is the growing number [n=7 (6%)] of strains resistant to beta-lactam/ beta- lactamase inhibitor, Augmentin (Amoxacillin-Clavulanic acid) which could eventually pose as a threat in therapy programmes. We noticed a portion of stool samples where Shigella species were isolated were not bloody diarrhoea stools. This could then mean diagnosis and therapy based on bloody stool for shigellosis could miss some cases. These findings confirm the need to formulate long-term surveillance programmes that would identify changes in antimicrobial susceptibility patterns and the dissemination of such formation to clinicians, scientists and all involved with human health care. 4.2 Conclusion The findings clearly highlight the occurrence of the four species of Shigella in the private health care system serviced by Lancet laboratories. The presence of this human enteric pathogen in Johannesburg communities could have significant public health implications, particularly among the immunocompromised (HIV/AIDS patients), elderly and children who are at greater risk. As there was no Shigella outbreak during the present study, an average of 2752.25 (11009/4) stools assayed each month a yielded of 27.5 isolates of which isolate distribution was 15.25 S. Sonnei, 11.75 S. flexneri and 0.5 S. boydii and S. dysenteriae respectively. This size of isolate yield represents a significant number of Shigella strains isolatable form human stools and a possible source for an outbreak. Children, particularly those below five years old, were found to be the most infected. This could suggest limitation in hygiene knowledge, particularly on the communicability of shigellosis. Children above five years and adults may need to be educated on the dangers of unhygienic practice such as not washing hands with soap after using the toilet and consumption of suspiciously contaminated or soiled foods to avoid spread of Shigella bacteria. 60 4.3 Limitations Investigation of Laboratory-Based Surveillance of Shigella, its Serotype and Resistance Patterns in Johannesburg, South Africa depended on the healthcare-seeking behaviour of individual patients and the clinician discretion to request stool culture. Thus, the result may not represent the asymptomatic cases in the community. It was not possible to identify up to serotypes level due to budget constraints Not all health care centres provided faeces for analysis, therefore, this study depicts presence or absence of shigellosis in areas where stool samples were received and cultured for Shigella. 4.4 Recommendations It is paramount to reduce and or completely eradicate the levels of infection that threaten human health in all communities, including this area of study, through knowledge based managerial strategies. Therefore, a combination of the following factors if implemented may be helpful: The current state of the municipality’s potable water supply systems must be inspected, and constantly tested for the possibility of being a vehicle for the transmission of bacteria. Infrastructure on waste and faecal disposal systems must be constantly evaluated and monitored to ensure optimal operation. Policies on food vending must be periodically re-evaluated to ensure adherence to food safety accreditation requirements and emphasis on correct hygiene practices could help limit the spread of bacterial infections, particularly Shigella. Surveillance laboratory data on food and water borne isolates should be published more frequently so as to help policy makers to measure the effectiveness of policies and implementation remedial instructions. As this study represents data collected in the first four months of the year, further work needs to be undertaken to establish whether Shigella strains are present in this society 61 throughout the changing seasons of the year. The seasonal presence of S. dysenteriae sero variants would be of particular importance not only