Update on Prostaglandin Analogues Used for the Treatment of
advertisement

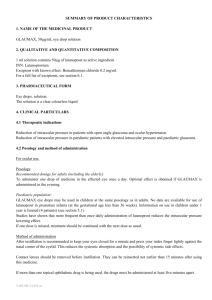
Update on Prostaglandin Analogues Used for the Treatment of Glaucoma 1 Learning Objectives Review the structure and mechanism of action of the commonly used prostaglandin analogues for treatment of glaucoma Review the efficacy of the commonly used prostaglandin analogues Know the side effects commonly associated with prostaglandins 2 Introduction Prostaglandin analogues are currently used as a first-line treatment for glaucoma because they effectively lower IOP Each prostaglandin analogue has a unique receptor-binding profile, but most agents have similar efficacy Compared with other antiglaucoma medications, prostaglandin analogues: – Reduce IOP to a greater extent – Provide good control over IOP fluctuations – Produce few systemic adverse events Prostaglandin analogues have similar side effects – Cause different degrees of hyperaemia, iris pigmentation changes, and eyelash growth IOP = intraocular pressure Marquis RE et al. Drugs Aging. 2005;22(1):1–21; Parrish RK et al. Am J Ophthalmol. 2003;135:688–703; Takagi Y et al. Exp Eye Res. 2004;78:767–776; van der Valk R et al. Ophthalmology. 2005;112:1177–1185; Holló G. Expert Opin Drug Saf. 2007;6(1):45–52. 3 Prostaglandin Analogues: Structure PGF2α = prostaglandin F2α Adapted with permission from Takagi Y et al. Exp Eye Res. 2004;78:767–776 and Marquis RE et al. Management of glaucoma: focus on pharmacological therapy. Drugs Aging. 2005;22(1):1–21. 4 Prostaglandin Analogues: Mechanism of Action FP = prostaglandin F Adapted with permission from Weinreb RN et al. Prostaglandin effects on the uveoscleral outflow pathway. In: Krieglsten GK, ed. Glaucoma Update VI; Springer-Verlag, Berlin. 2000:197–202. 5 SAFLUTAN™† (tafluprost) Has High FP Receptor Affinity: 12 Times Greater Than Latanoprost Prostaglandin Receptor-Binding Affinity (Moles per Liter)a Prostaglandin Analogueb FP EP1 EP2 EP3 IP/DP TP PGF2α 1.2 × 10−8 3.2 × 10−7 6.4 × 10−6 1.6 × 10−7 >10−4 > 10−4 Latanoprost acid 1.0 × 10−8 5.0 × 10−6 >10−4 2.8 × 10−5 >10−4 > 10−4 Travoprost 3.5 × 10−9 3.0 × 10−8 >10−4 2.4 × 10−5 >10−4 > 10−4 Bimatoprost 4.5 × 10−9 6.5 × 10−7 >10−4 >10−4 >10−4 3.4 × 10−5 Tafluprost 0.5 × 10−9 >10−6 >10−6 6.7 × 10−8 >10−6 > 10−6 Higher FP affinity has not been correlated with an increase in either efficacy or safety EC50 = half maximal effective concentration; FP = prostaglandin F; PGF2α = prostaglandin F2α aReceptor binding assessed according to EC 50 values. bData refer to active drug product. Stjernschantz JW. From PGF2α-isopropyl ester to latanoprost: a review of the development of Xalantan. Inv Ophthalmol Vis Sci. 2001;42(6):1134–1145; Stjernschantz JW et al. Mechanism and clinical significance of prostaglandininduced iris pigmentation. Surv Ophthalmol. 2002;47(suppl 1):S162–S175; Takagi Y et al. Exp Eye Res. 2004;78:767–776. †SAFLUTAN is a trademark of Merck & Co., Inc., Whitehouse Station, NJ, USA. 6 Substantial IOP-Lowering Efficacy of Prostaglandin Analogues is Consistent Across Products 40 Latanoprost Bimatoprost Travoprost IOP Reduction (%) 35 30 25 20 15 10 5 0 08:00 12:00 16:00 20:00 Time IOP = intraocular pressure Parrish RK et al. Am J Ophthalmol. 