INTRAOCULAR PRESSURE
LECTURE
S.C.C.O.
4/13/2015
1
I. DEFINITION
A. the tissue pressure of the ocular
contents
B. about 15 mm Hg but does fluctuate
(15.5 +/- 2.57)
C. normal range of pressures: 10.5 20.5
S.C.C.O.
4/13/2015
2
II. HOW IS IOP PRODUCED
S.C.C.O.
A. Aqueous produced by the ciliary
processes into the posterior chamber --> flows to anterior chamber and vitreole
chamber ---> bulk of fluid flows out the
angle (trabecular outflow) of the anterior
chamber (flow rate = 2.5
microliters/min)
4/13/2015
3
S.C.C.O.
4/13/2015
4
S.C.C.O.
4/13/2015
5
II. HOW IS IOP PRODUCED
– 1. resistance to flow at the lens-iris
interface
– 2. resistance to flow at the angle of the
anterior chamber
a.
pressure in the eye increases until the force
pushing fluid out of the eye (i.e., the eye
pressure) results in the same amount of fluid
leaving the eye as is produced and enters the
eye
S.C.C.O.
B. Aqueous exchanged with the retina,
lens, ciliary body,4/13/2015
iris and cornea
6
S.C.C.O.
4/13/2015
7
S.C.C.O.
4/13/2015
8
S.C.C.O.
4/13/2015
9
S.C.C.O.
4/13/2015
10
III.
FACTORS
INFLUENCE IOP
THAT
A. Long Term
– 1. Genetics - relatives of individuals with
open-angle glaucoma are more likely to
have high IOP
– 2. Age - IOP increases with increasing age
S.C.C.O.
4/13/2015
11
III. FACTORS THAT
INFLUENCE IOP
– 3. Sex - IOP's equal
in the age range 20
to 40, after
menopause women
have higher IOP's
S.C.C.O.
4/13/2015
12
III. FACTORS THAT
INFLUENCE IOP
– 4. Race - African-Americans have a higher
incidence of glaucoma than whites
S.C.C.O.
4/13/2015
13
III.
FACTORS
INFLUENCE IOP
THAT
B. Short Term
– 1. Diurnal variation - 3 to 6 mm Hg change
in 24 hr period; > 10 mm Hg change is
pathogenic
a.
Change probably related to aqueous
production and not drainage
S.C.C.O.
4/13/2015
14
S.C.C.O.
4/13/2015
15
S.C.C.O.
4/13/2015
16
III. FACTORS THAT
INFLUENCE IOP
– 2. Sitting - going
from a sitting to a
lying position results
in an increase in IOP
which is even greater
in glaucoma patients
– 3. Total Body
Inversion - causes
an increase in IOP
by as much as 15
mm Hg
S.C.C.O.
4/13/2015
17
III.
FACTORS
INFLUENCE IOP
THAT
– 4. Blinking - raises IOP briefly
– 5. Exercise - decreases IOP
– 6. Blepharospasm - increases IOP
– 7. Coughing - increases IOP
– 8. Blood pressure - some people believe
there is a link between blood pressure and
IOP but no clear evidence
– 9. General anesthesia - decrease IOP
– 10. Alcohol - decreases IOP
S.C.C.O.
4/13/2015
18
III.
FACTORS
INFLUENCE IOP
THAT
– 11. Cannabis - decreases IOP
– 12. Tobacco - increases IOP
– 13. Cholinergic Stimulating Agents (i.e.,
pilocarpine and echothiophate) - decrease
IOP by increasing the aqueous outflow
– 14. Adrenergic Stimulating Agents (i.e.,
epinephrine, propine, iopidine, alphagan) lower IOP by enhancing aqueous outflow
S.C.C.O.
4/13/2015
19
III.
FACTORS
INFLUENCE IOP
THAT
– 15. Adrenergic Blocking Agents (i.e.,
timolol and betaxolol) - decrease IOP by
decreasing aqueous production
– 16. Carbonic anhydrase inhibitors (i.e.,
diamox, trusopt, azopt) - decrease
aqueous production
– 17. Prostaglandins (i.e., xalatan, rescula,
travatan, lumigan) - increase uveoscleral
outflow
S.C.C.O.
4/13/2015
20
IV. MEASUREMENT OF IOP
A. Manometry
– 1. Cannulate the anterior chamber and
directly measure the pressure
– 2. Can not be done on humans
– 3. The original method used to measure
IOP
S.C.C.O.
4/13/2015
21
IV. MEASUREMENT OF IOP
B. Tonometry
– 1. Indentation
a.
the older of the 2 methods to measure IOP in
humans
b. involves measuring the indentation of the
cornea resulting from a given weight
c. the Schiotz tonometer is an indentation
tonometer
d. the weight of the tonometer displaces fluid in
the eye and thus affects the IOP measurement
S.C.C.O.
