Chronic Visual Loss
advertisement

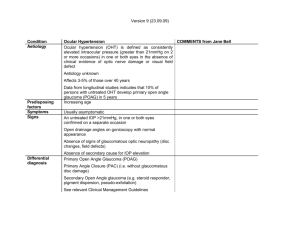
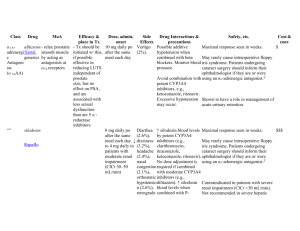
Chronic Visual Loss UBC Ophthalmology Club 2012 Approach History, physical, tests Patient population tends to be the elderly, but 2% of adults in the US over age 40 have vision <20/40 (Congdon et al. 2004. Arch Ophthalmol 122(4):477-85.) Prevalence increases with age Early detection may lead to early intervention and preservation of vision Primary care is the first screen, know when to refer Case 1 55M comes to GP for routine physical Has HTN, currently on thiazide Denies visual loss, eye pain, headaches Sister was taking an eye drop but not sure what that’s for Exam: OD 20/30 OS 20/30 (both 20/25 2 years ago) Pupils equal reactive No RAPD EOM full Confrontational VF grossly intact Case 1 Photo courtesy Dr. Fred Mikelberg Management: A. This pt needs urgent treatment to lower his IOP B. Refer pt to ophthalmologist 1-2 weeks C. Reassess pt in 3 months D. Increase his thiazide dose and consider adding a second antihypertensive Transillumination defect. (Kuo & Noecker, AAO 2009) Pseudoexfoliation. (Shaw, AAO 2003) Primary Open Angle Glaucoma Progressive optic neuropathy of unknown etiology with persistent VF defect Risk factors incl. elevated IOP, family hx, race, age, myopia Sx incl. gradual loss of peripheral visual field Further tests: VF testing of this pt reveals nasal step defect IOP: OD 29mmHg, OS 23mmHg Retina tomography shows moderate thinning of nerve fibre layer AAO recommends refer pt when: disc:cup >0.5 or one cup significantly larger than the other IOP > 21mmHg or >5mmHg difference between the eyes Sx of acute glaucoma Common Rx for glaucoma The only pharmacological target is lowering IOP Alpha agonists(↑drain, ↓aq): clonidine, brimonidine Beta blocker (↓aq): timolol CA inhibitor (↓aq): acetazolamide (Diamox) Prostaglandin analog (↑drain): latanoprost (Xalatan) SE of PG analog- iris color change and longer eye lashes Case 2 70M c/o decreasing vision in both eyes over last 6 months to GP This is particularly bothersome as he is having more trouble reading and watching TV No eye conditions in the past Hx significant for obesity and 50 pkyr smoking, quit 5 years ago Family history unremarkable Case 2 OD 20/80, OS 20/100 (last 2 years decreased) Pupils equal reactive EOM full CVF intact IOP within normal limits Fundoscopy: Amsler grid: (Khanifar et al. Retinal Physician, 2007) What do you tell this patient? A. he has missed the window for effective intervention B. he needs immediate antioxidant and zinc supplement C. his children are at increased risk of this disease D. his condition probably won’t cause complete blindness Age Related Macular Degeneration 2 forms: atrophic (dry) and exudative (wet) Leading cause of blindness in adults >75 yr, mostly from exudative form Multifactorial disease, see characteristic drusen Early diagnosis enables detection of exudative form, which can be effectively treated with anti-VEGF agents Screening in primary care: Visual distortions, especially in central vision Presence of drusen in macula, retinal pigment breakdown Refer to ophthalmologist for full evaluation Wet AMD Monthly injection, $1600 per shot Case 3 68F comes to GP with c/o decreased vision in her L eye She denies double vision or glares, in fact she said she can read better with her L eye than her R eye now; she wants to know if her reading glasses are still necessary No eye disease or trauma No family hx of eye diseases Meds include prednisone 20 mg daily for last 2 months for RA flare Case 3 (Espandar, AAO 2009) OD 20/30, OS 20/50 Pupils equal reactive no RAPD EOM full Confrontational VF full Fundus visualized, unremarkable Management What’s your course of action? A. Inform pt that her cataract is the result of her prednisone use B. This pt needs to see an ophthalmologist STAT because of risk of irreversible visual loss C. This pt’s presbyopia is improving so she should be followed up in 6 months at your office D. Referral to ophthalmologist for evaluation and treatment options Cataract Etiology: opacified lens Most commonly associated with increasing age, but also congenital, DM, steroid use, trauma, radiation Pt complain of painless gradual unilateral vision decrease “Second sight” refers to myopic shift as cataract increases power of lens; this is temporary Referral to ophthalmologist when decrease in vision becomes symptomatic and/or interfere with function Cataract removal+IOL implant is one of the most frequently-performed and successful procedures in all of surgery Other types of cataracts Cortical cataract Posterior subcapsular cataract Implantable IOL Case 4 63M with 17 yr hx of Type 2 DM comes to GP to c/o decrease in vision in both eyes Denies pain, distortions, double vision Hb A1c 7.5% despite being on metformin and gliclazide Also has dyslipidemia, on atorvastatin No previous eye complaints Case 4 (AAO, 2012) OD 20/40, OS 20/60 Pupils equal reactive, red reflex present EOM full VF intact AC deep and quiet Fundoscopy: Diagnosis What is the cause of this pt’s decreased vision? A. Non-proliferative diabetic retinopathy B. Age related macular degeneration C. Proliferative diabetic retinopathy D. Branch retinal vein occlusion Diabetic retinopathy Microvascular complication of DM Most common cause of vision loss in adults 25-74 yr In NPDR, vision loss arise from macular edema In PDR, vision loss can be rapid, secondary to scarring and vitreous hemorrhage Ophthalmologist referral when: Newly diagnosed DM patient Eye exam every 1-2 years after Patient who develop rapid vision change Glycemic control is the cornerstone of systemic management. DR is managed with laser and anti-VEGF PDR Proliferative disease, characterized by formation of new and fragile vessels that form a tangle on the disc and elsewhere. Pan-retinal photocoagulation uses laser to destroy ischemic retina in order to prevent neovascularization and preserve the macula. Summary 4 most common causes of chronic visual loss and their features: Open angle glaucoma- insidious, treat IOP Age related macular degeneration- distortions, most common Cataract- often unilateral, good result with surgery Diabetic retinopathy- check in all DM pt, bilateral visual loss All are either reversible or can be managed well (slow/stop vision loss) if detected early Therefore, primary care’s role is vital in screening of chronic eye diseases Questions? Edited by: Steven Schendel, PGY-4 Reviewed by: Drs. Fred Mikelberg, David Maberley, Francis Law Contact: R Tom Liu rztom.liu@gmail.com