for the severe form of the disease but to develop and evaluate preventative strategies that may avert a catastrophic outbreak. In the wake of increasing microbial drug resistance, up-to-date antibiogram profile, which is empirical in patient management, should be developed by continuously evaluating Shigella species response to antibiotics and an easily accessed database should be developed. Specific bacteriophages against Shigella species should be investigated in order to uncover alternative treatment regimes. Phylogenetic studies of Shigella isolates must be performed so as to ascertain the isolates’ clonal/ genetically relationship so as to help trace the source of infection. This will help formulation of specific area related remedial actions. 62 Chapter Five REFERENCES 63 5.0 References Asrat, D. (2008). Shigella and Salmonella serogroups and their antibiotic susceptibility patterns in Ethiopia, Eastern Mediterranean Health Journal, 14(4): 760-767. Bagamboula, C.F., Uyttendaele, M., Debevere, J. (2002). Acid tolerance of Shigella sonnei and Shigella flexneri. Journal of Applied Microbiology 93:479–486. Bardhan, P., Faruque, A. S., Naheed, A. and Sack, D. A. (2010). Decrease in shigellosis-related deaths without Shigella spp.-specific interventions, Emerging Infectious Diseases--Southeast Asia 16, 1718–1723. Available at: http//www.ncbi.nlm.nih.gov/pmc/articles/PMC2640118. (Accessed 17th July, 2013). BioMérieux. (2010). API 20 E: Identification system for Enterobacteriaceae and other nonfastidious Gram-negative rods. http://site.iugaza.edu.ps/mlaqqan/files/2012/04/Api20E1.pdf (Accessed 25th June, 2013). BioMérieux. (2008). Antibiotic Classification and Modes of Action. Available at http://www.biomerieux-usa.com/upload/VITEK-Bus-Module-1-Antibiotic-Classification-andModes-of-Action-1.pdf. (Accessed 23rd September, 2013). BIO Ventures for Global Health. (2011). Neglected Disease Pipeline > Diseases > Shigellosis: global burden. Available at: http://www.bvgh.org/Biopharmaceutical-Solutions/Global-HealthPrimer/Diseases/cid/ViewDetails/ItemID/13.aspx (Accessed 25th June 2013). Boucher, Y., Labbate, M., Koenig, J.E., Stokes, H.W. (2007). Integrons: mobilizable platforms that promote genetic diversity in bacteria. Trends Microbiology 15: 301– 309. Brink A.J., Moolman, J., Cruz da Silva, M. (2007). The National Antibiotic Surveillance Forum. Antimicrobial susceptibility profile of selected bacteraemic pathogens from private institutions in South Africa. South Africa Medical Journal; 97:630-636. 64 Burrowes, B., Harper, D.R., Anderson, J., McConville, M. and Enright, M.C. (2011). Bacteriophage therapy: Potential uses in the control of antibiotic-resistant pathogens. Expert Review of Anti-Infective Therapy; 9(9): 775-85. Cabral, P.S. (2010). Water Microbiology. Bacterial Pathogens and Water. International journal Environment Research and Public Health. 7(10): 3657–3703. Available at: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2996186/ (Accessed 11th May 2013). Castillo, A., Villarruel-López, A., Navarro-Hidalgo, V., Martínez-González, N.E. and TorresVitela, M.R. (2006). "Salmonella and Shigella in freshly squeezed orange juice, fresh oranges, and wiping cloths collected from public markets and street booths in Guadalajara, Mexico: incidence and comparison of analytical routes." Journal of Food Protection. 69 (11): 2595-2599. Available at: http://www.ncbi.nlm.nih.gov/sitse/entrez?cmd=Retrieve&db=pubmed&dopt=Abstract&list_uids =17133801 (Accessed 12th July 2013). CDC. (2013). Shigellosis: General Information - NCZVED Available online at http://www.cdc.gov/nczved/divisions/dfbmd/diseases/shigellosis/ (Accessed 10th July, 2013). CDC. (2012. Nutrition for everyone: Fruits and Vegetables. Available at: http://www.cdc.gov/nutrition/everyone/fruitsvegetables/index.html (Accessed 25th June, 2013) CDC. (2010). “Preliminary FoodNet Data on the Incidence of Infection with Pathogens Transmitted Commonly through Food—10 States, 2009,” MORBIDITY AND MORTALITY WEEKLY REPORT. 