4/13/2015
22
IV. MEASUREMENT OF IOP
– 2. Applanation
a.
only flattens a small portion of the cornea so
does not displace a large amount of aqueous.
b. better accuracy than indentation
c. the NCT and the Goldmann tonometers are
examples
S.C.C.O.
4/13/2015
23
IV. MEASUREMENT OF IOP
C. Schiotz
Tonometer
– 1. a plunger of a
known weight
pushes on the
cornea - thus result
depends on ocular
rigidity
S.C.C.O.
a. concept of ocular
rigidity developed by
Friedenwald
4/13/2015
24
S.C.C.O.
4/13/2015
25
IV. MEASUREMENT OF IOP
b.
log Pt - log Po = EVc
– log Pt1 - log Pt2 = E(Vc2 - Vc1)
– Pt = tonometric pressure
– Pt1, Pt2 = tonometric pressures with
different
plunger loads
– Po = IOP before tonometry
– E = coefficient of ocular rigidity
– Vc1, Vc2 = volume of corneal indentation
corresponding to Pt1 and Pt2
c.
average value of ocular rigidity is 0.0215, the
slope of the line joining the plots of 2
nomogram readings
S.C.C.O.
4/13/2015
26
S.C.C.O.
4/13/2015
27
IV. MEASUREMENT OF IOP
– 2. Advantages of Schiotz tonometry
a.
small and easily transported
b. inexpensive (about $100)
c. does not require electricity
S.C.C.O.
4/13/2015
28
IV. MEASUREMENT OF IOP
– 3. Disadvantages of Schiotz tonometry
a.
not extremely accurate - ocular rigidity
dependent and instrument scale markings are
not detailed
b. requires anesthetic for most patients
c. assumes everyones epithelium is 0.05 mm
thick
d. technique can produce abrasions
e. best if patient in a reclining position
f. placing the tonometer on the eye changes the
IOP
S.C.C.O.
4/13/2015
29
IV. MEASUREMENT OF IOP
D. Goldmann Tonometry
– 1. The most accurate method for IOP
measurement
– 2. Readings within 1 - 2 mm of actual IOP
– 3. Flattens a small portion of the cornea
S.C.C.O.
4/13/2015
30
S.C.C.O.
4/13/2015
31
S.C.C.O.
4/13/2015
32
S.C.C.O.
4/13/2015
33
S.C.C.O.
4/13/2015
34
S.C.C.O.
4/13/2015
35
IV. MEASUREMENT OF IOP
– 4. Theory
a.
the cornea is covered with a tear layer which
exerts a surface tension (force in towards the
cornea)
b. a probe applied to the cornea is acted
against (a force pushing out from the cornea)
by the corneal thickness and elasticity (the
bending force)
S.C.C.O.
4/13/2015
36
S.C.C.O.
4/13/2015
37
c.
if the area of the probe is of the proper size
then the force from the surface tension will
cancel the bending force
S.C.C.O.
4/13/2015
38
IV. MEASUREMENT OF IOP
d.
this leaves
– Pressure = Force / Area
e.
the area of the probe has a diameter of 3.06
mm
S.C.C.O.
4/13/2015
39
S.C.C.O.
4/13/2015
40
IV. MEASUREMENT OF IOP
– 5. Procedure
a.
instill fluorescein into the tear layer
b. view fluorescein pattern with the blue light on
the slit lamp
c. doubling prism in place to split the view in
half
d. image of the split circle must be lined up
e. pressure = the number on the drum times 10
in mm Hg.
S.C.C.O.
4/13/2015
41
IV. MEASUREMENT OF IOP
– 6. Sources of Error
a.
improper width or position of mires
b. inappropriate fluorescein levels
c. unusual corneal thickness
S.C.C.O.
4/13/2015
42
S.C.C.O.
4/13/2015
43
IV. MEASUREMENT OF IOP
– 7. Advantages of Goldmann Tonometry
a.
highly accurate and reliable (procedure does
not influence IOP)
b. accepted norm for IOP measurement
c. easy to perform
d. not very expensive (about $1000)
S.C.C.O.
4/13/2015
44
IV. MEASUREMENT OF IOP
– 8. Disadvantages of Goldmann Tonometry
a.
requires anesthesia
b. can result in an abrasion
c. must sterilize instrument after each use
d. not portable
S.C.C.O.
4/13/2015
45
IV. MEASUREMENT OF IOP
E. Noncontact Tonometer
– 1. Achieves corneal flattening by an air jet
of calibrated, increasing force
– 2. Corneal flattening is detected by a photo
cell
– 3. From the known force of the air jet and
the dimensions of the air jet the pressure is
calculated
S.C.C.O.
4/13/2015
46
S.C.C.O.
