Understanding and Treatment of Infantile Nystagmus Syndrome
advertisement
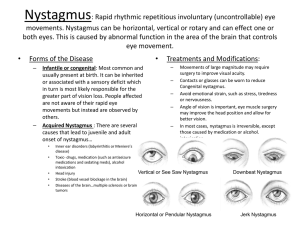
Understanding and Treatment of Infantile Nystagmus Syndrome Richard W. Hertle, MD, FAAO, FACS, FAAP Chief of Pediatric Ophthalmology, Children’s Hospital of Pittsburgh Director of Ocular Motility, The UPMC Eye Center Professor of Ophthalmology, The University of Pittsburgh The Laboratory of Visual and Ocular Motor Neurophysiology Examination Techniques: Highlights • Acuity Binocular and Monocular Gaze-Dependent • Color, Contrast • Ocular Motor Strabismus Nystagmus – “nulls” Head Posture • Accommodation • Refraction Objective Visual Acuity Testing 20/400 20/200 20/100 20/50 20/25 Evaluation Techniques: Afferent System • Vision testing procedures Behavioral Vision Testing (acuity, color, stereo) Visual Evoked Responses (flash, pattern, sweep) Electroretinography (flash, pattern) Contrast, Color and Visual Field Testing Evaluation: Efferent System Eye Movement Recordings • Methods High speed photographic methods. “Contact” electrooculography. Infrared reflectance oculography. Scleral contact lens/magnetic search coils. Eye Movement Recordings • Diagnosis/Differentiation of Eye Movement Disorders. • Utility as an “Outcome Measure” in Clinical Research. R Deg L 10 Foveation Periods Within ±..5° by ±4°/sec Window 5 Deg 0 -5 0 1 2 Time (sec) 3 4 5 Eye Movement Recordings • Value of data Diagnosis. Classification. Etiology. Therapy. Research. Age Distribution 30% 25% 20% 15% 10% 5% 0% <2 <5 685 Patients 1998-2005 <10 <15 <20 Age (year) <30 >31 Afferent System Efferent System Conception Development Birth Infancy Vision Vergence, Versions STABLE OCULAR MOTOR SYSTEM CEMAS Disease Name INFANTILE NYSTAGMUS SYNDROME (INS) [Old Congenital Nystagmus and “Motor and Sensory” Nystagmus] Criteria Infantile onset, ocular motor recordings show diagnostic (accelerating) slow phases Common Associated Findings Conjugate, horizontal-torsional, increases with fixation attempt, progression from pendular to jerk, family history often positive, constant, conjugate, with or without associated sensory system deficits (e.g., albinism, achromatopsia), associated strabismus or refractive error, decreases with convergence, null and neutral zones present, associated head posture or head shaking, may exhibit a ”latent” component, “reversal” with OKN stimulus or (a)periodicity to the oscillation. Candidates on Chromosome X and 6 May decrease with induced convergence, increased fusion, extraocular muscle surgery, contact lenses and sedation. General Comments Waveforms may change in early infancy, head posture usually evident by 4 years of age. Vision prognosis dependent on integrity of sensory system. Nystagmus and Vision • “Sensory” System Refractive Error Amblyopia Abnormal Binocular Vision Ocular Media Damage Retinal Disease Nycloptia/Photophobia Optic Nerve Disease Visual Cortex Disease • “Motor” System Oscillation Strabismus Abnormal Pursuit (tracking) Abnormal Saccades (fast eye movements) “MOTOR” SYSTEM TREATMENT Medications Visual Training (strabismus, binocular dysfunction) Acupuncture Biofeedback Vibratory Stimulation Prisms, Telescopes, Contact Lenses Botox Eye Muscle Surgery Medical Treatments Spectacles Contact Lenses