History of Artificial Joints
advertisement
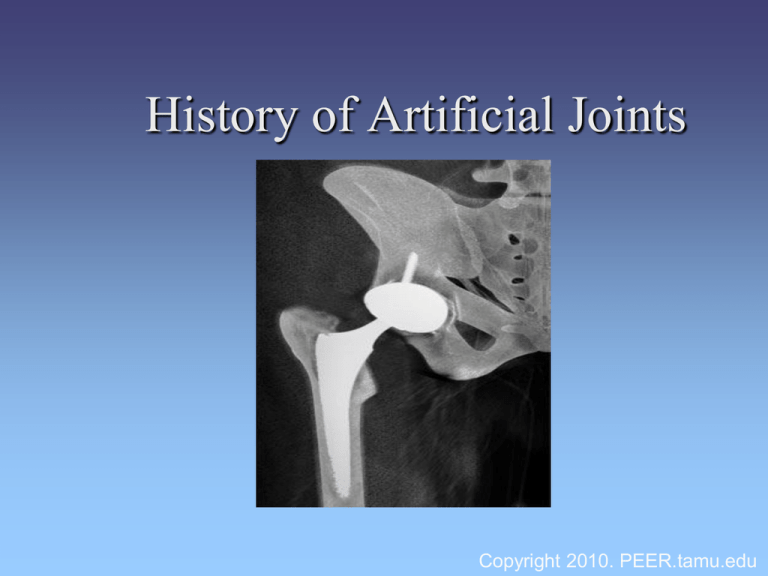
History of Artificial Joints Copyright 2010. PEER.tamu.edu Question: • Do you know anyone that has ever had a joint replacement surgery? • Many people are now benefitting from joint replacement surgery. • Pets also benefit from joint replacement surgery! Hip Replacement • The hip joint is the largest load bearing joint. A hip joint is lined with a layer of cartilage that reduces friction and acts as a shock absorber. • When the bone is exposed to arthritis and injury, this protective layer is damaged, causing extreme pain. • What are some things that could cause injury to your hip? Hip Replacement • The search to alleviate pain led surgeons over a century ago to research the possibility of hip replacements. Early Hip Arthritis Surgery in the 1800s • In 1821, Anthony White of the Westminster Hospital in London, performed the first anthroplasty, where an arthritic or joint surface is replaced. The procedure helped with pain and mobility, but failed with stability. Early Hip Arthritis Surgery in the 1800s • In 1826, John Rhea Bartonii performed the first osteomy, where a bone is cut to shorten, lengthen, or change its alignment. Unfortunately, this procedure had unpredictable results. • Early solutions also included removing calcium deposits and damaged cartilage. Leading the Way In 1891, Professor Themistocles Glück led the way in his development of a hip implant fixation. He produced an ivory ball and socket joint that he fixed to bone with nickel plated screws. He also used a mixture of plaster of Paris, and powdered pumice with resin for fixation. Glück Introduces New Ideas to Studies • Glück‘s studies on hip replacements led to greater advancements that were implemented on other joints, including knee joints. • He was also one of the first to propose implementing joints from corpses and amputated limbs . He proposed the idea by demonstrating in animal experiments that the cavity in the bone for the bone marrow would accept the shaft of the artificial joint if it is stably anchored within it. Glück Introduces New Ideas to Studies • Glück was also a pioneer in proposing the idea of biocompatibility, which explains how a foreign material placed in the body must be well tolerated by the patient’s body. Think Break: • What were some of the problems with early efforts at joint replacement? • What were some of the materials used in early joint replacement surgeries? Greater Advances • In 1925, a surgeon in Boston, Massachusetts, M.N. Smith-Petersen, M.D., molded a piece of glass into the shape of a hollow hemisphere which could fit over the ball of the hip joint and provide a new smooth surface for movement. While proving biocompatibility, the glass could not withstand the stress of walking and quickly failed. Greater Advances • One concern in prosthetics is using a material that is biocompatible and will not cause adverse effects once implanted, an idea Glück had introduced earlier. • M.N. Smith-Peterson continued his studies and pursued other materials including plastic and stainless steel. Cobalt-Chromium Alloy • A dramatic improvement was made in 1936 when scientists manufactured a cobalt-chromium alloy. This new alloy was both very strong and resistant to corrosion, and is still being used today. • While this new metal proved to be a great success, the actual resurfacing technique was not adequate. What is Hip Resurfacing? Hip resurfacing involves removing the cartilage from the surface of the femoral head and replacing it with a metal cap. This may save the hip joint for 20 to 30 years. Finding a solution… • In 1938, Dr. Jean Judet and his brother, Dr. Robert Judet, of Paris, attempted to use an acrylic material to replace arthritic hip surfaces. Unfortunately, this material fell short of expectations and tended to fall loose. Judet acrylic prosthetic design By this time it became clear that artificial joint material had to be biocompatible and withstand the stresses of the body. Continuing Research • In the 1950s, Frederick R. Thompson and Austin T. Moore separately developed replacements for