T cell lymphoma
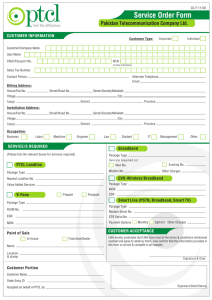
advertisement
How Can We Improve Therapy for T-cell Lymphoma? T cell lymphoma: What are the current standards of treatment? Should all patients be tested for CD30? Jia Ruan, M.D., Ph.D. Center for Lymphoma and Myeloma Weill Cornell Medical College New York Presbyterian Hospital Incidence of Peripheral T-cell Lymphoma 5-10% of all NHL in Western countries Most common: PTCL-nos, angioimmunoblastic, and ALCL Higher incidence, 15-20% of all lymphomas, in Asia Most common: PTCL-nos, NK/TCL, and ATLL J Clin Oncol 2008;26:4124-4130 WHO 2008 CLASSIFICATION: Mature NK/T-cell Neoplasms Nodal Disseminated •PTCL, NOS •AITL •ALCL, ALK+ •ALCL, ALK- Cutaneous •T-cell PLL •Mycosis fungoides •Sezary syndrome •T-cell LGL •Chronic lymphoproliferative •Primary cutaneous CD30+ LPD NK cells •Primary cutaneous •Aggressive NK-cell leukemia ALCL •ATLL •Lymphomatoid papulosis •Systemic EBV+ TCL •Subcutaneous Extranodal panniculitis-like Tcell lymphoma •NK/T-cell, nasal type •Primary cutaneous •Enteropathygamma-delta T-cell associated TCL •Other •Hepatosplenic TCL Blood. 2008;112:4384-4399 Peripheral T-cell Lymphoma: Prognosis International Prognostic Index (IPI) • • • • • Age >60 years Performance status ≥2 Serum lactate dehydrogenase level greater than the ULN Extranodal sites >1 Ann Arbor stage III or IV Prognostic Index for PTCL (PIT) • • • • Age >60 years Performance status ≥2 Serum lactate dehydrogenase level greater than the ULN Bone marrow involvement Blood 2004; 103; 2474-2479 PTCL: Outcome varies by subtypes and IPI 5-yr OS Diagnosis % IPI 0/1 IPI 4/5 PTCL-NOS 32% 50% 11% AITL 32% 56% 25% ALCL, ALK+ 70% 90% 33% ALCL, ALK- 49% 74% 13% ATLL 14% 28% 7% NKTCL, nasal 42% 57% 0 NKTCL, extranasal 9% 17% 0 Enteropathy-type 20% 29% 14% Hepatosplenic 7% 0 0 Subcutaneous panniculitis-like 64% 60% 0 J Clin Oncol 2008;26:4124-4130 Challenges in Management of T-cell lymphoma New Diagnosis Chemotherapy CHOP vs Other Relapse Chemotherapy Novel agents Transplantation Challenges: Difficulty to induce high quality and durability of responses. International T-cell Project: Role of Anthracycline PTCL-NOS AITL Other than ALK+ ALCL, no benefit of an anthracycline-containing regimen over a non–anthracycline-containing regimen. J Clin Oncol 2008;26:4124-4130 What do we actually get with first line CHOP? Citation Subtypes N ORR% CR % % Survival Savage et al PTCL-NOS 117 84 64 29 (5 yr-PFS) AITL 157 NR 46 30% (7-yr OS) PTCL(32) AITL(27) ALCLalk-(13) 83 79 39 ASCT PTCL(30) AITL(8) ALCL(5) 43 62 39 PTCL 29% 41 (2 yr-EFS) Lower for PTCL PTCL(34) AITL(12) 46 NR 39 26 (3 yr-OS) Ann Oncol 2004 Mourad et al Blood 2008 Reimer et al JCO 2009 Simon et al BJH 2010 Akagi et al J Clin Exp Hematop 2011 ORR 60-80+%, CR 30-60+% Durable remissions <20-30% Stratification based on IPI/PIT/Subtype PTCL: Can we do better than CHOP? Adding to the CHOP backbone CHOP + alemtuzumab CHOP + denileukin diftitox CHOP + bortezomib CHOP + etoposide Alternative intensive regimens Upfront SCT consolidation Novel strategies CHOP vs CHOP+ vs non-CHOP Possible incremental benefit by adding therapies to CHOP Benefit not equivalent in all subtypes (ALCL) Incremental benefit unlikely to significantly change prognosis Near MTD and toxicity soon outweighs benefit Non-CHOP intensive regimens are generally not better Autologous SCT as First-line Therapy in PTCL PFS, whole cohort 3-year PFS 36% 5-year PFS: 44% 1.0 4-year PFS: 44% 0.8 N=83 N=160 0.6 N=65 0.4 0.2 0.0 Time (months) 0 12 160 100 Number at risk 24 60 Time 85 65(months) 52 39 95% CI CHOP: ORR 79%, CR 39% Transplant rate 66% 36 48 months 72 17 Time (months) Survivor function CHOEP: ORR 82%, CR 51% Transplant rate 72% Reimer et al JCO 2009;27:106-113 D’Amore