Uterine blood flow and tocolysis
advertisement
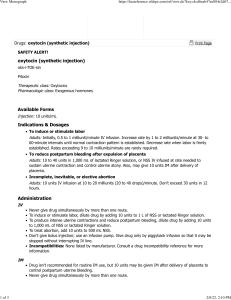
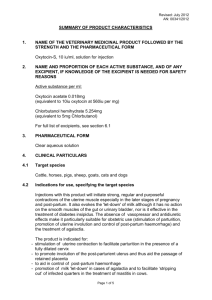
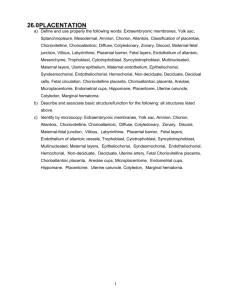
Uterine blood flow and tocolysis Tom Archer, MD, MBA UCSD Anesthesia Uterine blood flow (UBF) • Fetal O2 supply depends on adequate perfusion of placental lacunae. • Adequate perfusion requires high inflow pressure and low outflow pressure avoid aorto-caval compression with LUD. • UBF stops during uterine contraction need to avoid hyperstimulation from too much oxytocin. ) Normal placental function: fetal and maternal circulations separated by thin membrane (syncytiotrophoblast). Umbilical artery (UA) Umbilical vein (UV) Fetus “Lakes” of maternal blood Fetal capillaries in chorionic villi Precariously oxygenated environment Uterine veins Mom Archer TL 2006 unpublished Uterine arteries www.siumed.edu/~dking2/erg/images/placenta.jpg from Google images www.childbirths.com/.../fetalmonitoringetc.htm Colman-Brochu S 2004 http://www.manbit.com/OA/f28-1.htm http://www.manbit.com/OA/f28-1.htm Manbit images Chestnut chap. 2 Short term: Why increase uterine tone? • Stop placental implantation site from bleeding. – Let baby breast feed nipple stimulation causes oxytocin release from posterior pituitary. – Exogenous oxytocin (causes hypotension) – Methylergonovine (Methergine). No in HBP. – Carboprost (Hemabate). No in asthma / COPD. May cause diarrhea. Short term: Why decrease uterine tone? • Entrapped placenta (uterus has contracted with placenta or fragments inside). • Retained placenta will not allow uterus to fully contract continued bleeding. • Methods to relax uterus (for manual removal): – – – – Traditional: halothane anesthesia (+ETT) Probably better: IV or SL NTG. NTG also helps placenta to separate How about a spinal or epidural? What will they do? Not do? Tocolysis • Current OB practice: – no tocolytics after 34 weeks (because 34 weekers do very well) – If membranes are ruptured, don’t delay delivery (chorioamnionitis neurological injury to fetus). – Does tocolysis improve outcomes before 34 weeks? You can delay delivery, but are you accomplishing anything? We don’t know. Hauth JC Semin Perinatol 30:98-102 © 2006 Tocolysis: Why decrease uterine tone? • Allow time for betamethasone to promote lung maturation (before 33 weeks). • Does tocolysis before 34 weeks improve outcomes? • Maybe not. • If membranes are ruptured, delaying delivery may allow chorioamnionitis and fetal damage Management of spontaneous preterm labor • < 33 weeks, steroids. • < 34 weeks consider tocolysis • < 37 weeks, group B strep prophylaxis Hauth JC Semin Perinatol 30:98-102 © 2006 Tocolytics • Ethanol (historical interest). • MgSO4– NOT! • And, >50 gm MgSO4 associated with neonatal brain damage (IVH) (Mittendorf R Journal of Perinatology (2006) 26, 57–63). • Beta agonists (terbutaline, ritodrine). Pulmonary edema, tachycardia, hypotension, anxiety • Cyclooxygenase inhibitors (indomethacin) • Ca++ channel antagonists (nifedipine)– 1st line drug • Oxytocin antagonists (atosiban)—1st line drug Hauth JC Semin Perinatol 30:98-102 © 2006