Otitis Media
advertisement
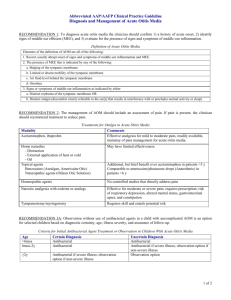
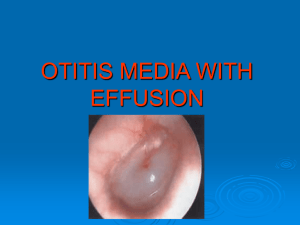
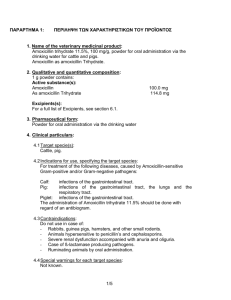
K. Myra Lalas Peds PGY 2 Definitions 1. Otitis media with effusion (OME)- presence of middle ear effusion without sings or symptoms of infection 2. Acute Otitis Media (AOM)- infection of the middle ear with acute onset of signs and symptoms, MEE, and signs and symptoms of middle ear inflammation. 3. Treatment- failure AOM- lack of improvement in signs and symptoms w/in 48-72 hrs after beginning antibiotics 4. Recurrent AOM- >=3 episodes of AOM occurring in the previous 6 mns or >=4 episodes in the past 12 mns 5. Chronic OM- OME persisting > 3mns 6. Chronic suppurative otitis media (CSOM)- purulent otorrhea assoc with a chronic TM perforation persisting > 6 wks despite appropriate treatment for AOM Symptoms of AOM Otalgia Fever Otorrhea Recent onset of anorexia Irritability Vomiting Diarrhea Epidemiology seasonal peak: winter peak age incidence: 6-18 mns of age Risk Factors for Developing Acute or Chronic OME or AOM ● Age <2 years ● Atopy ● Bottle propping ● Chronic sinusitis ● Ciliary dysfunction ● Cleft palate and craniofacial anomalies ● Child care attendance ● Down syndrome and other genetic conditions ● First episode of AOM when younger than 6 months of age ● Immunocompromising conditions Pathogenesis The middle ear space experiences slight negative pressure relative to the environment. Opening the eustachian tube intermittently during yawning or chewing relieves the negative pressure. Eustachian tube dysfunction (URI, GER, AR, craniofacial abnormalities)- negativ e P deepens (TM retracts)nasopharyngeal or oropharyngeal contents may reflux through the eustachian tube; inc neg P can also cause increased vasuclar permeability (effusion may develop). Microbiology 1. S. pneumoniae 2. Nontypeable H. influenzae- usu seen in those with recurrent AOM or AOM with treatment failure - otitis-conjunctivitis syndrome is assoc with isolation of this pathogen from the middle ear and cinjunctiva in older kids 3. M. catarrhalis 4. S. pyogenes 5. Group B Strep 6. S. aureus 7. for CSOM- P. aeruginosa, S. aureus, anaerobes occ, S. pneumoniae and nontypeable H. influenzae rarely PE Findings TM landmarks Normal TM OME: opaque or cloudy TM; visible AFL or air bubbles in middle ear; immobile TM on pneumatic otoscopy A normal (left) ear drum and an ear with acute otitis media (right). Note the thin clear tympanic membrane (ear drum) on the left. The ear with acute otitis media has a bulging tympanic membrane (due to pus in the middle ear) and increased redness over portions of the drum. AAP Recommendations Evidence-based clinical practice guideline that provides recommendations to PCP’s for the management of children from 2 months -12 years of age with uncomplicated AOM. Excluded are: anatomic abnormalities such as cleft palate, genetic conditions such as Down syndrome, immunodeficiencies, and the presence of cochlear implants. Also excluded are children with a clinical recurrence of AOM within 30 days or AOM with underlying chronic OME. Criteria for Initial Antibacterial-Agent Treatment or Observation in Children With AOM Age <6 mo 6 mo to 2 y 2y Certain Diagnosis Antibacterial therapy Antibacterial therapy Antibacterial therapy if severe illness; observation option* if nonsevere illness Uncertain Diagnosis Antibacterial therapy Antibacterial therapy if severe illness;* observation option if nonsevere illness Observation option* If the patient fails to respond to the initial management option within 48 to 72 hours, the clinician must reassess the patient to confirm AOM and exclude other causes of illness. If AOM is confirmed in the patient initially managed with observation, the clinician should begin antibacterial therapy. If the patient was initially managed with an antibacterial agent, the clinician should change the antibacterial agent. Temperature 39°C and/or Severe Otalgia Clinically Defined Treatment Failure at 48– 72 Hours After Initial At Diagnosis for Patients Being Treated Initially Management With Observation Option With Antibacterial Agents Recom Alternative for Penicillin Allergy Recom Alternative