59(14):418-22. Available at: http://www.cdc.gov/mmwr/preview/mmwrhtml/mm5914a2.htm (Accessed 23rd August, 2013). CDC. (2009. National Centre for Emerging Zoonotic, infectious Diseases (NCEZID) “Shigellosis.” Available at: http://www.cdc.gov/nczved/divisions/dfbmd/diseases/shigellosis/ (Accessed 13th March 2013) 65 Chakrabarti, L.A. (2010). Immune mechanisms of HIV control. Current Opinion Immunology; 22(4): 488–496. Cheesbrough M. (2006). District Laboratory Practice in Tropical Countries Part 2 Second Edition. part 2. Cambridge: University Press. Clinical Laboratory Standards Institute (CLSI). (2012). Performance standards for antimicrobial disk susceptibility tests; twenty-second informational supplement. CLSI document M100-S22. Wayne, P.; Clinical Laboratory Standards Institute. Committee on Infectious Diseases American Academy of Pediatrics (CIDAAP). (2009). Shigella infections: Red Book 2009 Report of the Committee on Infectious Diseases. 28th ed. Elk Grove Village, IL: American Academy of Pediatrics; 593-596. http://wwwnc.cdc.gov/travel/yellowbook/2012/chapter-3-infectious-diseases-related-totravel/shigellosis.htm (Accessed 19 June 2013). Cowley, M. and Oakey, R.J. (2013). Transposable Elements Re-Wire and Fine- Tune the Transcriptome. PLoS Genet 9(1): e1003234. doi: 10.1371/journal.pgen.1003234. Crowther-Gibson, P., Govender, N., D A Lewis,D.A., Bamford, C., A Brink, A., von Gottberg, A., Klugman, K., du Plessis, M., Fali, A., Harris, B., K H Keddy, K.H. and Botha, M. (2011). Human infections and antibiotic resistance, South African Medical Journal; 101(8):567- 577. Daskalakis, D.C. and Blaser, M.J. (2007). Another Perfect Storm: Shigella, Men Who Have Sex with Men, and HIV Clinical Infectious Diseases. 44:335–337. Domingues, S., Harms, K., Fricke, W.F., Johnsen, P.J., da Silva, G.J., and Nielsen, K.M. (2012). Natural Transformation Facilitates Transfer of Transposons, Integrons and Gene Cassettes between Bacterial Species. PLoS Pathog 8(8): e1002837. doi:10.1371/journal.ppat.1002837. 66 Drews, S. J., Lau, C., Andersen, M., Ferrato, C., Simmonds, K., Stafford, L., Fisher, B., Everett, D. and Louie, M. (2010). Laboratory based surveillance of travel-related Shigella sonnei and Shigella flexneri in Alberta from 2002 to 2007. Global Health 1;6:20. doi: 10.1186/1744-8603-620. Efuntoye,M.O. and Adenuga, A. (2011). Shigella serotypes among nursery and primary school children with diarrhoea in Ngo-Iwoye and Ijebu-Igbo, southwestern Nigeria. Available at: http://www.arpapress.com/Volumes/JPCS/Vol2/JPCS_2_07.pdf (Accessed 23th May, 2013). Farag, T.H., Faruque, A. S., Wu, Y., Das, S.K., Hossain, A., Ahmed, S., Ahmed, D., Nasrin, D., Kotloff, K. L., Panchilangam, S., Nataro,J.P, Cohen, D., Blackwelder, W. C., and Levine, M .M. (2013) Housefly Population Density Correlates with Shigellosis among Children in Mirzapur, Bangladesh: A Time Series Analysis. PLoS Neglected Tropical Diseases 7(6): e2280. doi:10.1371/journal.pntd.0002280. Fhogartaigh, C.N. and Edgeworth, J.D., (2009). Bacterial gastroenteritis. Medicine, 37 (11), 586593. Ghosha, M., Wahia, S., Mukesh Kumara M. and Gangulia A. (2007). Prevalence of enterotoxigenic Staphylococcus aureus and Shigella spp. in some raw street vended Indian foods. International Journal of Environmental Health Research; 7(2) 151-156. Gillings, M., Boucher, Y., Labbate, M., Holmes, A., Krishnan, S., Marita Holley,M., and Stokes, H.W. (2008) The evolution of class 1 integrons and the rise of antibiotic resistance. Journal of Bacteriology, 190: 5095–5100. Godoy, P., Bartolomé, R., Torres, J., Espinet, L., Escobar, A., Nuin, C., Domínguez, A. (2011). Waterborne outbreak of Shigella sonnei caused by consumption of public supply water. Gaceta Sanitaria, 25(5):363-367. Goodridge, L. D. (2013). Bacteriophages for managing Shigella in various clinical and nonclinical settings. Bacteriophage; 3:e25098. Available at: http://dx.doi.org/10.4161/bact.25098 Guo, X., Xia, R., Han, N. and Xu, H. (2011), Genetic diversity analyses of class 1 integrons and their associated antimicrobial resistance genes in Enterobacteriaceae strains recovered from aquatic habitats in China. Letters in Applied Microbiology, 52: 667–675. 