Rapid Recovery in Total Joint Replacement- A Rural
advertisement
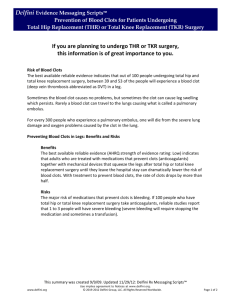
Rapid Recovery in Total Joint ReplacementA Rural Hospital Experience Adam English, RN, DNP-S Minnesota Center for Orthopaedics Cuyuna Regional Medical Center, Crosby, MN aenglish@cuyunamed.org Disclosure No financial disclosures to report. Objectives • Identify current trends in total joint replacement. • Describe the rapid recovery protocol for total joint replacement. • Explain the difference in patient outcomes between standard recovery and rapid recovery protocols. Trends in Total Joint Replacement • Projected increases by 2030: – THA- will increase by 174% – Hip revision- will increase by 137% – TKA- will increase by 673% (3.48 million) – Knee revision- will increase by 601% • Knee revisions will double by 2015 Trends-Cost • Half of patients receiving total joint replacement are under 65, and still in workforce1. • Job-related knee pain cost $3.4-$13.2 billion in lost wages for patients1. • After a surgery, societal savings averaged between $10,000 and $30,000/joint from increased earnings and a decrease in fewer work days and disability payments1. J Bone Joint Surg Am. 2013. Critical Access Hospitals (CAH) • No more than 25 inpatient beds. • Average length of stay no more than 96 hours. • Must offer 24/7 emergency access. • Must be in a rural area. • Allows CAH to receive cost-based reimbursement from Medicare instead of standard fixed rates. Cuyuna Regional Medical Center (CRMC) • Critical-access hospital located in north-central, rural MN. • Currently employs over 1000 people in a town of 1300. • Total joint replacement increased by 25% last year. • Over $2 million in surgical cases diverted away in 2012 because of no hospital bed available. Total Joint Replacement-Standard • General anesthesia with femoral nerve block for postoperative pain. • Physical therapy initiated on post-op day 2. • Average hospital stay: 3-5 days. CRMC-Rapid Recovery Protocol • Multimodal analgesia before, during, and after surgery. • Treat and eliminate potential complications (blood loss, nausea, urinary retention). • Use less narcotic pain medication throughout inpatient stay. • Get patient up and walking the day they have surgery. Preoperative Care • Medications (Pain): • Medications (Nausea): – Lyrica 150mg – ASA 325mg – Oxycontin 10mg – Scopolamine Patch behind ear. Potentially Flomax 0.4mg at HS based on AUA BPH scale (started 7-10 days preoperatively). Intra-operative Care • Anesthesia: General • Transexemic Acid: 1 gram IV before incision and 1 gram IV at closure. • Acetaminophen 1000mg IV: Q8 hours x 3 doses (started after implants in). • Toradol: 15mg IV Q6 hours x 4 doses (started at end of operation). Postoperative Care • Continue the scheduled non-narcotic pain medications (Acetaminophen and Toradol). • Narcotic Stratification: different pain meds based on level of patient pain. • DVT Prophylaxis: ASA 325mg PO BID x 4 weeks unless previously on warfarin. Orthopaedic Joint Coordinator • 24/7 total joint hotline that patients are instructed to call if any issues (before ER). • Handles all preoperative education, hospital rounds, and discharge instructions. • 100% clinic-based to be there to answer questions/concerns. • “Open-door” policy where total joint patients can come to the clinic to check incision/reassure patients. CRMC Rapid Recovery Outcomes • Knee Replacement data published in American Academy of Orthopaedic Surgeons (AAOS) (presentation at national conference in 2015). • Hip Replacement data published in American Academy of Hip and Knee Surgeons (AAHKS) with poster presentation at conference. Methods • Last 100 total joints using standard protocol compared to first 100 total joints using rapid recovery. • All