is/are from dog(s) with acute pancreatitis?
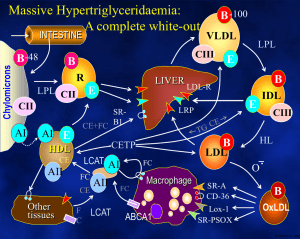
advertisement

History • Signalment • Diet • Vomiting • Prior episodes • Diarrhea History • Signalment • Diet • Vomiting • Prior episodes • Diarrhea Physical Examination • Anterior abdominal pain • Icterus • Profuse ascites • Fever • SQ abscesses Physical Examination • Anterior abdominal pain • Icterus • Profuse ascites • Fever • SQ abscesses WHICH CBC(S) IS/ARE FROM DOG(S) WITH ACUTE PANCREATITIS? 147033 147198 90524 PCV 28.5 28.8 30 40 WBC 30,000 45,500 9,800 11,500 Segs 26,100 33,670 4,606 9,890 Bands 900 2,730 2,450 0 Plat 87,000 407,000 679,000 470,000 Toxic mod mod none 159796 none Clinical Pathology • An anorexic, vomiting dog with fasting hyperlipidemia probably has acute pancreatitis Clinical Pathology • An anorexic, vomiting dog with fasting hyperlipidemia probably has acute pancreatitis • Most dogs with pancreatitis DO NOT have fasting hyperlipidemia Clinical Pathology • Amylase/Lipase – Sensitivity ~ 50% – Specificity ~ 50% • TLI – Sensitivity ~ 35% Clinical Pathology • cPLI – Sensitivity ~ 80-85% Sig: 7 yr M Boxer X CC: Anorexia/Vomiting HPI: Started 1 week ago snap PLI = pancreatitis Dog died despite therapy: Everything normal on gross necropsy PANCREATITIS versus CLINICALLY IMPORTANT PANCREATITIS Diagnostics • cPLI – Sensitivity ~ 80% • Abdominal ultrasound – Sensitivity probably ranges from 40% to about 65% Diagnostics • cPLI – Sensitivity ~ 80% • Abdominal ultrasound – Sensitivity probably ranges from 40% to about 65% because clinicians rarely repeat the ultrasound Diagnostics • cPLI – Sensitivity ~ 80% • Abdominal ultrasound – Sensitivity probably ranges from 40% to about 65% – Findings can change within hours ... WHAT IS THE BEST WAY TO DIAGNOSE CANINE ACUTE PANCREATITIS? Patient with possible acute pancreatitis Find evidence suggestive of pancreatitis Eliminate diseases mimicking pancreatitis Imaging (ultrasound) Chemistry panel Abdominal imaging cPLI Patient with possible acute pancreatitis Find evidence suggestive of pancreatitis Eliminate diseases mimicking pancreatitis Imaging (ultrasound) Chemistry panel Abdominal imaging cPLI All things being equal, try to avoid surgery THE REAL PROBLEM IS THAT ACUTE PANCREATITIS CAN PRESENT IN SO MANY DIFFERENT WAYS THAT YOU DON’T EVEN SUSPECT IT INITIALLY TAMU #88267 Sig: 7 yr M Sheltie CC: Vomiting HPI: Began 5 weeks ago Partial anorexia, vomits phlegm or bile once daily Dog otherwise pretty healthy PE: No significant abnormalities TAMU #88267 PCV = 37% (35-55) WBC = 21,800/ul (6,-16,000) Segs = 20,274/ul (4,-14,000) Lymphs = 840/ul (1,000 - 4,000) Platelets = 255,000/ul (200, - 500,000) TAMU #88267 Creatinine = BUN = Total protein = Albumin = ALT = SAP = Bilirubin = Urine: 2.0 mg/dl (< 2.0) 36 mg/dl (8-29) 4.7 gm/dl (5.5-7.5) 1.7 gm/dl (2.5-4.4) 10 U/L (< 130) 31 U/L (< 147) 0.4 mg/dl (< 1.0) 1.015 with 4+ protein TAMU #159796 Sig: 9 yr M(c) Pug CC: Vomiting, yellow scleras HPI: Feeling bad 12 days ago Started vomiting, responded to fluid therapy, but became ill again when started feeding it Dog’s eyes turned yellow PE: Scleras yellow TAMU #159796 PCV = 40% (35-55) WBC = 11,500/ul (6,-14,000) Segs = 9,890/ul (4,-12,000) Lymphs = 460/ul (1,-4,000) Eos = 230/ul (100-1,250) Platelets = 470,000/ul (200,-500,000) TAMU #159796 BUN = Creatinine = Glucose = Potassium = Cholesterol = Albumin = ALT = SAP = Bilirubin = 4 mg/dl (8-29) 0.7 mg/dl (< 2.0) 95 mg/dl (75-133) 3.6 mEq/L (3.8-5.1) 597 mg/dl (120-247) 2.9 gm/dl (2.5-4.4) 1,691 IU/L (< 130) 3,134 IU/L (< 147) 4.5 mg/dl (0-0.8) TAMU #159796 4/9 4/11 4/13 4/15 ALT 