PRESERVE-THE-MIRACLE_Antibiotic-awareness-week
advertisement

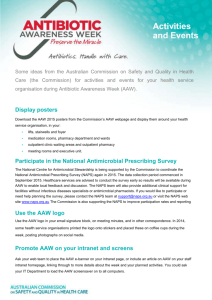
Preserving the Miracle of Antibiotics [Insert name of presenter] [Insert name of hospital] Overview • Antibiotic resistance – a critical patient safety and public health issue – the problem with resistant organisms – the link to antibiotic use • Appropriate use of antibiotics in our hospital – Antimicrobial Stewardship • Antibiotic Awareness Week 2012 – Preserving the miracle – use antibiotics appropriately Importance of antibiotics • Most significant impact on life expectancy in last 100 years (arguably) – ability to prevent and treat infection • Major factors: public health (sanitation), vaccination, antibiotics Crude mortality rates for all causes, noninfectious causes and infectious diseases over the period 1900-1996. 1. Armstrong GL et al, JAMA 1999;281(1):61-66 Antibiotics and other medical advances • Other advances rely on ability to control infection – – – – – – – Transplantation Neonatal care Chemotherapy for malignancy Immunosuppression Safe surgery Safe obstetric care Intensive care interventions Emergence of antibiotic resistance Antibiotic resistance threatens ability to control infection 2. Pray LA Insight Pharma Reports 2008, in Looke D ‘The Real Threat of Antibiotic Resistance’ 2012 Resistance spreads rapidly 3. Centers for Disease Control and Prevention http://www.cdc.gov/hai/ Antibiotic resistance in 2012 • Worldwide problems with resistant pathogens including MRSA, VRE, Gram negative organisms, HIV, TB and malaria4,5 • These problems affect us here in Australia too • Last line antibiotics (carbapenems, fluoroquinolones, 3rd-gen cephalosporins) may no longer be effective against some common bacteria e.g. multiresistant E. coli infections causing cystitis5 4. World Health Organization The evolving threat of antimicrobial resistance: Options for action 2012 5. Gottlieb T, Nimmo GR MJA 2011; 194(6): 281-283 Resistance in our region • Gram negatives (E. coli, Klebsiella spp.) – common infections e.g. UTI in community – high rates resistance in our region • ESBL-producing organisms = resistant to cephalosporins 6. Hawser SP et al. AAC 2009; 53(8):3280-3284 Antibiotic resistance locally • • • • Which infections are we seeing ? Insert hospital data Numbers of cases Example cases Real people are affected 7. IDSA ‘Patient stories’ 2012 http://www.idsociety.org/Patient_Stories/ Impact of resistance • Increased morbidity/ mortality – Evidence across many pathogens • Untreatable infections – Now being encountered • Increased costs – $18-29,000 US/ patient8 Antibiotic misuse drives antibiotic resistance 8. Roberts RR et al. Clinical Infectious Diseases 2009; 49:1175-1184 High consumption is associated with increased resistance Countries with high penicillin consumption also have high rates of penicillin resistance in pneumococci Occurrence of penicillinnonsusceptible Streptococcus pneumoniae (PNSP) versus outpatient use of penicillins in 17 European countries. 9. van de Sande-Bruinsma N et al. Emerging Infectious Diseases 2008; 14(11):1722-1730 Consumption varies widely between countries Note: graph represents per capita consumption 10. Goossens et al .Clin Infect Dis 2007; 44(8):1091-1095 Consumption varies between hospitals Even within a country – huge inter-hospital variation in antibiotic consumption e.g. meropenem use - 10-fold variation across 37 Australian hospitals meropenem doripenem ertapenem imipenem with cilastatin median Antimicrobial usage rate (DDD per 1000 OBDs) 70 60 National Antimicrobial Utilisation Surveillance Program (NAUSP) 2011-12 annual report11 50 40 30 20 10 0 P6 F3 A9 J8 W5 V5 G8 R9 G2 R3 O3 O2 I7 Z9 O7 D8 U2 M6 H7 F8 L6 L8 T3 L5 T4 D5 G5 B2 U6 U7 K0 R2 D6 O4 O5 L7 Z6 Hospital contributor code 11. South Australian Infection Control Service. National Antimicrobial Utilisation Surveillance Program (NAUSP) 2011-12 Annual Report. Antibiotic usage in our hospital • Insert local usage data if available Antibiotics are a limited resource • Few new antibiotics being developed • Most classes developed pre 1970 • Only 3 novel systemic classes in last 20 years • Growing recognition globally that: – new antibiotics are urgently required – we need to conserve what we have In summary.... • We have a problem ! – Growing rates of resistance – Inappropriate use – Decreasing pipeline of new antibiotics 12. Turnidge J et al. MJA 2009: 191(7): 368-373 What can we do? Preserve the miracle of antibiotics by appropriate use. 13. Carlet J et al. Lancet 2011: 378(9788): 369-371 What is inappropriate antibiotic use? • Prescribing unnecessarily – e.g. for viral infections, prolonged prophylaxis • Using broad spectrum agents when narrow spectrum agents are more appropriate. • Dose too high or too low • Duration of treatment too long • Not prescribing according to micro results • Timing - omitting or delaying dose “Appropriate use”? • Prescribe according to current endorsed • • • • • Therapeutic Guidelines: Antibiotic Check microbiology results Review empiric antibiotic therapy at 48-72 hours Seek infectious diseases/microbiology advice early for complex cases (insert process for ID consult here) Use pharmacy expertise for dosing advice (insert local processes here) Use the MINDME Creed 14. Therapeutic guidelines: antibiotic. Version 14. 