Slide 1
advertisement

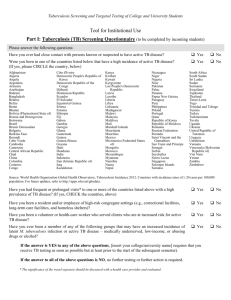
Paediatric tuberculosis Beate Kampmann FRCPCH PhD A/Professor in Paediatric Infection & Immunity Consultant Paediatrician Imperial College London, UK and Institute of Infectious Diseases and Molecular Medicine University of Cape Town, RSA Overview • What is special about TB in children? • Epidemiology- who are our patients? • Clinical presentations • How can we make the diagnosis? • New Immunological Tools-how helpful are they? • Issues in TB therapy in children • Future research topics Tuberculosis in Children…. the problem • Significant Morbidity and Mortality 1.4 million cases annually (95% developing countries) 450,000 Deaths estimated 10-15% of global burden related to childhood TB • Different clinical spectrum of disease 5-10% < 2 yr meningitis disseminated disease more common • Co infection with HIV- clinically very difficult to distinguish • Remains a diagnostic challenge paucibacillary, rarely culture confirmed : Sputum smear positive in 10.3% (10-14yr), 1.8% (5-9) and1.6% (<5) Cultures positive 21% (10-14), 5% (5-9) and 4.2% (<5), Tuberculosis in Children differs from adults • Immune responses are Age-dependent: Following infection 40% < 2 yr, 25% 2-5 yr and 5-15% of older children will develop disease within 2 years • Majority of disease results from progression of primary infection rather than reactivation might affect detectable immune responses • More likely to be extrapulmonary and disseminated, particularly in infants Newton, Kampmann The Lancet Infectious Diseases, August 2008; Vol 8: 498-510 Percentage of TB cases of foreign origin, 2006 Not included or not reporting to EuroTB 0% – 4% 5% – 19% 20% – 49% > 49% Andorra Malta Monaco San Marino Trends in incidence of TB in children under 15 years by ethnic group in London, 2001-2006 UK: Tuberculosis rates in persons born abroad by age Development of TB in immigrant children Sources: Enhanced Tuberculosis Surveillance, Labour Force Survey population estimates, Abubakar et al Arch. Dis. Child. 2008;93;1017-1021; Children with TB at Imperial HCT: Ethnicity and country of birth: south asian 29% Travel to TB endemic countries yes black african 47% arab 5% no dk hous ehold black african afro-caribbean caucasian SE asian mixed race arab no south asian caucasian 7% 39% vis itor yes 56% afro-caribbean 2% no Country of Birth 28% UK 38% dk 4% household 62% dk dk 5% mixed race 4% SE asianvisitor 6% 6% no non- UK 62% UK non-U K Children acquire TB from (household) contacts If you ask yourself, does this child have TB, ask yourself: is there TB in this family? Or: if you see adults with TB, ask yourself if they have children Presentation of PAEDIATRIC TB Case 1 -14 month Asian girl -previously well, no F/H of TB -3 weeks cough and unwell -admitted to local hospital -low grade fever -normal chest examination WHAT INVESTIGATIONS WOULD YOU DO? PAEDIATRIC TB Case 1 Mantoux test: 2mm Gastric washings; - microscopy and (later) culture negative -Rx. Erythromycin and Augmentin -no improvement on antibiotics -bronchoscopy planned PAEDIATRIC TB Case 1 1 day before bronchoscopy: - afebrile, less cough, looking well -continued improvement, - discharged home, no ∆ PAEDIATRIC TB Case 1 out-patient review 6 weeks later: -completely well, thriving, no cough “Grandfather admitted to local hospital with pulmonary TB” -repeat Mantoux: now 25mm -TB treatment commenced PAEDIATRIC TB Case 1 Discussion Points Primary TB in children: - spontaneous recovery is possible - diagnosis is difficult - no visible AFB - cultures usually negative - tuberculin test negative CHILDHOOD EXPOSURE PRIMARY PULMONARY INFECTION Successful immune response WELL ADULT IMMUNITY (live MTB) LATE REACTIVATION OF PULMONARY DISEASE FORMS CAVITY CHILDHOOD EXPOSURE PRIMARY PULMONARY INFECTION Self healing?? Inadequate immune response PROGRESSIVE PULMONARY DISEASE Lympho/ haematogenous spread MILIARY TB or EXTRA-PULMONARY DISEASE CHILDHOOD EXPOSURE PRIMARY PULMONARY INFECTION Inadequate immune response -most serious form of TB, fatal if untreated -most common in < 2 year-olds -worst prognosis in < 2 year-olds -insidious onset; PROGRESSIVE PULMONARY DISEASE Lympho/ haematogenous spread MILLIARY, EXTRA-PULMONARY DISEASE TB MENINGITIS TB MENINGITIS Primary focus in lung VI NERVE PALSY Brain focus (Rich focus) Meninges CSF Severe granulomatous inflammatory response BRAIN INFARCTION CSF protein ICP Cranial nerve