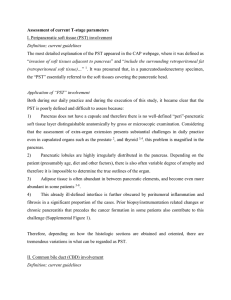
Pancreaticoduodenectomy

By Preston Paynter and Brielle Bowyer
Reasons for Procedure
Pancreatic Cancer
Chronic Pancreatitis
Severe trauma to the Pancreas
Diagnostic Procedures
CT scan
Needle biopsy
Cholangiopancreatography
Endoscopic ultrasound
Palpation of the pancreas
Procedure Summary
Resection
Part or all of the pancreas, duodenum, gallbladder, distal stomach and surrounding lymph nodes are identified and removed.
Reconstruction
Attachment of left over stomach, left over pancreas, and common bile duct to the jejunum.
**
Class II wound unless spillage occurs.
Supplies and Instrumentation
Supplies
Prep set
Basic pack
Basin set
Blades
○
○
#10
#11
Laparotomy drapes
Bovie
Suture
○ Doctors Pref.
Dressing
○ Doctors Pref.
Hemostatic agents
Suction
Head lamp
Instrumentation
Major instrument set
Vascular instruments
Biliary instruments (in room)
Long instruments
Bowl resection set
Retractors
○
○
Hand held
Self Retaining
Ligating clip appliers and clips
Staplers
Drains
Operative Prep
Anesthesia
General
Positioning
Supine with arms on arm boards
Skin Prep
Shave
Begin where incision will be.
Extends from chest to upper thighs and down to the table on both sides
Draping
Lap sheet outlined with towels
Incision
Left Sub-costal or upper midline
**Special consideration
-
Lubricate and protect the patient’s eyes
Operative Procedure
Resection
Incision is made
Exploration of the abdomen and assessment of the extent and resectability of the tumor is made.
Cholecystectomy
Removal of Lymph nodes in the surrounding area
Partial Gastrectomy
Vagotomy
Division of the Pancreas
Dissection of the retro-pancreatic vessels
Removal of Duodenum
Operative Procedure
Reconstruction
Pancreaticojejunostomy
Hepaticojejunostomy
End-to-side gastrojejunostomy
NG tube placed
Drains placed behind the pacreatic and biliary anastomoses
Stab wound made on the right side of the abdomen where drain tube exits.
Secured at the skin level with 3-0 silk
Counts take place
4 total Counts
Abdomen closed
Post-Op
Immediate Postoperative Care
Transport to PACU
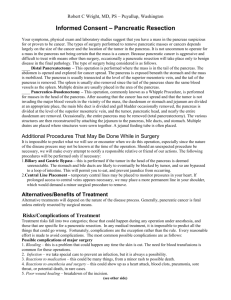
Possible Complications
Hemorrhage
Wound Infection
Fistula formation
Recurrence of Pathology
Leakage of Anastomosis
Nutritional/Digestive concerns
Ileus
Prognosis
Depends on response to primary condition
Mortality rate is 5% when surgery is performed by an experienced surgeon.