67 Gupta, A. and Polyak, C. (2004). Laboratory-Confirmed Shigellosis in the United States, 19892002: Epidemiologic Trends and Patterns. Clinical Infectious Diseases; 38:1372-1377. Hale, T. L. (1991). Genetic basis of virulence in Shigella species. Microbiological reviews, 55: 206- 224. Hale, T.L. and Bonventre, P.F. (1979). Shigella infection of Henle intestinal epithelial cells: role of the bacterium. Infection and Immunity; 24(3): 879–886. Hao, W., Allen, V.G., Jamieson, F.B., Low, D.E., Alexander, D.C. (2012). Phylogenetic Incongruence in E. coli O104: Understanding the Evolutionary Relationships of Emerging Pathogens in the Face of Homologous Recombination. PLoS ONE 7(4): e33971. doi:10.1371/journal.pone.0033971. Hassan, A. N., Farooqui, A., Khan, A., Khan, A.Y. and Kazmi, S.U. (2010). Microbial contamination of raw meat and its environment in retail shops in Karachi, Pakistan. Journal of Infection in Developing Countries; 4(6):382-388. He, F., Han, K., Liu, L., Sun, W., Zhang, L., Zhu, B. and Ma, H. (2012). Shigellosis: Outbreak Associated with Contaminated Well Water in a Rural Elementary School: Sichuan Province, China, June 7–16, 2009, PLoS One; 7(10): e47239. Heier, B.T., Nygard, K., Kapperud, G., Lindstedt, B.A., Johannessen, G.S., Blekkan, H. (2009). Shigella sonnei infections in Norway associated with sugar peas, May-June 2009. Euro Surveillance: 14(24):218-226. Hodges, K. and Gill, R. (2010). Infectious diarrhoea Cellular and molecular mechanisms, Gut Microbes 1(1): 4-21. Igumbor, E.O., Obi, C.L., Bessong, P.O., Potgieter, N., Mkasi, T.C., (2007). Microbiological analysis of banknotes circulating in the Venda region of Limpopo province, South Africa. South Africa journal of Science. 103 (9)10: 365-366. 68 Islam, M.S., Hossain, M.A., Khan, S.I., Khan, M.N.H., Sack, R.B., Albert, M.J., Huq, A., Colwell, R.R. (2001). Survival of Shigella dysenteriae type 1 on fomites. Journal of Health, Population and Nutrition, 19(3):177–182. Jiménez, K.B., McCoy, C.B. and Achi, R. (2010). Detection of Shigella in lettuce by the use of a rapid molecular assay with increased sensitivity, Brazilian Journal of Microbiology 41: 9931000. Keddy,K.H., Sooka, A., Crowther-Gibson, P., Quan, V., Meiring, S., Cohen, C., Nana, T., Sriruttan, C., Seetharam, S., Hoosen, A., Naicker, P., Elliott, E., Haffejee, S., Whitelaw, A., and Klugman,K.P. (2012). Systemic shigellosis in South Africa, Clinical Infectious Diseases, 54(10):1448 -1454. Keddy, K.H. (2010). The group for enteric, respiratory and meningeal disease surveillance in South Africa. Communicable Disease Surveillance Bulletin. 8(2):38-40. Available at: http://www.nicd.ac.za/ pubs/survbull/2011/CommDisBull May 2011.pdf. (Accessed 25th Januarys, 2013). Keenan, K.P., Sharpnack, D.D., Collins,H., Formal,S.B and O'Brien, A.D. (1986). Morphologic evaluation of the effects of Shiga toxin and E. coli Shiga-like toxin on the rabbit intestine. American Journal of Pathology; 125(1): 69–80. Kotloff K., Clemen. J.,and Key B. (1999b). Generic protocol to estimate the burden of Shigella diarrhoea and dysentreal mortality. Department of vaccine and Biologicals,WHO/V & B/99.26. Kutateladze, M. and Adamia, R. (2010). Bacteriophages as potential new therapeutics to replace or supplement antibiotics. Trends Biotechnology; 28(12): 591–595. Kramer, A., Schwebke, I., and Kampf, G. (2006). How long do nosocomial pathogens persist on inanimate surfaces? A systematic review. BMC Infectious Diseases, 6: 130. doi:10.1186/14712334-6-130 Available at: http://www.biomedcentral.com/content/pdf/1471-2334-6-130.pdf (Accessed 30th April 2012). 