1,691 2,108 1,275 SAP 3,134 3,753 3,633 Bili 4.5 4.5 4.8 2.6 4/16 1.2 TAMU #152494 Sig: 9 yr F(s) Dalmation CC: Vomiting/diarrhea HPI: Vomiting food/bile 6-8X in 2 weeks Diarrhea constantly for 2 weeks Decreased appetite for 10 days, anorexia for 5 days PE: T = 102.5 F, HR = 102/min TAMU #152494 PCV = 35.5% (35-55) WBC = 21,700/ul (6,-14,000) Segs = 15,200/ul (4,-12,000) Bands = 630/ul (< 500) Lymphs = 1,400/ul (1,-4,000) Platelets = 568,000/ul (200,-500,000) TAMU #152494 Sodium = 152 mEq/L (138-148) Potassium = 4.1 mEq/L (3.5-5.0) Glucose = 107 mg/dl (60-120) Albumin = 2.7 gm/dl (2.5-4.4) ALT = 123 IU/L (< 110) SAP = 2,174 IU/L (< 130) Creatinine = 1.3 mg/dl (< 2.0) TAMU #152494 Abdominal ultrasound: “… Small amount of anechoic effusion between liver lobes and around urinary bladder. Fine Needle Aspirate reveals turbid yellow tan fluid.” TAMU #152494 Abdominal fluid: WBC = 153,000/ul RBC = 0/ul Total protein = 4.6 gm/dl 90% nondegenerate neutrophils 8% macrophages, vaculated “Suppurative exudate” TAMU #152494 “Chronic necrotizing and fibrosing interstitial pancreatitis with multifocal ... suppuration and hemorrhage and peritonitis ...” Sterile pancreatitis versus Septic peritonitis Abdominal fluid 147260 152494 TP gm/dl 5.1 4.6 152485 109612 1.3 3.6 WBC/ul 15,059 153,000 700 18,200 RBC/ul 91,112 0 83,700 30,000 PANCREATITIS CAN: a) make no abdominal effusion b) make a little abdominal effusion c) make a massive abdominal effusion Pancreatitis can present as: • acute vomiting with abdominal pain • chronic, low grade vomiting/anorexia (abscess) • icterus (biliary tract obstruction) • ascites (minimal, little or lots) • acute abdomen (looks just like septic peritonitis) • SIRS (looks like septic shock) • any really sick animal SYSTEMIC INFLAMMATORY RESPONSE SYNDROME – used to be called “Septic shock” SYSTEMIC INFLAMMATORY RESPONSE SYNDROME – inadequate perfusion of the body tissues because of an exaggerated inflammatory response WHAT IS SUPPOSED TO HAPPEN Bacterial toxin, inflammatory cytokines Lymph nodes, hepatic macrophages Systemic circulation Courtesy of Dr. Katrina Mealey WHAT IS SUPPOSED TO HAPPEN Bacterial toxin, inflammatory cytokines Lymph nodes, hepatic macrophages Systemic circulation WHAT CAN HAPPEN Inflammatory cytokines Lymph nodes Systemic circulation EARLY -- SIRS Mild uneven vasodilatation “High output” shock Bright red mucus membranes Fast capillary refill time Bounding pulses Tachycardia LATE -- SIRS Severe peripheral vasodilatation + poor cardiac contractility “Low output” shock Pale mucus membranes Weak pulses Slow refill time THERAPY FOR PANCREATITIS Only supportive and symptomatic • NPO versus early feeding THERAPY FOR PANCREATITIS Only supportive and symptomatic • NPO versus early feeding • Fluid therapy Crystalloids Plasma Colloids Total/partial parenteral nutrition THERAPY FOR PANCREATITIS Only supportive and symptomatic • NPO versus early feeding • Fluid therapy Crystalloids Plasma Colloids Jejunostomy feeding (PEG-J, Nasal J, regular J) THERAPY FOR PANCREATITIS Only supportive and symptomatic • NPO versus early feeding • Fluid therapy Crystalloids Plasma Colloids Nutrition • Analgesics THERAPY FOR PANCREATITIS Only supportive and symptomatic • NPO versus early feeding • Fluid therapy • Analgesics • Anti-emetics: if vomiting makes it hard to maintain hydration or patient is really miserable • Proton-pump inhibitors: the same OTHER POSSIBILITIES • Antibiotics – “Regular” pancreatitis – SIRS OTHER POSSIBILITIES • Antibiotics • Heparin OTHER POSSIBILITIES • Antibiotics • Heparin • Steroids – Critical Care Medicine 36: 296-327, 2008