Pelvic Floor Prolapse
advertisement

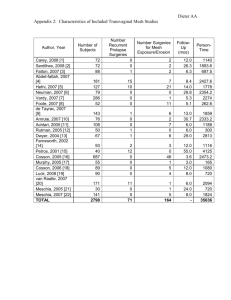
Pelvic Organ Prolapse : Overview of Causes and Surgical Options Vincent Tse MB BS ( Hons ) MS ( Syd ) FRACS Male and Female Incontinence Urodynamics Neuro-urology Pelvic Floor Reconstructive Surgery Department of Urology, Concord Hospital, Sydney, NSW “Pelvic Floor Reconstructive Surgery” Recent time becoming a cross-disciplinary field – Gynaecologist – Urologist – Colorectal surgeon the PELVIC FLOOR SURGEON Common interest and training in pelvic floor dysfunction Various national and international societies collaborating research in this growing area What is POP ? Herniation of adjacent structures into vagina What is Pelvic Organ Prolapse ? (POP) Herniation of various pelvic structures adjacent to the vagina Can be in the form of : • • • • anterior compartment – cystocele vault – enterocele/uterine prolapse posterior compartment – rectocele perineum – perineal descent POP Prevalence 20-30% in multiparous 2% in nulliparous 20% in post-gynaecological surgery 10% in requiring POP surgery in lifetime Pathophysiology of POP • Central is genetic predispositon – Age – Childbirth ( pudendal nerve injury denerevates levators) • One birth doubles POP risk • 10-15% increase every subsequent birth – Nerves – Collagen – Abdo pressure • BMI > 30 increases risk by 40-75% – Surgery • Burch • Hysterectomy Pathophysiology of POP ... Leading to herniation of various pelvic structures adjacent to the vagina from DETACHMENT or DISRUPTION Types of Defects Detachment – vagina is broken away from the pelvis and needs to be reattached Disruption – vaginal structure is torn and needs to be patched or repaired Normal Pelvic Support Muscle • Levator ani ( ‘pelvic floor muscle’) • Obturator muscles Ligaments • Endopelvic fascia » Pubourethral, urethropelvic, vesicopelvic, cardinal, uterosacral, rectovaginal septum … Nerves Blood Supply Level 1 support – vault/uterine prolapse Level 2 Support – cystocele, enterocele,recto cele Level 3 Support – Perineal descent,low rectocele LEVEL 2 and LEVEL 3 SUPPORTS Level 2 Support Defects - Anterior Compartment : The Cystocele 2 types : – CENTRAL DEFECT – Defect in fascia between vagina and bladder – Loss of central rugae – Looks like a round bulge on Valsalva – LATERAL DEFECT – Defect in fascia supporting lateral bladder to pelvic side wall – Central rugae intact – Flat sagging anterior vagina – >80% are mixed Anterior Compartment Prolapse : Cystocele Patient may present with : – – – – – – – Asymptomatic ‘bulge’ or pressure in vagina Often worse at end of day Back ache Irritation from contact with underwear Voiding difficulty and Recurrent UTIs Obstructive uropathy Cystocele are often accompanied by : – Prolapse of other compartments prolapse ( eg. vault or rectocele ) – STRESS incontinence Grading of Pelvic Organ Prolapse ( POP ) Baden-Walker ( older, more clinically useful ) • • • • Grade 1: minimal displacement with straining Grade 2: towards introitus with straining Grade 3: to and beyond level of introitus with straining Grade 4 : outside introitus at rest POP-Q ( newer … ) • Cumbersome and questionable clinical utility other than for research ( standardisation ) purposes Management Conservative • Simply observe • Vaginal ring pessary • Topical estrogen cream if indicated Surgical • Most pts need pre-operative urodynamics to exclude occult stress incontinence – Anterior colporraphy ( central defect ) – Paravaginal repair ( lateral defect ) • +/- TVT or fascial pubovaginal sling Type of Surgery Depends on … Detachment – vagina is broken away from the pelvis and needs to be reattached Disruption – vaginal structure is torn and needs to be patched or repaired Anterior Compartment • To Replace – Add mesh/biologic (graft augmentation) Mesh Use in PRIMARY Cystocele Repair Author Year Mesh N F- up mths Anatom. success % Infection% Vaginal erosion % Julian 1996 Marlex 12 24 100 0 8.3 Flood 1998 Marlex 142 36 94.4 3.5 2.1 Adhoute 2004 Gynemesh 52 27 95 0 3.8 Shah 2004 Prolene 29 25 93.3 0 6.7 Dwyer 2004 Atrium 47 29 94 0 7 Milani 2004 Prolene 63 17 94 0 13 de Tayrac 2007 Polypropylene 132 13 92.3 0 6.3 Hiltunin 2007 Polypropylene 104 12 93.3 (vs 61.5 AR) 0 17 Sivaslioglu 2008 Polypropylene 90 12 91 0 (vs 72% AR) 6.9 Nieminen 2008 Polypropylene 105 24 89 0 (vs 59% AR) 8.0 Level 2 Support Defects - Posterior Compartment: The Rectocele May present with : • • • • • • Asymptomatic Defecatory difficulty/constipation Digital manipulation of posterior vaginal wall Deep pelvic pain Back pain Urinary difficulty Entero-Rectocele Management Conservative • Bowel softeners • Exclude other possible low rectal conditions (eg. cancer) • Ring Pessary Surgical • • • • Pre-operative defecatory rectoproctography Posterior colporraphy Transanal Delorme repair Perineorraphy if perineal descent present Level 1 Support Defects : Vault / Uterine Prolapse Presentation often similar to cystocele Often co-exist with cystocele/rectocele Beware of the little old lady with unexplained back pain, recurrent UTIs, or renal failure – exclude PROLAPSE Procidentia Management Conservative • Observe • Ring pessary • Topical Estrogen if required Surgical • In general, – YOUNGER and SEXUALLY ACTIVE » Suspend to the sacrum – OLDER and NON-SEXUALLY ACTIVE » Suspend to the sacrospinous ligament Surgical Management : Level 1 FUNCTIONAL • To sacrum – Sacrocolpopexy/hysteropexy » Open, laparoscopic, robotic – Uterosacral ligament • To other level 1 sites – Sacrospinous ligament – Iliococcygeal fascia, etc NON-FUNCTIONAL • colpocleisis Open Sacrocolpopexy sigmoid Sacral promontory rectum vault bladder Transvaginal Sacrospinous Ligament Fixation Open vs Transvaginal Sacrocolpopexy Open • • • • • Level 1 evidence – most durable and effective Preserves vaginal axis hence less dyspareunia Lower complication profile Rx of choice for recurrence Longer stay and return to activity Transvaginal • • • • Equally effective but … Alters vaginal axis, hence higher dyspareunia rate ( 15%) May be more appropriate for the older, less sexually active Shorter stay and less invasive CONCLUSION Conclusion Causes of POP Level 1 and 2 support defects Overview of conservative and operative management of cystocele, rectocele and vault prolapse Take Home Messages Aetiology is multifactorial CAVEAT : pelvic examination in the elderly female with confusion, recurrent UTIs, unexplained renal impairment ! Conservative management with pessary Pelvic floor exercises may retard the progression of POP, but will not reverse any existing POP Management of pelvic prolapse are now managed by pelvic floor reconstructive surgeons who have had special training and may be a gynaecologist, urologist or colorectal surgeon ! Thank You for your Patience !