4/13/2015
47
IV. MEASUREMENT OF IOP
– 4. The higher the IOP the longer it takes to
flatten the cornea (i.e., if IOP = 17 mm Hg,
flattening takes 10.5 msec; if IOP = 36 mm
Hg, flattening takes 24 msec)
– 5. Advantages of NCT
a.
no anesthesia required
b. fairly reliable for pressures in the normal
range (less reliable as the pressure increases)
c. quick and easy to perform
d. does not touch the eye (can use on diseased
eyes)
S.C.C.O.
4/13/2015
48
IV. MEASUREMENT OF IOP
– 6. Disadvantages of NCT
a.
expensive (over $5000)
b. not accurate at high pressures
c. patient apprehension (puff) raises IOP
d. not easily portable
S.C.C.O.
4/13/2015
49
V. IOP AND GLAUCOMA
A. If the IOP is high enough for a long
enough time, the patient will lose visual
field in a characteristic pattern
B. If the angle is totally blocked the
pressure rises to 55 or 60 mm Hg and
field loss is seen in a few hours with
total loss in a few days
S.C.C.O.
4/13/2015
50
V. IOP AND GLAUCOMA
C. In open angle glaucoma the pressure
is more often in the 20's or 30's
– 1. this pressure can be tolerated for
months before damage occurs
– 2. sometimes patients with normal
pressure develop glaucomatous changes
S.C.C.O.
4/13/2015
51
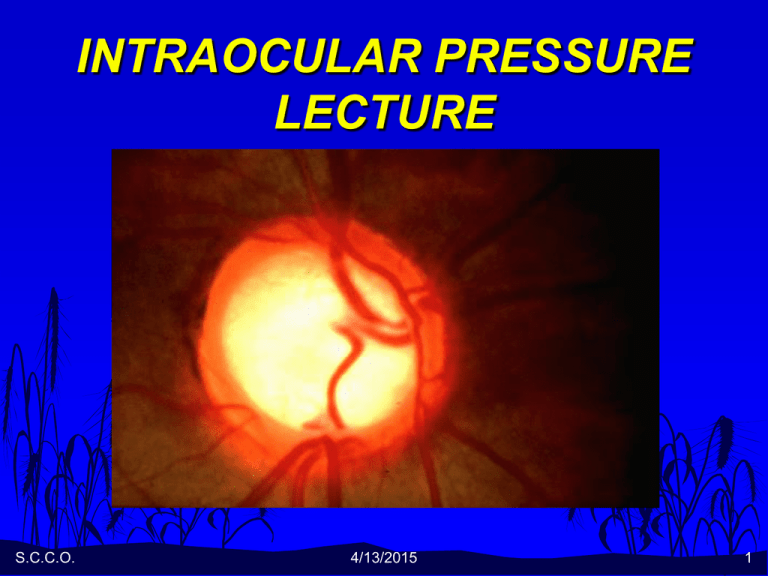
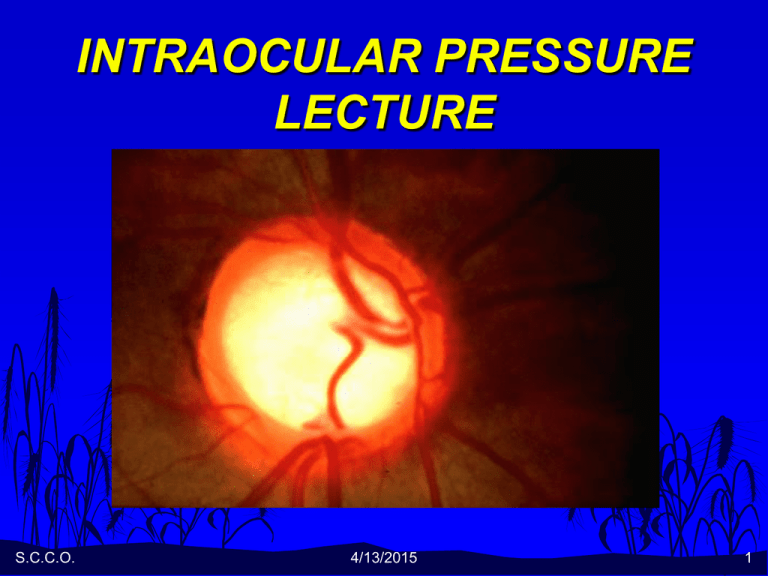
V. IOP AND GLAUCOMA
D. To diagnose glaucoma usually need:
– 1. high IOP
– 2. visual field defects
– 3. cupping at the disc
S.C.C.O.
4/13/2015
52
S.C.C.O.
4/13/2015
53
S.C.C.O.
4/13/2015
54
S.C.C.O.
4/13/2015
55
S.C.C.O.
4/13/2015
56