ANAESTHESIA FOR RENAL TRANSPLANTATION
advertisement
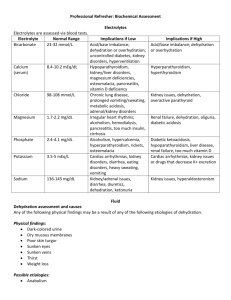
ANAESTHESIA FOR RENAL TRANSPLANTATION Dr.M.Kannan MD DA Professor and HOD of Anaesthesiology Tirunelveli Medical College Demand-supply imbalance 3000 300 per million 1800 per year in Tamilnadu Associated co-morbid conditions • Coronary artery disease • Congestive cardiac failure • Systemic Hypertension • Diabetes Mellitus Associated co-morbid conditions Coronary artery disease • Incidence 17%-34% • Coronary angiography & revascularisation • Irreversible LV dysfunction with very low cardiac output contraindication Associated co-morbid conditions Congestive cardiac failure • CCF is present before dialysis Independent prognostic Motality • CCF Associated with CRF IHD Hypoalbuminemia Old age Uremic cardiomyopathy Diabetes Anaemia AV-fistula Associated co-morbid conditions Systemic Hypertension • • • • • 70% of ESRD patients Discontinued before surgery ACE-inhibitors serum.K+ level monitored Calcium channel blockers Beta-blockers Continued peri-operatively Diuretics Laryngoscopy&Intubation • Exaggerated stress response • Opioids • beta-blockers • IV Lignocaine Associated co-morbid conditions Diabetes Mellitus Cardiac complications gets doubled Revised cardiac risk index • 1.High-risk surgical procedure. • 2.h/o IHD(excluding previous coronary revascularization) • 3.Heart failure • 4.h/o stroke or transient ischemic attacks • 5.Pre-operative insulin therapy • 6.Pre-operative creatinine levels higher than 2 mg/dl. Patho-physiological consequences of ESRD • Anaemia -Transfusion • Erythropoietin platelet function Uremic Coagulopathy Abnormal Normocytic normochromic Hyperkalemia Factor 8 anaemia Acidosis Uremic Cardiomyopathy Pre-operative dialysis Hypertension, Treatment-Dialysis Toxins Delays l- guanidinosuccinate,phen CVA, -Anaesthesia recovery Se.K+& acid-base status Phenolic Thrombosis ofacid fistulas • • • Delayed gastric emptying Sensitization of the recipient Pre-operative dialysis • Optimize fluid and electrolyte balance • Correct hemostatic abnormalities • Post dialysis weight loss of >2 kg -Indicate intra-vascular volume depletion -Thromboplastin time is checked for residual heparin -Hepatitis can be endemic Pre-operative optimazisation • Adequate BP control • Adequate control of blood glucose • Correction of se.K+ levels. • Correction of anaemia • Correction of coagulopathy Anaesthetic Agents • Thiopental • Propofol • Isoflurane -peripheral vaso-dilatation -minimal cardio-depressive effects -preservation of RBF -low renal toxicity Desflurane Sevoflurane • Fluoride • CompoundA • Fresh gas flow rates >4 L/min Opioids • Morphine • Pethedine • Reduced clearance • Accumulation of active metabolites • Fentanyl, sufentanil, • Safer alfentanil, • Metabolites are remifentanyl not potent, Muscle Relaxant -Succinyl choline ? -not contra-indicated in pts. with ESRD 0.6 m eq/l can be tolerated without significant cardiac risk Muscle Relaxant • Pancuronium • Less desirable in uremia. • Vecuronium • Slight in duration Elimination half lives of • Atracurium anti-cholinesterases • Hoffmann elimination are prolonged • Rocuronium • Clearance is unaffected in renal failure. Monitors • • • • • • 5-lead ECG. Arterial BP SpO2 EtCo2 Temperature . Urine output Special Monitors • CVP monitoring • Direct arterial pressure monitoring Sonicated albumin: • Pulmonary artery Hypotension >20/15 Systolic BP viability & Predict renal occlusion pressure 1.Poorlyvariation Hypovolemia controlled hypertension or LV dysfunction 2. CAD with • TEE Guide pharmacological correlates well with . Myocardial contractility 3 .Valvular heart disease interventions. • Contrast-EnhancedLV end-diastolic 4.COPD whenvolume severe. Perfusion USG Factors affecting kidney viability • • • Management of the kidney donor(living or cadaveric). How well the harvested organ is preserved. Peri-operative management of the kidney recipient. Anaesthetic considerations during donor nephrectomy • Venous return due to the kidney -adequate hydration • V/Q mismatching due to positioning • Mannitol and IV heparin (3000-5000) units before cross-clamping the renal vessels. • Administration of protamine to normalize coagulation Management of the Brain dead Kidney donor • Selection -Stable hemodynamics Adequate respiratory parameters Absolute contra-indications Prolonged hypotension Hypothermia Collagen vascular diseases Congenital or acquired metabolic disorders Malignancies, Generalized viral or bacterial infections DIC’ Hep B, HIV. Relative contra-indications • Age above 70 years • Diabetes mellitus • High serum creatinine before organ harvesting • Excessive pre-terminal use of vasopressors. Guidelines for intra-op management of the brain dead • • • • • A systolic BP >100 mm Hg PaO2 >100 mm Hg Urine output >100 ml/hr Hemoglobin concentration >100 g/l Central venous pressure between 5 and 10 mm Hg Guidelines for intra-op management of the brain dead • Vasodilators -Phentolamine • Hypotension- Fluid administration Pharmacological support • Bradycardia - Iso-prenaline (a direct acting chronotrope) and not atropine. Anaesthetic management of kidney recipients General Anaesthesia with controlled ventilation -Good hemodynamic stability -Better patient comfort. Regional Anaesthesia Dis-advantages: Systemic blood pressure -viability of the kidney donated. Large volumes of IVF precipitate acute LVF. Advantages It is cost-effective Complete abolition of stress response Less exposure to anaesthetic drugs Anaesthetic considerations in the recipient • Positioning – Care of the AV Fistula