the entire ball of the hip. Continuing Research • Their type of hip replacement replaced the arthritic femoral head (ball), but failed to replace the acetabulum (hip socket). • The prosthesis consisted of a metal stem which was placed into the marrow cavity of the femur, connected in one piece with a metal ball which fit into the hip socket. The Birth of “Total Hip Replacement” • In 1958, John Charnley from England introduced the idea of replacing the eroded arthritic socket with a Teflon component. When this failed he used a polyethylene polymer to construct the socket. Charnley replaced Teflon with polyethylene The Birth of “Total Hip Replacement” • To obtain fixation of the polyethylene socket as well as the femoral implant to the bone, polymethylmethacrylate was used as a bone cement. • By 1961, Charnley was performing surgery regularly with great results. Animal Studies • J. Charnley did not come across his innovations by pure luck. He became highly interested in animal studies and applied these findings to the design of hip replacement. • In particular, Charnley did research in the lubrication of animal joints after a patient with a Judet replacement produced a squeak when he moved his hip. Animal Studies • He studied the work of biologists who studied lubrication of animal joints. This helped Charnley explain why synovial (joint) fluid served as a lubricant for articular (joint) cartilage, but not for metal on bare bone, nor a lubricant for metal on metal. Hip Dysplasia in Dogs Normal Hip Abnormal Hip The left image is a normal hip. The femur is smooth and round. The ball fits nicely into the socket (acetabulum). The right image is a abnormal hip. We can see a shallow socket and a short neck attaching the ball to the shaft of the femur. Hip Dysplasia Treatment Total hip replacement in canines results in the most normal limb function in large dogs. The objective of this procedure is to replace the cartilage of the acetabulum “socket” with a polyethylene socket, and the femoral head with a metal prosthesis. Stop and Think: • What are some good reasons why researchers use animals as subjects in their investigations? Knee Replacement • The healthy knee joint is lined with cartilage. Arthritis and injury can cause damage to this protective layer. The damage of knee joints by arthritis led to research and development of knee replacements. Knee Replacements The study of hip replacements led to ways to treat knee joints. • Some of the early work began by implanting metal spacers between the bones of the knee. In the 1950s, McKeever and McIntosh attempted this procedure but results were unpredictable. The Beginning of Knee Replacements During the late 1960's, a Canadian orthopedist, Frank Gunston, from Sir John Charnley's Hip Center, developed a metal-on-plastic knee replacement to be secured to the bone with cement. This was really the first metal and plastic knee and the first with cement fixation. Continued Advancements • In 1972, John Insall, M.D., designed what has become the prototype for current total knee replacements. The prosthesis was made of three components for resurfacing all three surfaces of the knee -the femur, tibia and patella (kneecap). Each were fixed with bone cement and the results were outstanding. Leading Vendors • Moore’s 1952 model was produced in collaboration with Howmedica Inc., at the time Austenal Laboratories, now merged with Stryker®. • Stryker® is one of the leading medical device companies today. • Encore medical is also one of the leading medical device companies that led the way in prosthetic hip and knee replacements. Stryker Products Hip Replacement Systems Primary Acetabular Components Primary Femoral Components 3-D Knee Knee Replacement Joint Replacement Today Joint replacements have come a long way since their beginning. Every year, more than 600,000 people in the U.S. undergo hip- or knee-replacement surgery, according to Consumer Reports. New advancements in hip replacement include minimally invasive surgery that spares muscle, offering patients a faster recovery. The Future???? • What can you imagine for the future of Joint Replacement?