palsies Vascular occlusions Hydrocephalus Thick gelatinous exudate forms, envelopes base of brain TB MENINGITIS CSF -lymphocytes, low sugar, high protein, AFB may be visible -but often -polymorphs initially -protein normal initially -no visible organisms -sugar normal initially So: repeat LP, neuro-imaging, CXR, contacts CT scan; enhanced Ring enhancing tuberculomata MRI > SENSITIVITY THAN CT ENHANCED CT SCAN GADALLINIUM ENHANCED MRI HYDROCEPHALUS TB MENINGITIS SUCCESS of Rx DEPENDS ON EARLY DIAGNOSIS TB MENINGITIS TREATMENT with quadruple therapy Drugs: -? CSF penetration - duration - sensitivity Adjunctive therapy: - steroids - SIADH - acetazolamide - surgery Diagnostic tests Microbiological Organism smear culture DNA The “gold-standard” Appearance in sputum Appearance in culture ‘cording’ PAEDIATRIC TB: Implications of bacterial load Paediatric TB: 106 bacteria Adult TB: >109 bacteria - children less infectious - difficulty in confirming diagnosis (< 30%) - difficulty in detecting resistance Diagnostic tests Immunological Host response skin test antigen-specific production of IFNγ Acknowledgement & Thanks IGRA and the diagnosis of active TB Signs and symptoms Contact history Travel Active TB Radiology Microbiology TST IGRA TUBERCULIN SKIN TEST (used since 1890) -technically difficult in children -UK : 2 units of SSI tuberculin (PPD) - > 200 antigens, Read-out: -degree of hypersensitivity to PPD Problems with the TST: -poor specificity,does not distinguish between; -TB disease -TB infection -BCG -non-typical mycobacteria poor sensitivity, can be falsely negative in; -early infection -disseminated disease -severe malnutrition -other acute infections (measles, pertussis) -live vaccines -immunocompromised (HIV) *In children a negative TST does not exclude TB Gene deletions and the origin of BCG major antigens ESAT6 and CFP10 M. tuberculosis 10 deletions 64 genes M. bovis 4/5 deletions RD1 region 30/40 genes BCG substrains T cell tests (interferon-g) that distinguish M. tuberculosis infection from BCG vaccination IFN-responses to specific antigens by ELISPOT or Whole Blood Assay Unable to distinguish between TB and BCG effect Clear difference between acute TB and BCG vaccination Van Pinxteren Clin Diagn Lab Immunol 2000 IGRA and National TB guidelines UK: NICE Guidelines 2006 http://guidance.nice.org.uk/CG33 2 commercially available assays Antigens used: ESAT-6 CFP10 +/- TB7.7 mitogen negative control In principal: can both distinguish between BCG vaccination and M.tuberculosis infection But: Paucity of data in children Confusion about use of IGRA Principal of Quantiferon Gold In vitro blood test: Coating antibody Biotinylated 2nd ELISPOT assay PBMC+antigen antibody IFN-production Avidin-peroxidase Each spot is an individual T cell that has released IFN IGRA versus TST: our own research Spot the Difference Interferon-release assays (IGRA) in paediatric active and latent tuberculosis in London - a side-by-side comparison with TST Kampmann B, Whittaker E, Williams A, Walters S, Gordon A, Martinez-Alier N, Williams B, Crook AM, Hutton AM, Anderson ST. Interferon- gamma release assays do not identify more children with active TB than TST. Eur Respir J. 2009 Jun;33(6):1374-8 Acknowledgement & Thanks IGRA and the diagnosis of active TB Re sults (%) of all thre e te s tin the diffe rent sub-groupsof Active TB TST QFG-IT Tspot.TB All active TB (N=91) De finite (N=25) Probable (N=38) De finite & Probable (N=63) Pos s ible (N=28) >15 6-15 <6 + - Ind + - TF 43 19 38 46 45 9 38 53 9 83 8 8 80 12 8 58 38 4 45 30 26 52 42 5 45 45 10 60 21 19 64 29 6 50 42 8 7 14 79 7 79 14 11 79 11 IGRA missed between 20-40% of definite active TB Thanks Combining IGRAAcknowledgement and TST in the&diagnosis of active TB A combination of TST and IGRA increases sensitivity to above 93% & Thanks IGRA and the Acknowledgement diagnosis of active TB- other studies • Bamford et al, Arch Dis Child 2009 Oct 8 (Epub ahead of print) UK-wide study of 333 children from 6 large UK centers, 49 with culture-confirmed TB: TST had a sensitivity of 82%, Quantiferon-Gold in tube (QFT-IT) had a sensitivity of 78% and T-Spot.TB of 66%. Neither IGRA performed significantly better than a TST with a cut-off of 15 mm. Combining results of TST and IGRA increased the sensitivity to 96% for TST plus T-Spot.TB and 91% for TST plus QFG-IT in the definite TB cohort. • Nicol et al; Pediatrics 2009,Jan; 123(1): 38-43 Comparison of