Rashes in Pregnancy - Kate Hooks
advertisement

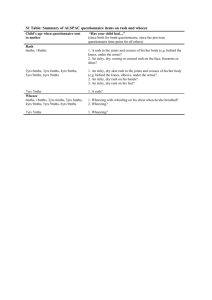
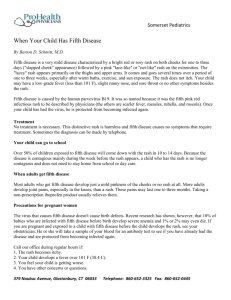
Kate Hooks A Common Consultation AIMS: To distinguish rashes which may have complications from those which do not. To develop a management strategy Some understanding of other skin rashes in pregnancy. Detailed hx/bloods at booking All women advised to contact GP or Midwife urgently if they are in contact with or develop a rash. Common illness Highly contagious- 90% of adults are immune Complicates 3/1000 pregnancies Incubation- 14-21 days- infectious from 2 days before the rash until crusting Features- Fever, Rashpapules/vesicles/centripetal/itchy/mucus membranes Risk to Mother 10% risk of pneumonia- inc with gestation Mortality 1/1000 infections Refer if rash worsening for >6 days Admit: Chest symptoms Neurological symptoms Haemorrhagic rash Immunosuppressed Risk- term, smoker, poor social circumstances Risk to Foetus/Newborn Gestation- <28wks 5-10% >30wks 50% Presentation <20wks- ^Miscarriage 1-2% FVS 20-37wks – risk of FVS rare Baby especially vulnerable 4 days before to 2 days after delivery- 20% risk of overwhelming neonatal infection- SPECIALIST ADVICE Management Mother clear hx of chickenpox- reassure Not- Send Serum Specific IgG- positive – reassure Negative- VZ-IgG- if less than 10 days from exposure- and close monitoring. Vaccination- rare 1-2% adult women are susceptible Reinfection can occur in those vaccinated Incubation- 14-21 Infectious- 7 days before-10 days after rash. Fever, lymphadenopathy and pink maculopapular rash Risk to Foetus <11wks- 90% risk transmission- 90% adverse outcome risk 11-16wks- 55% risk transmission- 20% adverse outcome risk >16wks- 45% risk transmission- risk deafness only >20wks- foetal development not affected Management Non vesicular rash- check for rubella antibodies or reassure only if immunisation x2. Also check Parvovirus B19. IgG- reassure No antibodies- send another sample 1 month after contact IgM- Confirm- inform mother result and implications Risk infection in pregnancy 1/400 50% young women not immune 50% risk of child fifths disease- non immune mother. Inc- 13-18 days- infectious from 10 days before the rash appears to the onset. Fever, arthritis, lace like rash trunk and extremities, ‘slapped cheeks’. Risk to Foetus Risk of transmission increases significantly with increased gestation. <20 weeks- 9% increase risk of miscarriage 3% affected foetuses- Hydrops- 50% will die Management Check for antibodies B19 IgG- reassure None- send further sample in 1 month or if rash develops IgM- confirm- Refer for specialist care No known Rx to prevent transmission 2 Weekly USS for hydrops Rare- MMR Coryzal, lymphadenopathy, conjunctivitis, maculopapular rash, Koplick spots No evidence to support an association between measles in pregnancy and congenital defects. But- Inc- maternal mortality, foetal loss and prematurity. Management- identify susceptible exposed womenspecialist care- human normal immunoglobulin Enterovirus Febrile illness o young children If contracted if 1st trimester- intrauterine growth retardation and spontaneous abortion Refer for specialist care Others- EBV, CMV Itchy In stretch marks in later stages Allergic response Rx- emollients and topical steroids Rare Autoimmune Second and third trimester Itchy, blistering, initially around the umbilicus and then the rest of the body Specialist advice- skin biopsy Rx- topical or oral steroids Common consultation If infectious exposure always check antibodies and seek specialist advice if no clear history.