inflammatory conditions of heart - Nursing PowerPoint Presentations
advertisement
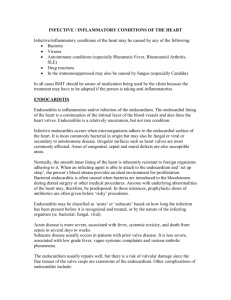
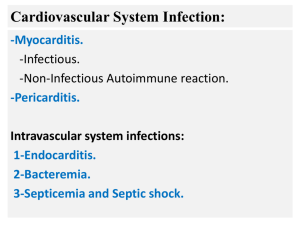
INFLAMMATORY CONDITIONS OF HEART LAYERS OF THE HEART MYOCARDITIS It is inflammation of heart muscle. CAUSES Commonest cause a virus. Other infections sarcoidosis, immune disease, pregnancy PATHOPHYSIOLOGY Virus invades the muscle local inflammation. After infection subsides, the body’s immune system continues to inflict inflammatory damage to the heart muscle. This immune response prolongs the myocarditis. MYOCARDITIS Sign & Symptoms Mild and cause no noticeable symptoms. Pain in the chest. Serious heart failure SOB, fatigue, fluid accumulation in the lungs & heart, rhythm irregularities inflammation or scarring. Diagnosis Detect signs of irritation of heart muscle. Blood tests (CPK) EKG, Nuclear heart scan shows. Treatment Corticosteroids. No proven medications Treatment -Salt restriction, ACE inhibitors, beta blockers treating as well as monitoring heart rhythm abnormalities. Prognosis After initial phase complete recovery of myocarditis Chronic Heart Failure due to injured heart muscle. Sudden unexpected, potentially fatal heart rhythm abnormalities. Prevented with implantable defibrillators - ENDOCARDITIS It is a serious infection of one of the four heart valves. Causes Growth of bacteria on one of the heart valves, leading to an infected mass called a vegetation. Infection may be bacteria in the blood stream after dental work, colonoscopy, and other similar procedures. Persons at Risk Heart valves (Aortic stenosis, Mitral stenosis, Mitral regurgitation etc) undergone valve replacements. etc). Endocarditis ENDOCARDITIS Sign & Symptoms Fever Fatigue Chills Weakness Aching joints and muscles Night sweats Edema of feet and abdomen Malaise Shortness of breath Occasionally scattered small skin lesions Diagnosis Echocardiography. TEE (Trans Esophageal Echocardiography) Identification of bacteria by blood culture. Treatment Antibiotics given intravenously for 4-6 weeks. Valve replacement Prognosis Response to treatment is indicated by a reduction in fever, negative blood cultures and findings on echocardiography. PERICARDITIS Heart sits in the centre of the chest and is surrounded by a sac called the pericardium. This sac has two layers one that fits tightly onto the heart muscle and another looser layer surrounding the inner layer. Inflammation of these tissue layers surrounding the heart is referred to as pericarditis. Etiology Idiopathic – cause of illness is not identified Mechanical injury to the heart Heart attack (MI) and Dressler’s syndrome Heart surgery and post pericardiotomy syndrome Trauma Infection Bacterial, viral, fungal, HIV Tumors/cancer Primary (rare) Metastatic Connective tissue disease Rheumatoid arthritis, SLE, Sarcoidosis, Scleroderma Metabolic disease Uremia, Hypothyroidism Medication reactions Side effects of: phenytoin, hydralizine and procainamide. Sign & Symptoms Chest pain SOB Fever, chills, muscle aches, malaise Diagnosis Physical evaluation Quality of pain, Physical finding – pericardial friction rub EKG Chest x-ray Ultrasound of the heart Blood testing for specific causes (Leukemia, kidney failure, connective tissue disease or thyroid abnormalities). Treatment Medicines that reduce inflammation NSAID’s to decrease inflammation and fluid accumulation in the pericardial sac. Narcotic pain medication for pain Corticosteroids for immunologically mediated causes. Pericardiocentesis /pericardotomy Complications Cardiac tamponade Constrictive pericarditis Nursing management Psychological support Assess heart sounds for new or worsening murmur. If pt received surgical treatment, provide postsurgical care. After surgery, monitor patient’s temperature; a fever may be present for weeks. Assess for signs and symptoms of organ damage such as stroke, CVA, meningitis, heart failure, MI etc. Instruct pt and family about activity restrictions, medications, and signs and symptoms of infection. Nursing management Reinforce that antibiotic prophylaxis is recommended for patients who have had infective endocarditis and who are undergoing invasive procedures. Refer to home care nurse to supervise and monitor intravenous antibiotic therapy in the home.