2003;135(5):688–703. 7 Prostaglandin Analogues Show Comparable Efficacy IOP Reduction Mean IOP Reduction (mmHg) at 8:00 Across Published Comparative Trials 0 Parrish N = 410 12 weeks Netland N = 390 12 months Gandolfi N = 232 3 months Noecker N = 269 6 months Multi-center, randomized, investigator-masked studies of patients with ocular hypertension or primary open-angle glaucoma. Study drugs given once daily. -6 p < 0.001 Latanoprost 0.005% Bimatoprost 0.03% -12 Travoprost 0.004% IOP = intraocular pressure Parrish RK et al. Am J Ophthalmol. 2003;135:688–703; Netland PA et al. Am J Ophthalmol. 2001;132:472–484; Gandolfi S et al. Adv Ther. 2001;18(3):110–121; Noecker RS et al. Am J Ophthalmol. 2003;135:55–63. 8 IOP-Lowering Efficacy: Prostaglandin Analogues vs Other Antiglaucoma Treatments Mean Change From Baseline as % Change in IOP Treatment Peak Trough Bimatoprost 33 28 Travoprost 31 29 Latanoprost 31 28 Timolol 27 26 Brimonidine 25 18 Betaxolol 23 20 Dorzolamide 22 17 Brinzolamide 17 17 IOP = intraocular pressure Adapted with permission from van der Valk R et al. Ophthalmology. 2005;112:1177–1185. 9 Adverse Events Associated With Prostaglandin Analogues Prostaglandin analogues have a better systemic safety profile than other antiglaucoma therapies Common side effects of prostaglandin analogues: – Conjunctival hyperaemia – Iris pigmentation changes – Eyelash growth Marquis RE et al. Drugs Aging. 2005;22(1):1–21; Holló G. Expert Opin Drug Saf. 2007;6(1):45–52. 10 Conjunctival Hyperaemia With Prostaglandin Analogues 80 70 Patients (%) 60 50 40 30 20 10 0 Latanoprost Bimatoprost Travoprost Parrish RK et al. Am J Ophthalmol. 2003;135:688–703; Stewart WC et al. Am J Ophthalmol. 2003;135:314–320. 11 Conjunctival Hyperaemia With Prostaglandin Analogues (cont) 50 Patients (%) 40 30 20 10 0 Xalatan® (latanoprost) Travatan® (travoprost) Lumigan® (bimatoprost) Xalatan Summary of Product Characteristics. Pharmacia Ltd., Kent, UK.: 2007; Travatan Summary of Product Characteristics. Alcon Laboratories (UK) Ltd., Hemel Hempstead, UK.: 2006; Lumigan Summary of Product Characteristics. Allergan Ltd., Marlow, Bucks, UK.: 2007. 12 Conclusions The IOP-lowering effect of prostaglandin analogues is primarily mediated by the FP receptor Prostaglandin analogues have similar and substantial IOP lowering effects Compared with other antiglaucoma medications, prostaglandin analogues: – Reduce IOP to a greater extent – Produce fewer systemic adverse events Ocular side effects are common to all prostaglandin analogues – Conjunctival hyperaemia, which occurs with varying frequencies among these medications – Iris pigmentation changes – Eyelash growth FP = prostaglandin F; IOP = intraocular pressure Takagi Y et al. Exp Eye Res. 2004;78:767–776; Parrish RK et al. Am J Ophthalmol. 2003;135:688–703; van der Valk R et al. Ophthalmology. 2005;112:1177–1185; Marquis RE et al. Drugs Aging. 2005;22(1):1–21; Holló G. Expert Opin Drug Saf. 2007;6(1):45–52. 13