OSCE (Answer)
advertisement
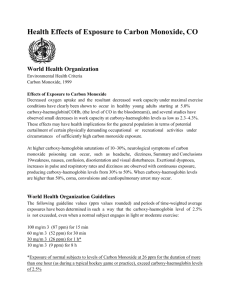
ospe KWH Case 1 • M/38 • Right shoulder contusion after S/F • PE: tenderness and swelling over his right upper chest . No skin impingement and no external wound found. No distal neurological deficit elicited Questions • 1) what is the diagnosis? • 2) what is the classification of the fracture? • 2) what is the management? Fracture clavicle Type I • Type I • distal to the coracoclavicular ligaments. • Coracoclavicular ligaments remain intact, • Displacement uncommon. • Treatment = sling. • Conoid ligament • Trapezoid ligament • Coracoid process • Acromion • Clavicle Type IIA • Type IIA • medial to the coracoclavicular ligaments. • Medial fragment frequently displaces superiorly. • Nonunion is frequent. • Treatment = ORIF. Consider hook-plate fixation (Haider SG, JSES 2006;15:419). Consider non-absorbable suture fixation. (Levy O, JSES 2003;12:24). Type IIB • Type IIB • Between the coracoclavicular ligaments. • Medial fragment frequently displaces superiorly. • Nonunion is frequent. • Treatment = ORIF. Consider hook-plate fixation (Haider SG, JSES 2006;15:419). Consider non-absorbable suture fixation. (Levy O, JSES 2003;12:24) Type III • Type III • Intra-articular, frequently without ligament disruption. • Generally little or no displacement. • Frequently missed or misdiagnosed as acromioclavicular joint injuries. • May lead to AC arthritis. • Treatment = sling. Consider distal clavicle excision for patients who are symptomatic at 6-12 months after injury. Case 2 • F/6 • Left elbow contusion after S/F in 2 months ago • c/o: persistent pain after the injury • PE: tenderness and swelling over her left elbow. ROM: 0-90 degree. No distal neurological deficit elicited. • X rays left elbow was taken Questions • 1) what is the diagnosis? • 2) what is the associated injury to look for? • 3) what is the management? Answers • Dislocated radial head • Plastic deformity of ulna shaft • Dx : greenstick Monteggia # with anterior radial head dislocation • Rx : ulnar correctional osteotomy + CR radial head +annular ligament repair Case 3 • • • • M/70 Left shoulder contusion after S/F PE: left shoulder in abducted position X rays of left shoulder was taken Questions • 1) what is the diagnosis? • 2) what is the method of reduction? Inferior shoulder dislocation (luxatio Erecta) • Rare , <1% • Result from forceful hyperabduction of shoulder • Reduction method: • 1) Axial (inline) traction • 2) Two step reduction The axial traction/countertraction method. Axial traction is applied to the arm with parallel countertraction using a sheet wrapped over the shoulder. Increasing the degree of abduction (if possible) and applying cephalad pressure to the displaced humeral head (star) can aid in reduction. After reduction of the inferior dislocation, adduct, supinate, and immobilize the arm for postreduction radiography. Step one, part one. Push anteroinferiorly on the mid humerus with hand A while "pulling" posteriorly on the medial condyle with hand B. Step one, part two. After conversion of the inferior to an anterior dislocation, adduct the arm and grasp the patient's wrist Step two. Hand A holds the patient's arm in abduction while hand B externally rotates the arm to reduce the now anteriorly dislocated humeral head. Case 4 • M/24 • He complained of epigastric and LUQ abdominal pain after having been assaulted by someone on two days ago. • PE: tenderness over his LUQ abdomen. No external wound was found. • BP 148/74 mmHg P93/min SaO2 99% • His BP drop to 60/30 mmHg after admission and return to 130/70 mmHg after 1000 ml gelofusin infusion. • Urgent CT was performed Plain films Plain films Plain films Contrast film Contrast films Contrast films Contrast films Contrast films Delay contrast films Delay contrast Delay contrast Delay contrast Questions • 1) describe the CT findings • 2) what is the diagnosis? • 3) What is the abnormal CT findings that indicate surgical intervention ? • 4) what is the management? Answers • Hyperdense peri-splenic hematoma • Scatter intrasplenic hypodense area, suggestive of hematoma and ischemic area • Curvilinear ill-defined hyperdensities are seen within the hypodense region, suggestive of active bleeding • Contrast brush in intrasplenic hypodense area in delay contrast films • Dx : intrabdominal hematoma due to splenic laceration and presence of active bleeding • Rx : spleenectomy Case 5 • F/25 • She attempted suicide by burning charcoal at home • PE: GCS 14/15, BP 98/73 mmHg, Pulse 83/min, SaO2 99% on 100%O2 • Systems review were unremarkable. No focal neurological sign elicited. Question • 1) describe the CT findings • 2) what is the diagnosis? • 3) what is the management? Answers • Symmetrical hypodensity noted at bilateral basal ganglia • Compatible with CO poisoning • Rx : stabilize ABC • Administer 100%O2 via tight fitting face mask • Intubate and provide IPPV on 100%O2 if unconscious • Record ECG, check ABG, COHB level • Consider hyperbaric oxygen therapy if • COHB >25%, pregnant patients with COHB >10%, myocardial ischemia, worsening symptoms despite oxygen therapy, all patients with syncope, neurological or cardiac abnormalities with elevated COHB Case 6 • F/25, Phx depression • Attempted suicide by drug overdose • PE: unconscious, GCS 4/15, BP 100/60 mmHg Pulse 70/min • She was intubated in AED. Questions • 1) describe the ECG finding • 2) what is the diagnosis? • 3) what is the mangement? Answers • Widening QRS complex, terminal 40ms rightward axis shift, non-sustained VT • Dx : TCA overdose • RX : stabilize ABC • Sodium bicarbonate boluses and infusion to narrow QRS to <100ms and keep PH 7.45 to 7.55 Case 7 • M/37 • Family history of premature death of unknown cause • Complained of palpitation and atypical chest discomfort for few episodes. • PE: BP 140/80 mmHg P 95/min • Systems review were unremarkable. Questions • 1) describe the ECG findings • 2) what is the diagnosis? • 3) what is the management? Answers • Sinus rhythm with ST segment elevations in V1-V3 • Dx : brugada syndrome • Associated with syncope and sudden death • PE and echocardiogram to exclude other cardiac causes • Electrophysiologic study to determine the inducibility of arrhythmias for risk stratification • Serum K & Ca levels : ECG patterns in hyperkalemia and hypercalcemia similar to that of brugada syndrome • Cardiac enzyme and troponin in patients with symptoms compatible with ACS • No pharmacological therapy has proven to reduce the occurrence of ventricular arrhythmias or sudden death • The only proven effective treatment in prevent sudden death and treating Ventricular arrhythmias is implantation of an automatic implantable cardiac defibrillator (ICD).