surgeries performed by a fellowship-trained orthopaedic surgeon using the same approach for all patients. • Measured length of stay, pain levels, narcotic usage, need for skilled nursing facilities, readmissions, complications. • No patients excluded from data set. Patient Demographics Patient Characteristics Pre-Rapid Recovery Post-Rapid Recovery p value Gender (% Male-Female) 50.0-50.0 54.0-46.0 0.693 Mean Age (Years) 69.24 67.14 0.247 Mean ASA Classification 2.56 2.5 0.552 Mean BMI 35.75 34.57 0.421 No significant difference in gender, age, ASA, BMI Total Hip Replacement • Patients in rapid recovery protocol had a mean discharge day of 1.5 compared to 2.75 days in the pre-rapid recovery group (p<0.0001). • Pain scores were significantly better in the rapid recovery group with a postoperative day one average of 2.8/10 compared t0 4.1/10 before (p=0.002). 3 5 2.5 4 2 Before Rapid Recovery 1.5 1 After Rapid Recovery 0.5 Before Rapid Recovery 3 After Rapid Recovery 2 1 0 0 Length of Hospital Stay(Days) (p<0.0001) Postoperative Day #1 Pain (out of 10) (p=0.002) Total Hip Replacement • Skilled Nursing Facilities (SNF): In the pre-rapid recovery dataset, 34% of patients required a SNF stay. In the post-rapid recovery dataset, only 7% were sent to SNF. SNF (%) 35 30 25 20 SNF (%) 15 10 5 0 Pre-Rapid Recovery Post-Rapid Recovery • Readmissions: In the pre-rapid recovery dataset, there 1 readmission (constipation) within the first 30 days postoperatively. This compares to 1 re-admission (wound dehiscence) in the postrapid recovery dataset. Total Knee Replacement • Patients in the rapid recovery group had a mean discharge day of 1.7 compared to 3.2 days in the pre-rapid recovery group (p<0.001). • Patients in the rapid recovery group had mean pain scores that were significantly better in the rapid recovery group (3.2/10) compared to the pre-rapid recovery group (4.8/10). Total Knee Replacement • Narcotic consumption was significantly less (11.21mg) in the rapid recovery group than in the pre-rapid recovery group(21.76mg). • In the pre-rapid recovery group, 34% of patients discharged to skilled nursing facilities compared to 7% in the rapid recovery group. SNF (%) 35 30 25 20 SNF (%) 15 10 5 0 Pre-Rapid Recovery Post-Rapid Recovery Discussion • Data demonstrates the positive impact and advantages of an easily translatable rapid recovery protocol using non-narcotic medicines. • Patients are able to discharge on Day 1, pain scores are markedly better, and the overall health care costs are diminished, due to shorter length of hospitalization and less need for skilled nursing facilities. Discussion • Forecast is for dramatic increase in patient volume. • Health care reform is going to place more emphasis on outcomes and value. • Facilities must prepare for increase in volume and prove their outcomes. References 1. 2. 3. 4. 5. Ruiz, D., Koenig, L., Dall, T., Gallo, P., Narzikul, A., Parvizi, J., Tongue, J. (2013). The direct and indirect costs to society of treatment for end-stage knee osteoarthritis. The Journal of Bone and Joint Surgery. 95:1473-80. Tayrose G, Newman D, Slover J, Jaffe F, Hunter T, Bosco III J. Rapid Mobilization Decreases Length of Stay in Joint Replacement Patients. Bulletin of the Hospital for Joint Disease. January 2013; 71(3):222-226. Malviya A, Martin K, Harper I, Muller S, Emmerson K, Parlington P, Reed M. Enhanced Recovery Program for Hip and Knee Replacement Reduces Death Rate. Acta Othopaedica. October 2011;82(5):577-581. Lombardi A, Berend K, Adams J. A Rapid Recovery Program: Early Home and Pain Free. Orthopaedics. September 2010;33(9):656. Doman D, Gerlinger T. Total Joint Arthroplasty Cost Savings with a Rapid Recovery Protocol in a Military Medical Center. Military Medicine. January 2012; 177 (1):64-69.