T-SPOT.TB assay and TST for the evaluation of young children at high risk for tuberculosis Sensitivity of the T-SPOT.TB was no better than that of the tuberculin skin test (>10mm) for culture-confirmed tuberculosis (n=10) (50% T-Spot and 80% TST) and was poorer for the combined group of culture-confirmed and clinically probable tuberculosis (n=58) (40% T-Spot and 52% TST). • Bianchi et al, PIDJ 2009, Jun;28(6):510-4 IGRA was positive in 15 of 16 (93.8%) children with active pulmonary TB • Connell et al, Thorax 2006, Jul;61(7):616-20 The whole blood IFN-gamma assay was positive in all 9 children (100%) with TB disease. Acknowledgement & Thanks IGRA and the diagnosis of active TB A negative IGRA does not exclude active TB IGRA is not a “rule-out”- test, but can add value to additional investigations Acknowledgement & Thanks IGRA and the diagnosis of latent TB Contact history Travel/Immig ration Absence of clinical signs and symptoms Latent TB negative Radiology TST IGRA IGRA and the diagnosis of latent TB • No “gold standard” for LTBI • Acknowledged discrepancy of TST and IGRA results - due to poor specificity of TST (Kampmann ERJ 2009, Connell PlosOne 2008, Bianchi PIDJ 2009) • Which IGRA is better? - Good agreement between 2 IGRAS (92%, k=0.82) (similar to Connell et al, PLoS One. 2008 Jul: agreement between QFT-IT and T-SPOT.TB 93%, k=0.83). • Currently: ? “over-treatment” by paediatricians - but: to date no studies of negative predictive value of IGRA in children • Performance in very young children- conflicting messages • Increased sensitivity in immuno-compromised hosts Conclusion 2: Latent TB • Good agreement between 2 IGRAS (92%, k=0.82) • “over-treatment” by Paediatricians, compared to NICE recommendations • How many children will develop TB if TST> 15, but untreated with chemopro as IGRA negative? • How many children have neg TST but would have had pos IGRA at screening • Longitudinal survey required Conclusions • IGRA should not currently replace the • IGRA detect immune memory do not confirm the TSTbut in children presence or absence of M. tuberculosis- active or latent • higher specificity than TST not forget the many • we the should additional challenging question in • designed to test for evidence of TB infection, not TB disease childhood TB • can be used as a rule-in testmicrobiological for active TB in children, better diagnostics better biomarkers than IFN but not as a rule-out test better vaccines • higher sensitivity in immunocompromised patients compared to TST improved understanding of primary TB TB treatment in children • Treatment regimens are adopted from adult schemes • Children respond very well to treatment, incl DOTS • Dosages need to be adjusted for weight: • Pharmakokinetics in children differ from adults - INH- 5-10 mg/kg, rapid acetylators (1) - Ethambutol 15-25 mg/kg (2) •Problems with treating TB in the HIV-infected child on ART 1: Schaaf et al, Arch Dis Child 2005; 90:614 2: Donald et al, Int J Tuberc Lung Dis 2006; 10:1318 Drugs and ADHERENCE IF YOU DON’T TAKE THE DRUGS, THEY WON’T WORK PAEDIATRIC TB POOR ADHERENCE Support -hospital TB clinic -community -health care workers -social services -DOT (Directly Observed Therapy) -accurate record of treatment -successful treatment -prevention of resistance -different adult -different location Take Home messages: • Think of the diagnosis, especially in the epidemiological context • TB is a family disease • The diagnosis of active TB in children is based on a jigsaw of findings • IGRA can be an additional piece in the jigsaw, but a negative IGRA does not exclude active TB • TB therapy needs a lot of support for families • founded in April 2009, branch of TBNET • to date: members from 15 European countries, incl. Eastern Europe • includes clinicians, epidemiologists and laboratory scientists Aims • enhance the understanding of the pediatric aspects of tuberculosis • facilitate collaborative research studies for childhood TB in Europe • provide expert opinion through excellence in science and teaching • establish a better evidence base for diagnosis and treatment of TB in children Research questions - immunological mechanisms of age related susceptibility to TB - Epidemiology of childhood TB - MDR /XDR TB in children - Performance/evaluation of new diagnostics - New drugs - New vaccines Thank you Any questions? E-mail: b.kampmann@imperial.ac.uk Website: www1.imperial.ac.uk/medicine/people/b.kampmann/