T-Cell Lymphoma SUV max
advertisement

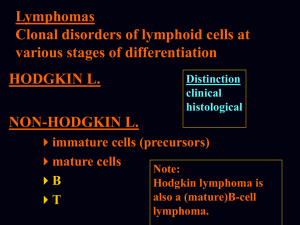
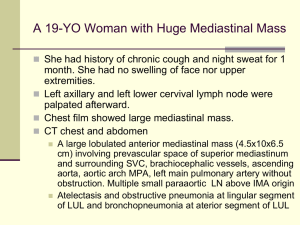
CME-Certified 2012 Hematology Tumor Board Series: Practical Solutions to Current Clinical Challenges in T-Cell Lymphoma Moderator James O. Armitage, MD Joe Shapiro Distinguished Chair of Oncology Professor of Internal Medicine Division of Hematology/Oncology Department of Internal Medicine University of Nebraska Medical Center Omaha, Nebraska Panelists Julie M. Vose, MD, MBA Bertrand Coiffier, MD, PhD Neumann M. and Mildred E. Harris Professorial Chair Chief and Professor of Internal Medicine Division of Hematology/Oncology Department of Internal Medicine University of Nebraska Medical Center Omaha, Nebraska Professor of Hematology Head, Department of Hematology Hospices Civils de Lyon Université Claude Bernard Lyon, France Owen O’Connor, MD, PhD Professor of Medicine and Developmental Therapeutics Columbia University College of Physicians and Surgeons Director of the Center for Lymphoid Malignancies New York-Presbyterian Hospital Columbia University Medical Center New York, New York Program Goals • Identify prognostic and clinical factors that should be considered in selecting treatment for patients with T-cell lymphoma. • Consider patient- and disease-specific factors when selecting frontline and relapse/refractory treatment options for patients with T-cell lymphoma. • Assess how emerging therapies or regimens for patients with T-cell lymphoma may impact current treatment practices. T-Cell Lymphoma Overview • Relatively rare − ~10% of lymphomas in the United States • PTCL − Arises from mature T-cell counterparts − Geographic variation in distribution − Has 3 major aggressive subtypes • PTCL-NOS (25.9%) • AITL (18.5%) • ALCL (ALK+[6.6%], ALK−[5.5%]) AITL = angioimmunoblastic T-cell lymphoma; ALCL = anaplastic large cell lymphoma; ALK = anaplastic lymphoma kinase; NOS = not otherwise specified; PTCL = peripheral T-cell lymphoma. Vose J, et al. J Clin Oncol. 2008;26:4124-4130. T-Cell Lymphoma Overview • Relatively rare − ~10% of lymphomas in the United States • PTCL − Arises from mature T-cell counterparts − Geographic variation in distribution − Has 3 major aggressive subtypes • PTCL-NOS (25.9%) • AITL (18.5%) • ALCL (ALK+[6.6%], ALK−[5.5%]) AITL = angioimmunoblastic T-cell lymphoma; ALCL = anaplastic large cell lymphoma; ALK = anaplastic lymphoma kinase; NOS = not otherwise specified; PTCL = peripheral T-cell lymphoma. Vose J, et al. J Clin Oncol. 2008;26:4124-4130. PTCL-NOS Clinicopathologic Features • Clinically aggressive, typically occurs in adults aged 50 to 70 years − Usual patient presentation: high-stage disease, generalized lymphadenopathy, B symptoms, and peripheral blood eosinophilia • Highly variable pathology − Most likely represents more than 1 subtype • Broad differential diagnosis due to the heterogeneous appearance − Other lymphoma subtypes − Reactive hyperplasias due to viral or drug reaction AITL Clinicopathologic Features • Clinically aggressive, typically occurs in middle-aged or elderly adults − Dismal outcome with current therapies − Usual patient presentation: generalized lymphadenopathy, fever, weight loss, skin rashes, arthritis, polyclonal hypergammaglobulinemia, and hemolytic anemia • Displays a characteristic arborizing vascular pattern • Coexisting immune dysfunction may complicate diagnosis. • Differential diagnosis − Other lymphoma subtypes − Atypical immune reaction − Hyperplasia (viral or idiopathic) ALCL Clinicopathologic Features • Clinically aggressive with biphasic age distribution − Younger patients, generally ALK+ • Associated with improved survival compared with other PTCL subtypes − Older patients, more likely ALK− • Not challenging to identify − CD30 strongly expressed in all cases − t(2;5)(p23;q25), prototypical translocation in ALK+ subtype • Abnormal ALK-NPM fusion protein overexpressed Case 1 PTCL-NOS Case 1 Presentation, Biopsy, PET/CT Scan • A 50-year-old man presented with fatigue and lymphadenopathy. • Biopsy showed PTCL-NOS. • Patient underwent PET/CT scanning, which showed − Nodes in the axilla, periaortic region, and iliac region; and − An SUVmax of 9. SUVmax = maximum standardized uptake value. Case 1 Additional Findings • His spleen was slightly enlarged with no focal lesions. • Results of a CBC were normal, except for his platelet count, which was 135,000/mm3. • Results of a bone marrow biopsy were negative. • Remaining results from the diagnostic work-up were negative. Case 1 How Would You Approach This Patient? T-Cell Lymphoma SUVmax Nodal 18 16 14 12 10 8 6 4 2 0 SUVmax SUVmax Extra-nodal *† T-Cell Indolent B-NHL Aggressive B-NHL 18 16 14 12 10 8 6 4 2 0 * T-Cell Indolent B-NHL B-NHL = B-cell non-Hodgkin lymphoma; SUVmax = maximum standardized uptake value. Storto G, et al. Br J Haematol. 