69 Lan, R. and Reeves P.R. (2002) Escherichia coli in disguise: molecular origins of Shigella Microbes and Infection 4; 1125–1132. Available at: http://www.emi.unsw.edu.au/~lanlab/public/publications/RL24.pdf (Accessed 10th July, 2013). Lehmann, M.J., Sherer, N.M., Marks, C.B., Pypaert, M., and Mothes, W. (2005). Journal of cell Biology; 170, 317–325. Le Faou, A. (2010). Prevalence of shigellosis diarrhoea in a paediatrics population: hospital based survey in Bangui, Central African Republic. Journal of Infection in Developing Countries; 4(10):655- 657. Lefebvre, J., Gosselin, F., Ismail, J., Lorange, M., Lior, H., and Woodward, D. (1995). Evaluation of Commercial Antisera for Shigella Serogrouping, Journal of Clinical Microbiology, 33:1997-2001. Li, Y., Cao, B., Liu, B., Liu,D., Gao, O., Peng, X., Wu, J., Bastin, D.A., Feng, L., and Wang, L. (2009). Molecular detection of all 34 distinct O-antigen forms of Shigella, Journal of Medical microbiology, 58(1):69-81. Madiyarov,R.S., Bektemirov, A.M., Ibadova, G.A., Abdukhalilova, G.K. Aybek V Khodiev, A.V, Bodhidatta, L., Orntipa Sethabutr, O. and Mason. C. J. (2010). Antimicrobial resistance patterns and prevalence of class 1 and 2 integrons in Shigella flexneri and Shigella sonnei isolated in Uzbekistan. Gut Pathogens, 2:18 doi:10.1186/1757-4749-2-18. Makhubu, N. 2012. “Deadly infection investigated”,_ Pretoria News_25th April_ p1 Mamatha, B., Pusapati, B.R., Rituparna, C. (2007). Changing patterns of antimicrobial susceptibility of Shigella serotypes isolated from children with acute diarrhoea in Manipal South India, a 5-year study. Southeast Asian Journal of Tropical Medicine Public Health; 38: 863-866. Man, A.L., Prieto-Carcia,M.E. and Nicoletti,C. (2004). Improving MC mediated transport across mucosal barrier: do certain bacteria hold the key? Immunology, 113, 15-22. 70 Mandomando, I., Sigauque, B., Valles, X. (2007). Epidemiology and clinical presentation of Shigellosis in children less than five years of age in rural Mozambique. Pediatric Infectious Diseases Journal. 26(11):1059-1061. Available at: http://www.ajtmh.org/content/76/3/522.full.pdf+html (Accessed 25th May, 2013). Metzler, J. and Nachamkin, I. (1988). Evaluation of a latex agglutination test for the detection of Salmonella and Shigella spp. by using broth enrichment. Journal of clinical Microbiology 26(12): 2501–2504. Moselakgomo, A.2007. “Diarrhoea outbreak in Delmas”,_ Sowetan live_31st Oct., http://www.sowetanlive.co.za/sowetan/archive/2007/10/31/diarrhoea-outbreak-in-delmas (Accessed 25th March, 2012). Murayama, S.Y., Sakai, T., Makino, S., Kurata, T., Sasakawa, C. and M Yoshikawa M. (1986). The use of mice in the Sereny test as a virulence assay of Shigellae and enteroinvasive Escherichia coli. Infection and Immunity; 51(2): 696–698. Nakamura, M. (1962). The survival of Shigella sonnei on cotton, glass, wood, paper and metal at various temperatures. Journal of Hygiene 60:35–39. Nealer, E., Bertram, E., van Eeden, E., van Nierkerk, D., Tempelhoff, J and Coetzee C. (2009). Addressing issue of epidemiological disaster: Obervations on Delmas water-based crisis 19932007. Available at: http://acds.co.za/uploads/research_reports/Delmas_Ver1.pdf (Accessed 25th May 2012). Nicolo, M.S., Gioffre, A., Carnazza, S., Platania, G., Di Silvestro, I., Guglielmino, S.P.P. (2011) Viable but nonculturable state of foodborne pathogens in grapefruit juice: A study of laboratory. Foodborne Pathogens and Disease 8(1):11–17. 71 Niyogi, S.K.(2005). Shigellosis. Journal of Microbiology. 43:133-43. Available at: http://www.msk.or.kr/jsp/downloadPDF1.jsp?fileName=p.133-1430.pdf (Accessed 20th July, 2012). Obi, C.L., Ramalivhana, J., Momba, M.N.B., Onabolu, B., Igumbor, J.O., Lukoto M., Mulaudzi, T.B., Bessong, P.O., Jansen van Rensburg, E.L., Green, E. and Ndou, S: (2007). Antibiotic resistance profiles and relatedness of enteric bacterial pathogens isolated from HIV/AIDS patients with and without diarrhoea and their household drinking water in rural communities in Limpopo Province South Africa: African Journal of Biotechnology. 