2010 Antimicrobial stewardship (AMS) • Part of broader system for infection prevention and control to minimise resistance • Aim is to optimise use of antibiotics taking into account: – Evidence of efficacy – Toxicity – Ecologic harm (effect on resistance) • Requires team work at all levels: – Executive and clinical leadership – Prescribers, clinicians, pharmacists Essential elements: treatment guidelines, formulary with restrictions, selective susceptibility reporting of isolates, effective audit and feedback to prescribers National Safety & Quality Health Service Standards Standard 3: Antimicrobial Stewardship Criterion Actions required: 3.14.1 An antimicrobial stewardship program is in place 3.14.2 The clinical workforce prescribing antimicrobials have access to endorsed Therapeutic Guidelines on antibiotic usage 3.14.3 Monitoring of antimicrobial usage and resistance is undertaken 3.14.4 Action is taken to improve the effectiveness of antimicrobial stewardship 15. ACSQHC National Safety & Quality Health Service Standards www.safetyandquality.gov.au/our-work/accreditation/nsqhss/ Antibiotic Awareness Week 2012 Preserve the miracle • Antibiotic Awareness Week, 12-18 November, 2012 – A nationally coordinated campaign to promote appropriate antibiotic use, supported by: • • • • • The Australian Commission on Safety and Quality in Health Care NPS MedicineWise Australasian College for Infection Prevention and Control Australasian Society for Infectious Diseases Australian Society for Antimicrobials • An international effort: UK and Europe, USA, Canada Antibiotic Awareness Week activities • National resources – For hospitals: Australian Commission on Safety and Quality in Health Care – For consumers and primary care, health professionals: NPSMedicineWise • 127 Australian hospitals participating in national antibiotic survey • Social media events (Facebook, Twitter) • Media releases (ACSQHC, NPS MedicineWise) • Events in hospitals all over Australia • Insert local hospital activities? Hospital resources • Australian Commission on Safety and Quality in Health Care – ‘Antimicrobial Stewardship in Australian Hospitals’ – Downloadable tools and resources (example policies, guidelines, templates, packet cards etc) – Link to antimicrobial prescribing elearning modules – Links to international websites – Presentations http://www.safetyandquality.gov.au/our-work/healthcareassociated-infection/antimicrobial-stewardship/ Resources for Consumers and Health Professionals • NPS MedicineWise – Resources for consumers, health professionals – Facebook, Twitter conversations planned for the week – Antimicrobial prescribing e-learning modules www.nps.org.au Our Hospital tools and activities to promote appropriate use of antibiotics • AMS committee (or other committee e.g. infection control, drug & therapeutics committees) to coordinate activity • Education – prescribing guidelines • Policy – Formulary with restrictions and approval • Access to expert prescribing advice – ID, Micro, Pharmacy • Audits and feedback • Prescribing survey? • Who to contact? Key Messages • Resistance is a critical public health and patient safety issue • Resistant infections are harder to treat and are associated with higher rates of morbidity and mortality • Inappropriate antibiotic use is a major driver of resistance • Antibiotics are a limited and precious resource • Up to 50% of antimicrobial prescribing in hospitals is inappropriate • Antimicrobial Stewardship Programs and appropriate use of antibiotics can contribute to reducing resistance and make a difference to patient safety and quality of care Want to know more ? Australia • Australian Commission on Safety and Quality in Health Care (ACSQHC) www.safetyandquality.gov.au • NPS MedicineWise www.nps.org.au • State & territory health departments International • European Antibiotic Awareness Day ttp://ecdc.europa.eu/en/eaad/Pages/Home.aspx • Canadian Antibiotic Awareness Week http://antibioticawareness.ca/ • United States Get Smart About Antibiotics Week http://www.cdc.gov/GetSmart/campaignmaterials/week/index.html Acknowledgements and References • Australian Commission on Safety and Quality in Health Care – AMS Jurisdictional Network – Antibiotic Awareness Week working group members • Australian Group on Antimicrobial Resistance • National Antimicrobial Utilisation Surveillance Program • Melbourne Health – NHMRC Antimicrobial Stewardship partnership grant team • European Centre for Disease Prevention and Control References: The presentation in it’s original version along with a complete list of references can be downloaded from the Commission web page: http://www.safetyandquality.gov.au/our-work/healthcare-associatedinfection/antimicrobial-stewardship/antibiotic-awareness-week-2012