CASE CONFERENCE
advertisement
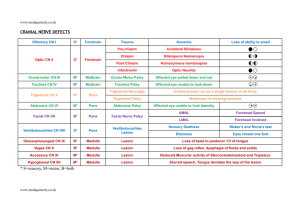
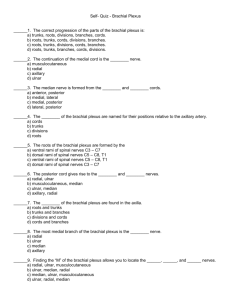
CASE CONFERENCE Suying Lam, MD PGY1 Presentation: FT male with L upper extremity weakness Born via NSVD Nuchal cord x 1 not tight Apgar: 9 at 1 minute; 9 at 5 minutes Physical Exam VS: T: F HR: x’ RR: x’ BP: UE: LE: Weight: 4kg Length: 53 cm Head circumference: 36 cm Chest circumference: 35 cm Abdominal circumference: 33.5 Physical Exam General: alert, NAD, macrosomic Skin: pink HEENT: AFOF, + molding, + swelling Patent nares, no cleft, no pits Thorax: symmetric expansion Lungs: clear, equal breath sounds Heart: RRR, no murmurs Abdomen: soft, NT, ND, BS+ Extremities: FROM R UE and both LE Reflexes: asymmetric moro reflex, sucking +, grasp + L UE: (+)abduction, (+)flexion but not against gravity. Position: adducted, internally rotated, elbow extended, forearm pronated, wrist and fingers flexed. Neonatal Brachial Plexus Palsies Smellie 1779 Duchenne and Erb 1870’s Klumpke 1885 Brachial Plexus Anatomy Risk Factors Large birth weight Average vertex: 3.8-5 Kg Average breech: 1.8-3.7 Kg Breech presentation Maternal diabetes Multiparity Second stage of labor that lasts more than 60 minutes Assisted delivery (mid/low forceps, vacuum extraction) Forceful downward traction on the head during delivery Previous child with OBPP Intrauterine torticollis Shoulder dystocia Causes Obstetric trauma: Clavicular fracture Humeral fracture Shoulder dislocation or subluxation Intrauterine compressive brachial plexus palsy Humeral osteomyelitis Neonatal Hemangiomatosis Exostosis of the first rib Neoplasm's (neuromas, rhabdoid tumors) Differential Diagnosis Pyramidal Tract Lesions Pre-brachial plexus lesions Cervical Spinal Cord Injury Amyoplasia Congenita (arthrogryposis) Pseudoparalysis secondary to pain (humeral fracture) Anterior horn cell injury (congenital varicella or congenital cervical spinal atrophy Diagnosis Laboratory: generally not necessary Imaging studies: Chest X-ray CT myelography High-resolution MRI Other tests: Electrodiagnostic studies (2-3 weeks after injury) Nerve conduction Studies Complete Brachial Plexus Palsy Duchenne-Erb Palsy C5-C6 Position: internally rotated, adducted, elbow extended, forearm is pronated, wrist is flexed and adducted, and fingers are flexed. Upper middle trunk brachial plexus palsy C5-C6-C7 Difference with Erb’s palsy: wrist is in neutral position (wrist flexor and extensors are equally weak) Klumpke Palsy C8-T1 Floppy hand: wrist is flexed, fingers extended following the forces of gravity Horner’s syndrome Fascicular brachial plexus palsy One muscle or a group of muscles in the arm Due to injury of a small group of motor fibers Management Rest period of 7 days pin the sleeve of neonate’s shirt to hold the elbow in a flexed position Physical Therapy Goals: minimizing bony deformities and joint contractures, while optimizing functional outcomes Passive and Active ROM exercise Bimanual activities Strengthening Promotion of sensory awareness Weight-bearing activities: propioceptive input + skeletal growth Static and dynamic splints Instructing parents and family: home exercise program Other treatments: Neuromuscular electrical stimulation Botulinum toxin A therapy Surgical Intervention Prognosis Degree of future improvement cannot be determined during a single evaluation, especially if performed immediately after birth. Improvement during the first few weeks is a relatively good indicator of final outcome. Incidence of permanent sequelae: 3-25% Findings consistent with severe initial injury (Horner’s syndrome) portend a less favorable prognosis Peripheral nerves re-myelinate at a rate of 1mm/day. If nerve is not transected, recovery can be expected by: 4-5 months in Erb’s palsy 6-7 months in upper-middle trunk palsy 14 months for a total BPP.