Low Vision Aids Penalization (patching, drops) Medical Treatments Photophobia Nystagmus • Sedatives, Hypnotics, Neuroleptics, Anti-seizure drugs • Acupuncture, Biofeedback, Vibratory Stimulation Strabismus and binocular dysfunction • Orthoptics • Spectacles • Penalization “Nystagmus” Surgery • Effect a Positive Change on the Oscillation Improve Waveform Increase Foveation Broaden Null Position Improve Periodicity • Treat Anomalous Head Positions ANIMAL MODEL OF INS • • • • • Achiasmatic Belgian Sheepdogs Ocular Motor Behavior Ocular Motor Analysis Infrared Oculography Recording Preoperative and Postoperative Visual Behavior Eye Movement Recordings HUMAN CLINICAL TRIALS EYE MUSCLE SURGERY AND INS • Simple tenotomy of all 4 horizontal recti • Reattachment at the original insertion • Final Effect related to underlying visual system disease Hertle RW, Dell’Osso LF, FitzGibbon, EJ, Yang D, Mellow SD. Horizontal Rectus Muscle Tenotomy In Children with Infantile Nystagmus Syndrome: A Pilot Study. Journal of AAPOS 2004:8;539-548 Hertle RW, Dell’Osso LF, FitzGibbon, EJ, Thompson DJS, Yang D, Mellow S. Horizontal Rectus Tenotomy In Patients with Congenital Nystagmus: Results In Ten Adults Ophthalmology 2003:11;2097-2115 HUMAN CLINICAL TRIALS EYE MUSCLE SURGERY AND INS • Increased Foveation (amount of time during a beat of INS during which the eye is moving at <4 deg/sec and within a few degrees of the target – when the eye/brain “sees”) Targe t Preferred OD Fixing Under Binocular Conditions Targe t HUMAN CLINICAL TRIALS EYE MUSCLE SURGERY AND INS • Improved Waveforms (Pure Jerk and Pendular to Jerk/Pendular with foveation) Target Preferred OD Fixing Under Binocular Conditions Target HUMAN CLINICAL TRIALS EYE MUSCLE SURGERY AND INS • Increased Breadth of The Null Zone R 10 degrees L 5 sec R 10 degrees 5 sec Pre-Operative L Post-Operative HUMAN CLINICAL TRIALS EYE MUSCLE SURGERY AND INS • 1-3 Lines of Recognition Acuity Increase LogMar Acuity Pre-Post Tenotomy Acuity 1 0.9 0.8 0.7 0.6 0.5 0.4 0.3 0.2 0.1 0 LogMar OU Pre LogMar OU Post 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 Patient # HUMAN CLINICAL TRIALS EYE MUSCLE SURGERY AND INS Improved Visual Recognition Time (Speed of Recognition) Lo gM AR 0.94 (20/176, S ize 7) 10 00 Latency (m sec) • 8 00 6 00 4 00 -40 -30 -20 -10 0 10 20 V e lo city (d egrees/s ec) 30 40 GAZE DEPENDENT VISUAL ACUITY 30 deg 20 deg Fig. 1.Gaze angle EFP 10 deg 0 deg 10 deg 20 deg 30 deg HUMAN CLINICAL TRIALS EYE MUSCLE SURGERY AND INS • Improved Gaze Dependent Visual Acuity (GDVA) 1 0.9 0.8 0.7 0.6 0.5 0.4 0.3 0.2 0.1 0 PREOP POSTOP -30 -20 -10 0 10 20 30 DEGREES OF GAZE PRE-POST GDVA PT. 25 LogMAR Acuity LogMAR Acuity PRE-POST GDVA PT. 19 1 0.9 0.8 0.7 0.6 0.5 0.4 0.3 0.2 0.1 0 PREOP POSTOP -30 -20 -10 0 10 DEGREES OF GAZE 20 30 Enthesial Area Annulus Of Zinn “Myotendon” CONTROL HUMAN ENTHESIS Myelin Nerve Ending Axon 2u Capillary 500u 2u TREATMENT:ANIMAL MODEL Etiologic INS with Gene Defect (RPE65 – Leber’s in Humans) Genetic Therapy* Conclusions Ask For: • Accurate Evaluation Afferent System Efferent System • Accurate Diagnosis Sensory System Deficits Nystagmus Type Strabismus Head Posturing • Medical Treatment Options • Surgical Treatment Options • Treatment versus “CURE”