2010;151:195-197. Case 1 Initial Treatment Considerations • As a relatively young and fit patient, he should be given aggressive therapy. − Consider an etoposide-containing regimen. • Consider ASCT as consolidation after induction therapy. • Always try to enroll a patient in clinical trial, if possible. CHOP not effective PTCL DSHNHL Experience EFS of Younger Patients (Aged 18-60 y; LDH Level < UNV) 100 Percentage of Patients 90 80 Etoposide (n = 103) 70 60 50 40 Non-etoposide (n = 41) 30 20 P = .004 10 0 0 10 20 30 40 50 60 70 80 90 100 110 Months EFS = event-free survival; LDH = lactate dehydrogenase; UNV = upper normal value. Schmitz N, et al. Blood. 2010;116:3418-3425. PTCL Up-Front ASCT IMAGE NO LONGER AVAILABLE ASCT = autologous stem cell transplant; OS = overall survival; PFS = progress-free survival. d’Amore F, et al. J Clin Oncol. 2012;30.3093-3099. Role of PET as Interim Prognostic Factor Remains to be Clarified! PTCL-NOS European Perspective PTCL-NOS Anthracycline-Based Chemotherapy AbouYabis AN, et al. ISRN Hematol. 2011;2011:623924. PTCL Survival Based on IPI Score IPI = International Prognostic Index. Sonnen R, et al. Br J Haematol. 2005;129:366-3672. PTCL-NOS Novel Treatment Approaches Case 2 ALCL Case 2 Presentation, Biopsy, PET/CT Scan • A 41-year-old man presented with fever 38.5oC) and malaise and was found to have a palpable right axillary node. • A biopsy of the axillary node showed ALCL, CD30+ and ALK−. • Results of a bone marrow biopsy were negative. • He underwent PET/CT scanning, which showed PET-avid enlarged nodes in the chest and abdomen. Case 2 How Would You Approach This Patient? Case 2 Initial Treatment Considerations • Given that it is stage III disease, ALCL, ALK−, it should be approached as if it were PTCL-NOS rather than ALCL, ALK+. • He is young and may tolerate the highdose combination very well. − Treatment options include ACVBP* with supportive G-CSF, CHOEP, or EPOCH. • If he reaches CR → ASCT. * Regimen not available in the United States. Aggressive Lymphoma ACVBP vs CHOP or HDT/ASCT IMAGE NO LONGER AVAILABLE HDT = high-dose chemotherapy. Tilly H, et al. Blood. 2003;102:3418-3425. Gisselbrecht C, et al. J Clin Oncol. 2002;20:2472-2479. International T-Cell Lymphoma Project Subtypes and Clinical Outcomes IMAGE NO LONGER AVAILABLE Vose J, et al. J Clin Oncol. 2008;26:4124-4130. Relapsed or Refractory ALCL Targeting CD30 With Ab-Drug Conjugate IMAGE NO LONGER AVAILABLE Pro B, et al. J Clin Oncol. 2012;30:2190-2196. What if Patient Had ALCL, ALK+ Disease? Use Standard CHOP-Based Chemotherapy. Targeting ALK Crizotinib Novel Agents Pralatrexate Case 3 AITL Case 3 Presentation, Biopsy, PET/CT Scan • A 70-year-old women presented with a macular rash, pruritus, drenching night sweats, 10-lb weight loss, and widespread lymphadenopathy. • Biopsy results showed AITL. • Results of a bone marrow biopsy were positive. • A CBC found anemia (Hb 10 g/dL), and the Coombs was negative. • PET/CT scanning revealed widespread enlarged nodes above and below the diaphragm. CBC = complete blood count; Hb = hemoglobin. Case 3 How Would You Approach This Patient? Relapsed and Refractory PTCL PROPEL Trial Subtype IWC Response Rates, % CI, 95% PTCL-NOS (n = 59) 32 21-46 AITL (n = 13) 8 0-36 ALCL (n = 17) 35 14-62 IWC = International Workshop Criteria. O’Connor O, et al. J Clin Oncol. 2011;29:1182-1189. Relapsed and Refractory PTCL Phase 2 Study of Romidepsin Subtype CR/CRu, % ORR, % PTCL-NOS (n = 69) 14 29 AITL (n = 27) 19 30 ALCL, ALK− (n = 21) 19 24 CRu = complete remission unconfirmed. Coiffier B, et al. J Clin Oncol. 2012;30:631-636. Case 3 Initial Treatment Considerations • Patients like this—older and not very well—often respond early on to steroids. − Start with a steroid-containing combination to try to get her symptoms under control and improve her performance status. • Avoid anthracycline-based therapy. • Single-agent gemcitabine may help manage disease without excess myelosuppression. • Look for the possible presence of an associated B-cell clone; if found, use a rituximab combination. • This is one of the more difficult patient types. • If possible, enroll the patient in clinical trial! AITL Role of Transplant Concluding Remarks • The key to getting a better understanding of these rare lymphoma subtypes and to improving patient outcomes lies in a collaborative effort and efficient enrollment of patients into clinical trials. • We also need more biologic studies to discern and understand clinicopathologic features of various PTCL subtypes better.