6 (8): 1035-1047. Ojha,S.C., Yean,C.Y., Ismail, A., and Kirnpal-Kaur Banga Singh, K.B.(2013). A Pentaplex PCR Assay for the Detection and Differentiation of Shigella Species. BioMed Research International, 2013: 9. Avalaible at: http://dx.doi.org/10.1155/2013/412370 accessed 9th September, 2013. Opintan, J.A. and Newman, M.J. (2007). Distribution of Serogroups and Serotypes of Multiple Drug Resistant Shigella Isolates. Ghana Medical journal, 41(1): 8–29. Pazhani, G.P., Niyogi, S.K., Singh. A.K., Sen, B., Taneja, N., Kundu, M., Yamasaki, S., Ramamurthy, T. (2008). Molecular characterization of multidrug-resistant Shigella species isolated from epidemic and endemic cases of shigellosis in India. Journal of Medical Microbiology; 57: 856-863. Peng, J., Zhang, X., Yang, J., Wang, J., Yang, E., Bin W., Wei C., Sun, M. and Qi Jin, Q. (2006). The use of comparative genomic hybridization to characterize genome dynamics and diversity among the serotypes of Shigella, BioMed Central journals, 7:218. http://www.biomedcentral.com/1471-2164/7/218 72 (Accessed 20th July, 2013). Available at: Perry, J.D. and Freydière, A.M. (2007). The application of chromogenic media in clinical microbiology. Journal of Applied Microbiology, 103(6) 2046-2055. Pieper R., Zhang, Q., Parmar P.P., Huang, S.T., Clark, D.J., Alami, H., Donohue-Rolfe, A., Fleischmann, R.D., Peterson, S.N. and Tzipori, S. (2009). The Shigella dysenteriae serotype 1 proteome, profiled in the host intestinal environment, reveals major metabolic modifications and increased expression of invasive proteins. Proteomics 2009, 9(22):5029-5045. Pillay, D.G., Karas, A.J. and Sturm, A.W. (1997). An outbreak of Shiga bacillus dysentery in KwaZulu/Natal, South Africa, Journal of Infection; 34(2):107-111. Pincus, D. H. (2006). Microbial Identification using the BioMerieu Vitek 2 System. Available at: https://store.pda.org/bookstore/.../ERMM_V2_Ch01.pdf (Accessed 06th March, 2013). PRO-LAB Diagnostics. (2012). Shigella Slide Agglutination Antisera. http://www.pro-lab.com/inserts/Shigella.pdf (Accessed 3rd October, 2013). Available at: Qu, F., Bao, C., Chen, S., Cui, E., Guo, T., Wang, H., Zhang, J., Wang, H., Tang, Y.W., Mao, Y. (2012) Genotypes and antimicrobial profiles of Shigella sonnei isolates from diarrhoeal patients circulating in Beijing between 2002 and 2007. Diagnostic Microbiology and Infectious Disease; 74(2):166-170. Ram, P.K., Crump, J.A., Gupta, S.K., Miller, M.A. and Mintz, E.D. (2008). Part II. Analysis of data gaps pertaining to Shigella infections in low and medium human development index countries, 1984–2005 Epidemiology and Infection, 136(5): 577–603. Ramos-Moreno, A.C., Gonc¸ L., Ferreira, A. and Martinez, M.B. (2009). Enteroinvasive Escherichia coli vs. Shigella flexneri: how different patterns of gene expression affects virulence. Federation of European Microbiological Societies 301(2): 156–163. Ray, K., Marteyn, B., Sansonetti, P.J., and Tang, C.M. (2009). Life on the inside: the intracellular lifestyle of cytosolic bacteria. Nature Reviews Microbiology. 7(5): 333–340. 73 Romero, S., Grompone, G., Carayol, N., Mounier, J., Guadagnini, S., Prevost, M.C., Sansonetti, P.J., and Tran Van Nhieu, G. (2011). ATP-Mediated Erk1/2 Activation Stimulates Bacterial Capture by Filopodia, which Precedes Shigella Invasion of Epithelial Cells. Cell Host Microbe 9(6): 508–519. Rowe-Magnus, D.A., Guerout, A.M., and Mazel, D. (2002). Bacterial resistance evolution by recruitment of super-integron gene cassettes. Molecular Microbiology; 43(6): 1657–1669. Schroeder, G.N. and Hilbi H. (2008). Molecular pathogenesis of Shigella spp.: controlling host cell signaling, invasion and death by type III secretion. Clinical Microbiology Reviews. 