Kebba Jobarteh

Absorption, Retention and
Empowerment
Addressing the Root Causes of Attrition
Through Scale-up of Community Adherence
Support Groups
Mozambique
• Population: 23.4 million (2011)
• Human Development Index
(165/169)
• Life expectancy 48.4 years
• Mean years of schooling: 1.2
- 33% adult men and 63% adult women illiterate
• Limited human resources and physical infrastructure
₋ > 830,000 births per year, ~65% in health facilities
₋ 50-60% DO NOT have access to health care
₋ Many clinics and hospitals lack continuous access to water (63%), electricity (74%)
₋ Poor roads, seasonal flooding
• >70% rural
National and USG-supported
ART coverage through 2013
400 000
360 000
320 000
280 000
240 000
200 000
160 000
120 000
80 000
40 000
0
2%
4%
0%
10%
2%
20%
8%
37%
18%
48%
27%
44%
53%
51%
45%
49%
45%
30%
32% 32%
34%
2003 2004 2005 2006 2007 2008 2009 2010 2011 2012 2013
60%
50%
40%
30%
20%
10%
0%
On Treatment
(USG - FY)
On Treatment
(National - CY)
National
Coverage (USG direct support)
National
Coverage
(MOH)
* Coverage estimates are calculated as those on ART at end of reporting period (MOH - Dec 31, USG - Sep 30), divided by midyear Spectrum estimates from 2012 Demographic Impact Report. 2012-13 USG targets are as proposed in COP12.
Absorptive Capacity
• The public health system in
Mozambique is currently straining to serve the needs of the population
– 3 physicians/100,000 inhabitants
– 21 clinical officers/100,000 inhabitants
– 40 MCH nurses/100,000 inhabitants
– 1.4 million infected
– 603,375 eligible for treatment
– 273,561 alive and on treatment
• Model of HIV care must be adapted
Traditional Retention Strategies
– Pre-ART/ART counseling
– Care package
– Peer educators
– Support groups
– Defaulter tracing
– Community health workers
– SMS messaging
A Different Approach
• Community adherence support groups
(CASG)
– Establish treatment groups with up to 6 members
– One representative from the group visits the health facility every month and does the following:
• Clinical assessment and CD4 count
• Provides feedback to the health facility about the five other members of the group
• Obtains lab results for other members
• Collects one month’s worth of ARV’s for each group member
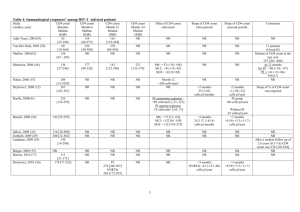
Results from MSFTête Pilot
Cohort of 1384 ART patients in 12 health facilities in Tête Province
– 291 groups formed
– 12-month retention: 97.5%
– Mortality: 0.2%
– LTFU: 2.3%
– Median follow-up time: 12.9 months
Decroo, T., Telfer, B., Biot, M., Maïkéré, J., Dezembro, S., Cumba, L. I., Dores, C. D., et al.;
Distribution of antiretroviral treatment through selfforming groups of patients in Tête province, Mozambique ; Journal of Acquired Immune Deficiency
Syndromes, February 2011
Patient Level Characteristics
• Median CD4 count at ART initiation: 176 cells/mm 3
• Median amount of time on ART prior to
CAG: 22.3 months
• Median age: 36 years
• 70% female
• Median CD4 count gain: 478.5 cells/mm 3
Before the Monthly Clinic Visit
• All members convene at a place of their choosing to do the following:
– Discuss their health and any other issues that may arise
– Pill counts
– Basic negative screening tool
After the Monthly Clinic Visit
• All members of the group reconvene at a place of their choosing to do the following:
– Report lab results
– Distribute medications
– Convey any health messages received during the clinic visit
Impact at Health Facility
• Reduce number of stable ART patients accessing the health facilities
• Increase capacity of a health facility to enroll new patients
• Increase amount of time staff can dedicate to sick or complex patients
• Decrease congestion at the pharmacy
• Decrease acuity of consultations and admissions due to earlier access to health services
• Improved reporting on patient outcomes
Impact on patient
• Decreased number of health facility visits
• Improved self-monitoring of clinical conditions
• Improved psycho-social support
• Stigma reduction
• Early warning system for illness
• Improved monitoring and resources to address adherence problems
• Social safety net
• Income generation
• Family testing
• Community education
Scale-Up
• Government of Mozambique piloting the model in all 11 Provinces
– 3-6 health facilities per Province
– 3 tiers
• >1000 patients
• 500-10000 patients
• <500 patients
• 12-month pilot with national scale-up pending the results of retrospective evaluation
6 Months of Progress
PROVINCE
Cabo Delgado
Gaza
Inhambane
Manica
Maputo Cidade
Maputo
Provincia
Nampula
Niassa
Sofala
Zambezia
Grand Total
NUMBER OF
GROUPS
51
121
159
94
87
123
84
41
132
189
1081
NUMBER OF
PATIENTS
229
552
727
318
152
561
310
150
492
813
4304
Who is currently eligible
• Non-pregnant
• Stable
• Adult (or at least adult doses of ARVs)
Who could be eligible?
• Pre-ART populations
• Pregnant HIV-infected women
• Children
• Defaulters
• TB infected patients
• HIV/TB co-infected patients
Challenges
• Allowing for a flexible dynamic
• Phased implementation
• Perception of strategy as a panacea
• Staff ownership
• CD4 count monitoring
• Demand creation
• Urban settings
• Links with other adherence and retention strategies
• Patients with the most need may not have access
“The most important aspect of self-management is the realization that people with a chronic condition are those that have the most comprehensive expertise in dealing with that condition.”
-Katarina Kober & Wim Van Damme
Obrigado!
Acknowledgements
HIV-infected and affected Mozambicans
Aleny Couto (MISAU)
Vania Macome (MISAU)
Armando Bucuane (MISAU)
Joe Lara (MISAU)
Tom Decroo (MSF-B)
Sergio Dizembro (MSF-B)
Inacio Malimane (CDC)
Paula Samo Gudo (CDC)
Lisa Nelson (CDC)