et al JCO 2012;30:3093-3099 MSKCC data (S Horwitz) CHOP/CHOP-ICE ORR 82%, CR 51% Relapsed PTCL: Spectrum of Disease BCCA registry 1976-2010: 191 patients with PTCL-nos, AITL, ALCL 38 received transplant (SCT 69%); 153 non-transplant candidates Panel 1: All 153 non-transplant pt Panel 2: 89 pt received chemoRx Median PFS 3.1 months Median PFS 3.7 months Median OS 5.5 months Median OS 6.5 months J Clin Oncol 2013;31:1970-76 Novel Therapy in Relapsed PTCL Agents Patient No. ORR % CR% PFS (mon) DOR (mon) OS (mon) Chemo (BCCA) 89 55 26 3.7 N/A 6.5 39 51 23 N/A N/A N/A 111 29 11 3.5 10.1 14.5 130 25 15 4 28 11.3 58 86 57 13.3 12.6 NR 60 50 28 3.6 3.5 6.2 54 22 11 2.5 3.6 N/A 31- AITL 15-AITL 4.6-AITL 3.5-AITL JCO 2013 Gemcitabine Ann Oncol 2010 Pralatrexate JCO 2011 Romidepsin JCO 2012 a Brentuximab JCO 2012 b Bendamustine JCO 2013 Lenalidomide EJC 2013 a: based on ASH2012 update b: includes ALCL patients only Histone Deacetylase (HDAC) Inhibitors Agents Romidepsin Belinostat Drug class Class I HDACi Class I&II HDACi 14 mg/m2 IV 4h, weekly 3 of 4 wks 1000 mg/m2 IV 30min, daily x 5, every 3 wks Dosing PTCL subtypes PTCL PTCL AITL Pt number 130 129 22 ORR 25% 26% 45% CR 15% 10% 18% TTR 1.8 months DOR 28 months 8.3 months 7.5 months PFS 4 months N/A 5.8 months OS 11.3 months N/A 9.2 months Thrombocytopenia (gr 3/4) Neutropenia (gr 3/4) Anemia (gr 3/4) 5.6 wk 24% 20% 11% JCO 2012;30:631-636 ASCO2013, abstract 8507; ICML2013, abstract 153 13% 13% 10% Brentuximab Vedotin: Antibody-Drug Conjugates CD30 Expression in PTCL 195 cases of PTCL from western Europe. Semi-quantitative evaluation of IHC positive tumor cells %. Transcriptomic CD30 mRNA levels were evaluated in parallel. ICML2013, abstract 151 Brentuximab Vedotin: Phase II study in CD30+ NHL •NCT01421667 •29 patients with PTCL enrolled: AITL (11) and PTCL-NOS (18) •CD30 expression ranged from 5-100% •Brentuximab vedotin 1.8 mg/kg IV over 30 min every 21 days •22 evaluable: ORR 36% (6 CR, 2 PR), DoR not reached •Subset in AITL (10): ORR 50% (4 CR, 1 PR), DoR NR •Safety data consistent with profile of BV Ongoing Analysis of Correlation of CD30 expression with response ICML2013, abstract 152 Other Potentially Promising Drugs/Combinations KW-0761, (CTCL and PTCL) HuMax CD4 (CTCL and PTCL) Aurora Kinase Inhibitor PI3K inhibitor IPI-145 Plitidepsin L-asparaginase (NK/T cell Lymphoma) Pralatrexate-Romidepsin Romidepsin-Bortezomib Romidepsin-lenalidomide Carfilzomib T-cell Lymphoma: New Treatment Paradigms Chemotherapy New Diagnosis CHOP vs Other Clinical Trials Relapse Novel Treatment Clinical Trials Transplantation Changing Standard Treatment Paradigms Moving New Therapies Upfront? Pharma/Registration/FDA guided approaches = X+CHOP vs CHOP Ongoing or planned randomized upfront studies BV+CHP vs CHOP (NCT01777152) Romi+CHOP vs CHOP (NCT01796002) Belinostat+CHOP vs CHOP (NCT01839097) ?Aurora kinase + CHOP vs CHOP ?HuMax CD4 + CHOP vs CHOP Maintenance Strategies CHOP +/- Pralatrexate maintenance (NCT01420679) Consolidation High dose + autoSCT High dose + autoSCT + romidepsin (NCT01908777) Optimize Treatment in TCL: More Questions than Answers Frontline setting CHOP is inadequate for most Standard of care should be clinical trial when possible Is adding a new drug to CHOP a winning strategy? • Entirely new regimens? e.g. SMILE for NK/T • Novel biologics based therapy? • HD consolidation vs. maintenance strategies? Relapse/refractory setting When to prioritize chemo over biologics? Is there an algorithm to cycle through various biologics? SCT vs. maintenance? Acknowledgement Lymphoma program, Weill Cornell Medical College • John Leonard, M.D. • Morton Coleman, M.D. • Richard Furman, M.D. • Peter Martin, M.D. Lymphoma program, MSKCC • Steve Horwitz, M.D.