21(1): 134-156. Singh, K. (2009). Laboratory-acquired infections. Clinical Infectious Diseases, 49(1): 142-7 Smith, A.M., Keddy, K.H., Sooka, A., Ismail, H., Dejong, G.M. (2009). Analysis of a temporal cluster of Shigella boydii isolates in Mpumalanga, South Africa, November to December 2007. Journal of Infection in Developing Countries; 3(1):65-70. Sivapalasingam, S., Nelson,J.M., Joyce, K., Hoekstra, M. Angulo,F.J. and Mintz, E.D. (2006). High prevalence of antimicrobial resistance among Shigella isolates in the United States by the national antimicrobial resistance monitoring system from 1999 to 2002. Journal of Antimicrobial agents and chemotherapy, 50(1): 49–54. Statistics South Africa (StatSA. (2012). Mortality and causes of death in South Africa, 2010: Findings from death notification. Statistical Release P0309.3. Available at: http://www.statssa.gov.za. (Accessed 30th September 2012). Talukder, K.A., Islam, Z., Dilip K., Dutta, M., Islam, A., Bijay, K., Khajanchi, I.J., Azmi, M. S., Iqbal, M.A., Hossain, S. G., Faruque, G., Balakrish, N. and David A. S. (2006). Antibiotic resistance and genetic diversity of Shigella sonnei isolated from patients with diarrhoea between 1999 and 2003 in Bangladesh. Journal of Medical Microbiology, 55, 1257–1263 74 Taneja, N., Nato, F., Dartevelle, S., Sire, J.M., Garin, B., Phuong, L. N., Diep, T.T., Shako, J.C., Bimet, F., Filliol, I., Muyembe, J., Ungeheuer, M.N., Ottone, C., Sansonetti, P., Germani, Y. (2011) Dipstick Test for Rapid Diagnosis of Shigella dysenteriae 1 in Bacterial Cultures and Its Potential Use on Stool Samples. PLoS ONE 6(10): e24830. doi:10.1371/journal.pone.0024830. Tao, J., Feng, L., Guo, H., Li, Y. & Wang, L. (2004). The O-antigen gene cluster of Shigella boydii O11 and functional identification of its wzy gene. Federation of European Microbiological Societies Microbiology Letter 234, 125–132. Tau, N.P., Smith, A.M., Sooka, A. and Keddy, K.H. (2012). Molecular characterization of extended-spectrum β-lactamase-producing Shigella isolates from humans in South Africa, 2003– 2009. Journal of Medical Microbiology January 61 (1):162-164 Todar K. (2010). Shigella and shigellosis. Todar’s Online Textbook of Bacteriology. Available online: http://www.textbookofbacteriology.net/Shigella.html (assessed on 16th July 2013). Tiruneh, M. (2009). Serodiversity and Antimicrobial Resistance Pattern of Shigella Isolates at Gondar University Teaching Hospital, Northwest Ethiopia. Japanese journal of infectious diseases, 62, 93-97. Toronto Public Health (TPH). (2002). Health advisory: shigellosis food poisoning investigation. Available at: http://www.city.toronto.on.ca/health/advisory_shigella.htm. (Accessed 22nd March 2014) UNAIDS. (2012). Together we will end AIDS. Available at: http://www.unaids.org/en/media/unaids/contentassets/documents/epidemiology/2012/20120718_ togetherwewillendaids_en.pdf. (Accessed 12th July 2013). 75 Ugbogu, O. C., Nwachukwu, N. C. and Ogbuagu, U. N. (2006). Isolation of Salmonella and Shigella species from house flies (Musca domestica l.) in Uturu, Nigeria African Journal of Biotechnology; 5 (11): 1090-1091, Available online at: http://www.academicjournals.org/AJB (Accessed 22nd May 2012). Vrints, M., Mairiaux, E., and Van Meervenne, E. (2009). Surveillance of Antibiotic Susceptibility Patterns among Shigella sonnei Strains Isolated in Belgium during the 18-Year Period 1990 to 2007. Journal Clinical microbiology; 47(5): 1379–1385. Warren, B.R., Parish, M.E., Schneider, K.R. (2006). Shigella as a foodborne pathogen and current methods for detection in food. Critical Reviews in Food Science and Nutrition 46(7): 551–567. Washington, E.W., Procop, G. W., Schreckenberger, P.C., Woods, G.L. (2006). Colour Atlas and Textbook of Diagnostic Microbiology, 6thTH Ed. Lippincott-Williams