Masterclass 8
advertisement

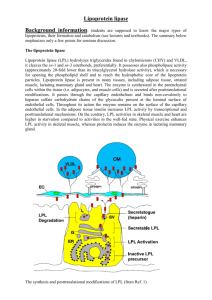
Massive Hypertriglyceridaemia: A complete white-out, INTESTINE Chylomicrons B -48 B LIVER E LPL CII CII LCAT AI CE FC CE Other tissues F C AII LCAT B LDL-R E B CETP HDL LDL FC Macrophage FC ABCA1 LPL E LRP SRCE+FC B1 AI E AII VLDL CIII R AI B -100 SR-A CD-36 Lox-1 SR-PSOX IDL CIII HL . O B OxLDL DAVIGNON 2006 Metabolic Relationships Among Lipoproteins 1. VLDL LDL 3. HDL TG 2. TRIGLYCERIDES Lipoprotein Lipase` HDL SMALL DENSE LDL Chylomicrons and their remnants may be less likely to cause atherosclerosis (smaller numbers and larger size) Fatty Acid and Triglyceride Flux FATTY ACIDS (ALBUMIN) TG (VLDL) LIPOPROTEIN LIPASE TG (CHYLO-MICRONS) Pancreatic Lipase Movement Most pancreatic lipase is secreted into the pancreatic duct, but some moves back into capillaries. Chylomicron Role in Pancreatitis Pancreatic lipase acts on chylomicrons adherent to capillary endothelium, producing fatty acid anions, or soaps. By detergent action, cell membranes are disrupted, releasing more lipase, and additional fatty acid anions are produced in a vicious cycle. Dietary management of lipoprotein lipase deficiency: Avoid dietary fat, except MCT’s and marine oil n-3 fatty acids Other treatment options in lipoprotein lipase deficiency • Fibrates and marine oil n-3 fatty acids: limitation of gene response • Avoid insulin deficiency: Cofactor for lipoprotein lipase • Temporary effect of plasmapheresis • Temporary effect of plasma transfusion in apo C2 (cofactor) deficiency • ? Xenical • Future: DGAT1 inhibitors • ?Gene therapy Algorithm for Diagnosis of Apo B Dyslipoproteinemias HyperApo B > 1.2 g/L NormoApo B < 1.2 g/L NormoTG < 1.5 mmol/L HyperTG > 1.5 mmol/L TG:Apo B > 0.12 NomoTG > 1.5 mmol/L Hyper TG > 1.5 mmol/L LDL VLDL + LDL TG:Apo B < 0.12 Apo B > 0.75 g/L Apo B < 0.75 g/L TC:Apo B > 6.2 TC:Apo B < 6.2 Chylo + VLDL Chylo Chylo + VLDL Remnants VLDL ■ Complete (FHC) or partial LPL deficiency associated with a secondary factor ■ Complete LPL deficiency (FHC) ■ Primary apoCII deficiency ■ Familial dysbetalipoproteinemia (type III) ■ Hepatic lipase deficiency ■ (Primary cause associated with a secondary factor) Lipoproteins Normal Primary Causes ■ Normal ■ Hypoalphalipoproteinemia ■ Familial hyperTG ■ Partial LPL deficiency ■ FH ■ Polygenic ■ FDB ■ PCSK9 deficiency ■ ARH deficiency ■ CYP7A1 deficiency ■ Hypoalphalipoproteinemia ■ FCH ■ βSitosterolemia Abbreviations: apo, apolipoprotein; ARH, autosomal recessive hypercholesterolemia; CAPD, continuous ambulatory peritoneal dialysis; Chylo, chylomicrons; CP7A1, cytochrome P450 7A1; DM2, diabetes mellitus type 2; dysbeta; dysbetalipoproteinemia; FCH, familial combined hyperlipidemia; FDB, familial defective apoB; FH, familial hypercholesterolemia; FHC, familial hyperchylomicronemia; HAART, highly active antiretroviral therapy; LPL, lipoprotein lipase; PCOS, polycystic ovary syndrome; SLE, systemic lupus erythematosus; TC, total cholesterol; TG, triglyceride. de Graaf J et al. Nat Clin Pract Endocrinol Metab 2008;4:608- Relationship of Non-Fasting Triglycerides and Cardiovascular Risk Copenhagen City Heart Study(7587 women and 6394 men) Nordestgaard BG, et al. JAMA. 2007;298(3):299-308 Relationship of Non-Fasting Triglycerides and Cardiovascular Risk Womens Health Study (n= 26,509) Bansal S, et al. JAMA. 2007;298(3):309-316 Relationship of Non-Fasting Triglycerides and Cardiovascular Risk Copenhagen City Heart Study(7587 women and 6394 men) Nordestgaard BG, et al. JAMA. 2007;298(3):299-308 Rx and response Fibrates and marine oil n-3 fatty acids: greater prospect of gene upregulation Niacin: greater prospect of gene upregulation Avoid insulin deficiency: Cofactor for lipoprotein lipase Temporary effect of plasmapheresis ? Xenical Future: DGAT1 inhibitors Essential Fatty Acid Families ω-3 family ω-6 family H3C C18:2 ω-6 COOH Linoleic H3C C18:3 ω-3 • Corn Oil • Safflower Oil • Sunflower Oil H3C H3C COOH C20:4 ω-6 Arachidonic COOH -Linolenic • Flaxseed Oil • Canola Oil • Soybean Oil COOH C20:5 ω-3 Eicosapentaenoic (EPA) H3C COOH C22:6 ω-3 Docosahexaenoic (DHA) More thrombotic and inflammatory metabolites Less thrombotic • Oily Fish and inflammatory • Fish Oil Capsules metabolites What happens in the food chain?: Starting materials Modification by herbivores Accumulation by carnivores Essential Fatty Acid Contrasts: Position of 1st double bond • N-6 : • Greater availability in diet • Greater availability in membranes. • Main substrate for PG & LT • Typical inflammatory response • N-3: • Lower availability, so lesser substrate for PG & LT • Highest potential number of double bonds. • Less inflammatory response Essential Fatty Acid Contrasts: Chain length • N-3 < 20C (Plant): • N-3 > C20 (Marine) • Too short for membrane Phosphlipid • Suitable for membrane Phospholipid • Full effect as antiarrhythmic • Strongly anti- arrhythmic • No effect on TG • No effect on platelet adhesion • Effective precursor • Reduce TG synthesis and decrease TG by about 50% • Reduce platelet adhesion. Postprandial Lipoproteins affect FMD after Oral Fat Load 7 6 Triglycerides mmol/L 5 4 3 2 0h 2h 4h 6h 8h TG & RLP-C increased significantly and continuously up to 4 & 6 hours respectively 1.0 0.9 Remnant-C FMD revealed decreased vasodilation at 4-6 hours mmol/L 0.8 0.7 0.6 0.5 0.4 0h 2h 4h 6h 8h 2h 4h 6h 8h % Dilation 18 16 14 12 Results vary, but postprandial events, including secretion of chylomicrons, exert strong effects on vascular function FMD 10 0h Franco M et al. J Clin Endo & Metab 2004;89:2946-2950 Summary and link to cases Mrs N.S. • This 36 year old woman has not been able to conceive. She gained a large amount of weight (BMI 38) when she stopped smoking in her mid 20’s. Unfortunately she resumed smoking in her early 30’s without any change in weight. Alcohol intake is less that 30 gms / week. Two years ago she became diabetic and now requires insulin to maintain HB A1C < 7.5%. Even then, associated lipid levels include triglyceride of 38 mmol/l, but she has not suffered pancreatitis. Questions concerning Mrs N.S. • What priority do you place on cessation of smoking in this case? High / Low • Your preferred strategy to achieve weight loss involves the use of A) Xenical B) Meal replacement C) gastric bypass D) Metformin • If symptoms suggested the onset of an attack of pancreatitis, appropriate immediate intervention would include: A) Nil by mouth B) Consideration of plasmapheresis, C) Commencement of statin therapy D) Reduction in Insulin dose E) All of the above This 36 year old woman has not been able to conceive. She gained a large amount of weight (BMI 38) when she stopped smoking in her mid 20’s. Unfortunately she resumed smoking in her early 30’s without any change in weight. Alcohol intake is less that 30 gms / week. Two years ago she became diabetic and now requires insulin to maintain HB A1C < 7.5%. Even then, associated lipid levels include triglyceride of 38 mmol/l, but she has not suffered pancreatitis. • What priority do you place on cessation of smoking in this case? High / Low • Your preferred strategy to achieve weight loss involves the use of A) Xenical B) Meal replacement C) gastric bypass D) Metformin • If symptoms suggested the onset of an attack of pancreatitis, appropriate immediate intervention would include: A) Nil by mouth B) Consideration of plasmapheresis, C) Commencement of statin therapy D) Reduction in Insulin dose E) All of the above What priority do you place on cessation of smoking in this case? • High • Low What priority do you place on cessation of smoking in this case? A vexed problem. Theoretical reasons for “high” Your preferred strategy to achieve weight loss involves the use of ... • A) Xenical • B) Meal replacement • C) gastric bypass • D) Metformin Your preferred strategy to achieve weight loss involves the use of ... Pro’s and con’s of each If symptoms suggested the onset of an attack of pancreatitis, appropriate immediate intervention would include • A) Nil by mouth • B) Consideration of plasmapheresis, • C) Commencement of statin therapy • D) Reduction in Insulin dose • E) All of the above If symptoms suggested the onset of an attack of pancreatitis, appropriate immediate intervention would include... Pattern of the problem (a case for “A”) Mrs N.S. • Although advice about diet and smoking fails to alter weight or glycaemic control, your introduction of fenofibrate and fish oil reduces TG to 17 mmol/l. Mrs N.S. desperate to start a family and is actively pursuing IVF. • Is the decline in TG to 17 mmol/l sufficient to eliminate the risk of acute pancreatitis? Yes / No • Do reproductive hormones like oestrogen and progesterone, IVF therapies or pregnancy itself affect triglyceride levels or risk of pancreatitis? Yes / No • Would you continue fenofibrate? Yes / No • Your estimate on Mrs N.S’s risk of a cardiovascular event is: A) Low now and in the future B) Low now, but high in the future C) High, even now. Is the decline in TG to 17 mmol/l sufficient to eliminate the risk of acute pancreatitis? • Yes • No Is the decline in TG to 17 mmol/l sufficient to eliminate the risk of acute pancreatitis? The case for “no” TG in mg% For mmol/l Divide by 90 Do reproductive hormones like oestrogen and progesterone, IVF therapies or pregnancy itself affect triglyceride levels or the risk of pancreatitis? • Yes • No Do reproductive hormones like oestrogen and progesterone, IVF therapies or pregnancy itself affect triglyceride levels? The case for “yes” Obstet Gynecol. 1993 May;81(5 ( Pt 2)):890-2. Recurrent pancreatitis associated with in vitro fertilization. Steinmetz OK, Hashim E, Falcone T, Hemmings R, Bourque J. BACKGROUND: We report the possible association between in vitro fertilization (IVF) and recurrent acute pancreatitis. CASE: A patient developed acute pancreatitis during each of two cycles of IVF. On a spontaneous cycle, serum triglycerides were as follows: early follicular phase 2.34 mmol/L, mid-follicular phase 4.17 mmol/L, and late follicular phase 6.6 mmol/L. During an episode of acute pancreatitis, the serum triglyceride level was 38.45 mmol/L. CONCLUSION: Acute pancreatitis may occur in patients with a family or personal history of hypertriglyceridemia who are candidates for IVF. Would you continue fenofibrate? • Yes • No Would you continue fenofibrate? Uncertain teratogenicity versus manifest risk. Pregnancy: Teratogenic Effects, Pregnancy Category C Safety in pregant women has not been established. Fenofibrate has been shown to be embryocidal and teratogenic in rats when given in doses 7 to 10 times the maximum recommended human dose (MRHD) and embryocidal in rabbits when given at 9 times the MRHD (on the basis of mg/meter2 surface area). There are no adequate and well-controlled studies in pregnant women. Fenofibrate should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus Your estimate on Mrs N.S’s risk of a cardiovascular event is: A) Low now and in the future B) Low now, but high in the future C) High, even now. Your estimate on Mrs N.S’s risk of a cardiovascular event is: The tentative case for “C” Mr G.T. • Mr G.T. is 32 years old. He is Chinese and he consumes an Asian diet. He is not overweight, but his business and social obligations involve occasional Asian banquets. He rarely drinks more than 20 gms alcohol per week. He suffered occasional episodes of abdominal pain in adolescence and early adulthood, and recently he was admitted to an intensive care unit with his first episode of acute pancreatitis. Fasting plasma lipids included plasma triglyceride level of 56 mmol/l but plasma glucose is within normal limits. Questions concerning Mr G.T. • What physical findings might accompany an episode of this severity? (More than 1 possible) A) Tendon Xanthomas B) Lipaemia Retinalis C) Tuberous Xanthomas D) Eruptive Xanthomas E) Corneal Arcus • How would you investigate the possibility of lipoprotein lipase (LPL) deficiency? A) Plasma LPL mass B) Plasma LPL activity C) Plasma