PPT - Cochin GUT Club

A rare case of psychosis
Dr. Sunil K Mathai
Dr Charles Panackel
Dept. of Gastroenterology
MTH Kochi, Kerala
Presenting Author – Dr Sunil K
Mathai HOD Gastroenterology
History
• 19 year male
• Student
• Change in behavior ~ 4 months
History
• Running amok
• Intermittent panic attacks
• GTCS
• Seen by a neurologist – Evaluated with CT
Brain and EEG and started on Valproate
History
• Continues to have abnormal behaviour
▫ Death of father – recent ‘stressor’
▫ Morning symptoms (? School phobia)
▫ Normal examination + CT brain
▫ No significant organic findings
? Functional (Panic disorder)
• Referred to a psychiatrist
Psychiatrist consulted
• Psychiatry evaluation and follow up
At MTH
• Continues to have symptoms and hence referred here.
• Basic Hematological Investigations – normal
• EEG, MRI brain– Normal
At MTH
• Has seizures in hospital
• Treated with Eptoin
• Blood results – RBS 40mg%
• Prompt recovery with IV dextrose
At MTH
• Recurrent Hypoglycemia ???
• Cause for hypoglycemia ???
• Insulin secreting Tumors
• Factitious
• Mesenchymal tumors
• Metabolic disorders
At MTH
• Sr. Insulin levels 27.1 microIU/ml (Normal <5)
• C –peptide level 694 pmol/L (Normal < 160)
• Insulin/Sugar Ratio 0.9
(Normal : 0.3-0.4)
• Sr. Prolactin – normal
• Sr. calcium – normal
• Low plasma glucose levels (less than 45 mg/dl)
+
• High serum insulin (>6 mU/ml)
• Suggestive of hypoglycemia secondary to an insulinoma
Provisional diagnosis – Insulinoma
What next ?
• Imaging study
CT abdomen with contrast
CT abdomen
• Single well circumscribed lesion in neck of pancreas
• Well enhancing in arterial phase
• Suggestive of Neuroendocrine tumor
(NET) of pancreas
PD
Endoscopic ultrasound EUS
• Pancreas – 2 echogenic lesions
1.
1.8 X 2 cm sized, well defined lesion near neck region
2.
0.7 cm sized lesion just proximal to first
Diagnosis
• Symptomatic Hypoglycemia
• Insulinoma Hyperinsulinemia
Management Plan
• Surgical removal – Enucleation
• Smaller lesion close to MPD – post operatively chance of pancreatic fistula
• ERCP + Elective PD stenting
Surgery
• Laparoscopic enucleation
• Intra operative ultrasound
Postoperative period
• Uneventful
• Rapid recovery
• Post OP – RBS : normal
Normal pancreas insulinoma
Encapsulated well diffrentiated pancreatic neuroendocrine tumours
Final diagnosis
• Symptomatic hypoglycemia
• Hypeinsulinemia
• Encapsulated well differentiated pancreatic neuroendocrine tumors (NET) - insulinoma
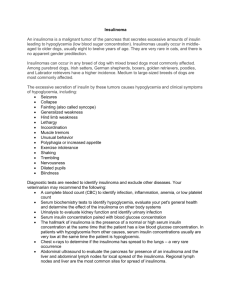
Insulinomas
• Large majority present in 4 th decade
• Women > men (3:2)
• Symptoms most common in early morning
• Sporadic / associated with MEN 1
Insulinomas - symptomatology
• Whipple’s triad
• Most patients have neuroglycopenic symptoms ~82 –
92%
▫ apathy, amnesia, dizziness, confusion, and coma
• Sympathetic overactivity
• Often misdiagnosed as ‘ Neurological / psychiatric illness’
Treatment of insulinoma
• Medical therapy
▫ Complex carbohydrates
▫ Diazoxide (150-200 mg/day)
▫ Octreotide / Lanreotide
• Surgical therapy
▫ Surgical exploration ( if no liver mets) – upto 80% curative
Take home message
• ‘Tubular vision’ in era of specialization
• Go back to ‘basics’
• Newer modalities available for treatment of insulinomas
• EUS & Intraoperative ultrasound are an essential tool
Thank you…
Special thanks to
• Dept. of surgical Gastroenterology
• Dept. of Endocrinology