for Penicillin Allergy Clinically Defined Treatment Failure at 48– 72 Hours After Initial Management With Antibacterial Agents Recom Alternative for Penicillin Allergy No Amoxicillin, Non-type I: Amoxicillin, Non-type I: Amoxicillin- Non-type I: 80–90 mg/kg cefdinir, 80–90 mg/kg cefdinir, clavulanate, ceftriaxone, per day cefuroxime, per day cefuroxime, 90 mg/kg per 3 days; type cefpodoxime cefpodoxime day of I: ; type I: ; type I: amoxicillin clindamycin azithromycin azithromycin component, , clarithro , clarithro with 6.4 mg/kg per day of clavulanate Yes Amoxicillin- Ceftriaxone, clavulanate, 1 or 3 days 90 mg/kg per day of amoxicillin, with 6.4 mg/kg per day of clavulanate Amoxicillin, Ceftriaxone, Ceftriaxone, Tympanocen clavulanate, 1 or 3 days 3 days tesis, 90 mg/kg per clindamycin day of amoxicillin, with 6.4 mg/kg per day of clavulanate Antimicrobial prophylaxis for recurrent OM Children < 2yo benefit the most if a child has had > = 3 episodes of AOM in 6 mns or 4 episodes in 4 mns, s/he should be considered a candidate for chemoprophylaxis. give 1/2 the treatment dose of either amoxicillin or sulfonamides qdaily over 6 mns ideally during winter and spring a new episode of AOM in a child receiving chemoprophylaxis should be managed with a different antibiotic Treatment CSOM- topical antibiotics (usu ciprofloxacin); if with copious amount of pus, do daily suctioning before instilling the topical antibiotics OME- expectant management for low-risk children. Risk factors: developmental delay, hearing loss, evidence of injury to the TM or middle ear - tympanostomy tube placement for those with persistent OME or those with risk factors for developmental delay or evidnece of damage to the middle ear Complications Intratemporal Intracranial Hearing loss TM perf CSOM Cholesteatoma Tympanosclerosis Mastoiditis labyrinthitis Meningitis Subdural empyema Brain abcess Extradural abscess Lateral sinus thrombosis Cholesteatoma Destructive and expanding growth consisting of keratinizing epithelium in the middle ear and/or mastoid process, usu from tear in the TM TM perforation Mastoiditis A 2½-year-old boy is not yet saying any words. His parents are worried that he is not developing like his peers and are concerned that he is not yet talking. Other than two episodes of otitis media in the past year, he has been in good health. A formal audiology evaluation reveals normal hearing. His head circumference is at the 90th percentile; his weight and height are at the 75th percentile. His physical examination findings are normal. His father did not talk until he was 3 years old. Of the following, the MOST appropriate next step is to order electroencephalography order head magnetic resonance imaging reassure the parents and have the child return in 6 months refer the child for developmental evaluation refer the child for neurologic evaluation You are precepting a group of residents in continuity clinic. Several of them have seen patients who have earaches and have diagnosed acute otitis media. One resident says that he read that antibiotic treatment is not always necessary in these cases, and he wants to observe one of his patients with pain medication only. You tell him that this is only a reasonable option for certain children, and proper follow-up must be ensured. Of the following, the patient who would be treated MOST appropriately with observation and pain management rather than antibiotic therapy is a 4-month-old who has a temperature of 38.4°C and an air- fluid level behind a mobile, erythematous tympanic membrane a 6-month-old who has a temperature of 38.9°C and fluid behind an erythematous, immobile tympanic membrane a 9-month-old who has a temperature of 38.0°C and a shiny, pink tympanic membrane that moves well with insufflation a 15-month-old who has a temperature of 39.5°C and purulent drainage from the external auditory canal a 21-month-old who has a temperature of 38.1°C and an erythematous, bulging tympanic membrane References Gould, JM and PS Matz. Otitis media. Peds in Rev: 2010; 31; 102-116. Subcommittee on Management of Otitis Media. Diagnosis and Management of Otitis Media. Pediatrics: 2004; 113; 1451-1465. aap.org emedicine.com