LPL activity after a heparin bolus D) Protein iso-electric focussing for Apo C3 E) Genetic testing • What diet advice would you give on discharge? A) Low fat diet < 10% energy B) Medium chain triglycerides to minimumize carbohydrate C) Extra fish oil (>15 gms) D) All of the above E) Low fat diet < 25% energy • Mr G.T. is 32 years old. He is Chinese and he consumes an Asian diet. He is not overweight, but his business and social obligations involve occasional Asian banquets. He rarely drinks more than 20 gms alcohol per week. He suffered occasional episodes of abdominal pain in adolescence and early adulthood, and recently he was admitted to an intensive care unit with his first episode of acute pancreatitis. Fasting plasma lipids included plasma triglyceride level of 56 mmol/l but plasma glucose is within normal limits. • What physical findings might accompany an episode of this severity? (More than 1 possible) A) Tendon Xanthomas B) Lipaemia Retinalis C) Tuberous Xanthomas D) Eruptive Xanthomas E) Corneal Arcus • How would you investigate the possibility of lipoprotein lipase (LPL) deficiency? A) Plasma LPL mass B) Plasma LPL activity C) Plasma LPL activity after a heparin bolus D) Protein iso-electric focussing for Apo C3 E) Genetic testing • What diet advice would you give on discharge? A) Low fat diet < 10% energy B) Medium chain triglycerides to minimumize carbohydrate C) Extra fish oil (>15 gms) D) All of the above E) Low fat diet < 25% energy What physical findings might accompany an episode of this severity? (More than 1 possible) • A) Tendon Xanthomas • B) Lipaemia Retinalis • C) Tuberous Xanthomas • D) Eruptive Xanthomas • E) Corneal Arcus What physical findings might accompany an episode of this severity? (More than 1 possible) The case for “B” and “D” How would you investigate the possibility of lipoprotein lipase (LPL) deficiency? • A) Plasma LPL mass • B) Plasma LPL activity • C) Plasma LPL activity after a heparin bolus • D) Protein iso-electric focussing for Apo C3 • E) Genetic testing How would you investigate the possibility of lipoprotein lipase (LPL) deficiency? The case for “C”, but “E” is becoming possible What diet advice would you give Mr G.T. on discharge? • A) Low fat diet < 10% energy • B) Medium chain triglycerides to minimize carbohydrate • C) Extra fish oil (>10 gms/day) • D) All of the above • E) Low fat diet < 25% energy What diet advice would you give Mr G.T. on discharge? The case for “D”, but the dilemma re CHO More questions about Mr G.T. • Despite your dietary advice, Mr G.T. suffers a recurrence of pancreatitis 5 months later. • When massive hypertriglyceridaemia is present, which of the following symptoms may occur? A) Risk of pancreatitis, Abdominal pain, hepatosplenomegaly B) Confusion C) Peripheral paresthesias D) Dyspnea E) All of the above • If lipoprotein lipase deficiency is confirmed, what treatment options would you suggest? A) Continuation of current diet B) Gene therapy C) Total pancreatectomy plus pancreatic transplant D) Biliary diversion E) Plasmapheresis When massive hypertriglyceridaemia is present, which of the following symptoms may occur? A) Risk of pancreatitis, Abdominal pain, hepatosplenomegaly B) Confusion C) Peripheral paresthesias D) Dyspnea E) All of the above When massive hypertriglyceridaemia is present, which of the following symptoms may occur? The case for “E”. Accumulated case reports, eg “He reported recurrent headaches and dizziness with lightheaddedness and vertigo independently of alcohol consumption. These symptoms were accompanied by mood disturbances including dysphoria and depression. Neurologic examination was normal. If lipoprotein lipase deficiency is confirmed, what treatment options would you suggest? • A) Continuation of current diet • B) Gene therapy • C) Total pancreatectomy plus pancreatic transplant • D) Biliary diversion • E) Plasmapheresis If lipoprotein lipase deficiency is confirmed, what treatment options would you suggest? The case for “A”