POSTER - Directed vs Non Directed Second Stage Labor Care and
advertisement
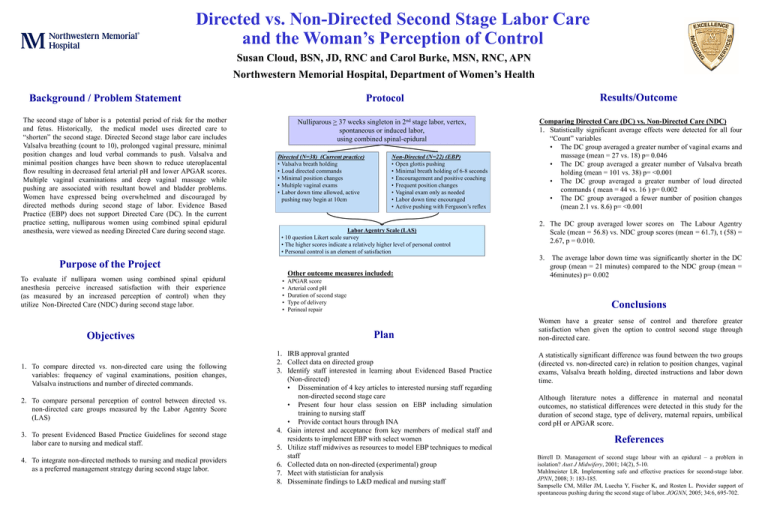
Directed vs. Non-Directed Second Stage Labor Care and the Woman’s Perception of Control Susan Cloud, BSN, JD, RNC and Carol Burke, MSN, RNC, APN Northwestern Memorial Hospital, Department of Women’s Health Background / Problem Statement The second stage of labor is a potential period of risk for the mother and fetus. Historically, the medical model uses directed care to “shorten” the second stage. Directed Second stage labor care includes Valsalva breathing (count to 10), prolonged vaginal pressure, minimal position changes and loud verbal commands to push. Valsalva and minimal position changes have been shown to reduce uteroplacental flow resulting in decreased fetal arterial pH and lower APGAR scores. Multiple vaginal examinations and deep vaginal massage while pushing are associated with resultant bowel and bladder problems. Women have expressed being overwhelmed and discouraged by directed methods during second stage of labor. Evidence Based Practice (EBP) does not support Directed Care (DC). In the current practice setting, nulliparous women using combined spinal epidural anesthesia, were viewed as needing Directed Care during second stage. Nulliparous > 37 weeks singleton in 2nd stage labor, vertex, spontaneous or induced labor, using combined spinal-epidural Directed (N=38) (Current practice) • Valsalva breath holding • Loud directed commands • Minimal position changes • Multiple vaginal exams • Labor down time allowed, active pushing may begin at 10cm Non-Directed (N=22) (EBP) • Open glottis pushing • Minimal breath holding of 6-8 seconds • Encouragement and positive coaching • Frequent position changes • Vaginal exam only as needed • Labor down time encouraged • Active pushing with Ferguson’s reflex Labor Agentry Scale (LAS) • 10 question Likert scale survey • The higher scores indicate a relatively higher level of personal control • Personal control is an element of satisfaction Objectives 1. To compare directed vs. non-directed care using the following variables: frequency of vaginal examinations, position changes, Valsalva instructions and number of directed commands. 2. To compare personal perception of control between directed vs. non-directed care groups measured by the Labor Agentry Score (LAS) 3. To present Evidenced Based Practice Guidelines for second stage labor care to nursing and medical staff. 4. To integrate non-directed methods to nursing and medical providers as a preferred management strategy during second stage labor. Comparing Directed Care (DC) vs. Non-Directed Care (NDC) 1. Statistically significant average effects were detected for all four “Count” variables • The DC group averaged a greater number of vaginal exams and massage (mean = 27 vs. 18) p= 0.046 • The DC group averaged a greater number of Valsalva breath holding (mean = 101 vs. 38) p= <0.001 • The DC group averaged a greater number of loud directed commands ( mean = 44 vs. 16 ) p= 0.002 • The DC group averaged a fewer number of position changes (mean 2.1 vs. 8.6) p= <0.001 2. The DC group averaged lower scores on The Labour Agentry Scale (mean = 56.8) vs. NDC group scores (mean = 61.7), t (58) = 2.67, p = 0.010. 3. Purpose of the Project To evaluate if nullipara women using combined spinal epidural anesthesia perceive increased satisfaction with their experience (as measured by an increased perception of control) when they utilize Non-Directed Care (NDC) during second stage labor. Results/Outcome Protocol Other outcome measures included: • • • • • APGAR score Arterial cord pH Duration of second stage Type of delivery Perineal repair The average labor down time was significantly shorter in the DC group (mean = 21 minutes) compared to the NDC group (mean = 46minutes) p= 0.002 Conclusions Plan 1. IRB approval granted 2. Collect data on directed group 3. Identify staff interested in learning about Evidenced Based Practice (Non-directed) • Dissemination of 4 key articles to interested nursing staff regarding non-directed second stage care • Present four hour class session on EBP including simulation training to nursing staff • Provide contact hours through INA 4. Gain interest and acceptance from key members of medical staff and residents to implement EBP with select women 5. Utilize staff midwives as resources to model EBP techniques to medical staff 6. Collected data on non-directed (experimental) group 7. Meet with statistician for analysis 8. Disseminate findings to L&D medical and nursing staff Women have a greater sense of control and therefore greater satisfaction when given the option to control second stage through non-directed care. A statistically significant difference was found between the two groups (directed vs. non-directed care) in relation to position changes, vaginal exams, Valsalva breath holding, directed instructions and labor down time. Although literature notes a difference in maternal and neonatal outcomes, no statistical differences were detected in this study for the duration of second stage, type of delivery, maternal repairs, umbilical cord pH or APGAR score. References Birrell D. Management of second stage labour with an epidural – a problem in isolation? Aust J Midwifery, 2001; 14(2), 5-10. Mahlmeister LR. Implementing safe and effective practices for second-stage labor. JPNN, 2008; 3: 183-185. Sampselle CM, Miller JM, Luecha Y, Fischer K, and Rosten L. Provider support of spontaneous pushing during the second stage of labor. JOGNN, 2005; 34:6, 695-702.