Publishers. Winkler, P., Ghadimi, D., Schrezenmeir, J. and Jean-Pierre, K. (2007). Molecular and Cellular Basis of Microflora-Host Interactions, Journal of Nutrition 137(8): 756S–772. World Health Organization (WHO). (2012). “Shigellosis.” (2004, 2003, 2002, 2000). http://www.who.int/csr/don/archive/disease/shigellosis/en/ (Accessed 11th July 2013) World Health Organisation, (2009). Diarrhoeal Diseases. http://www.who.int/vaccine_research/diseases/diarrhoeal/en/index6.html (Accessed 15th May 2013). World Health Organization (WHO). (2008). Guidelines for Drinking-water Quality, Incorporating 1st and 2nd Addenda, Volume 1, Recommendations. 3rd ed. WHO; Geneva, Switzerland. 76 World Health Organization. (2005). Guidelines for the control of shigellosis, including epidemics due to Shigella dysenteriae type 1. Department of Child and Adolescent Health and Development. Geneva. Available at: http://whqlibdoc.who.int/publications/2005/9241592330.pdf (Accessed 15th May 20132). Wose Kinge C, Mbewe M. (2010). Characterisation of Shigella species isolated from river catchments in the North West province of South Africa. South African Journal of Science; 106(11/12): 1-4. Yismaw, G., Negeri C and Kassu A. (2006). A five-year antimicrobial resistance pattern observed in Shigella species isolated from stool samples in Gondar University Hospital, northwest Ethiopia. Ethiopian Journal of Health Development; 20(3): 194-198. Yue-Ying, S., Hong-You, C., Xi, Z., Yuan, Z. and Min, C. (2012). The simulation study of immunomagnetic separation method for the detection of Shigella species. Laboratory Medicine; 27(3): 167-170. Zafar, A., Sabir, N. and Bhutta, Z.A. (2005) Frequency of isolation of Shigella serogroups/ scrotypes and their antimicrobial susceptibility pattern in children from slum area in Karachi. Journal of Pakistan Medical Association; 55(5): 184-8. Zaika, L.L. (2001). The effect of temperature and low pH on survival of Shigella flexneri in broth. Journal of Food Protection 64(8):1162–1165. Zaika, L.L. (2002a). The effect of NaCl on survival of Shigella flexneri in broth as affected by temperature and pH. Journal of Food Protection 65(5): 774–779. Zaika, L.L. (2002b). Effect of organic acids and temperature on survival of Shigella flexneri in broth at pH 4. Journal of Food Protection 65(9):1417–1421. Zaika, L.L. and Phillips J.G, (2005) Model for the combined effects of temperature, pH and sodium chloride concentration on survival of Shigella flexneri strain 5348 under aerobic conditions. International Journal of Food Microbiology 101(2): 179–187. 77 Zhang, H., Wang, R. and Bao, H. (2013). Phage inactivation of foodborne Shigella on ready-toeat spiced chicken. Poultry Science; 92(1): 211-7. Zhang, Y. and Lin, K. (2012). A phylogenomic analysis of Escherichia coli / Shigella group: implications of genomic features associated with pathogenicity and ecological adaptation. Bio MedCentral Evolutionary Biology, 12:174. doi:10.1186/1471-2148-12-174. 78 Appendix 79 APPENDIX I Publications 1. Zulu L. J., Nyila, M. A. and Smit J.; Laboratory Based Surveillance of Shigella, its Serotype and Resistance patterns in Johannesburg, South Africa (submitted for publication). 2. Zulu L. J. and Nyila M.A.; Stubborn Shigella infection remains a risk. (Submitted for publication). 3. Zulu L.J., Moeketsi, G.M., Thangwana, N, S. and Nyila M.A.; Carbapenem resistance trends in gram negative bacilli bacteria (to be submitted for publication). Conference Presentation 1. Zulu L. J., Nyila, M. A., and Smit J.; Laboratory Based Surveillance of Shigella, its Serotype and Resistance patterns in Johannesburg, South Africa. Abstract no. 158 was accepted (18th Biennial Conference of the South African Society of Microbiology (SASM) 24-27 November, 2013) and article was presented in part. 80 APPENDIX II Ethical approval 1. Lancet Laboratories Ethical Approval 2. University of South Africa Ethical Approval 81 82 83