nalini obstetrical emergencies - Nursing PowerPoint Presentations
advertisement

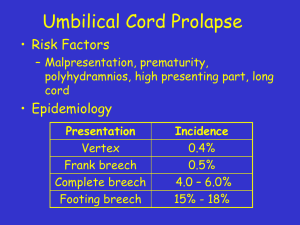
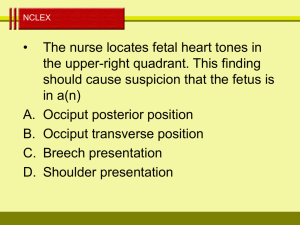
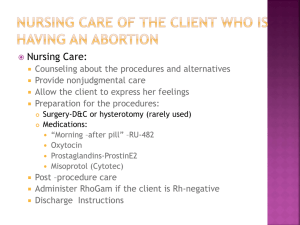
Every Mom’s Dream…... OBSTETRICAL EMERGENCIES Care is a state in which something does matter ; it is the source of human tenderness DEFINITION • AN UNFORESEEN COMBINATION OF CIRCUMSTANCES OR THE RESULTING STATE THAT CALLS FOR IMMEDIATE ACTION • LIFE -OR -DEATH SITUATION • INFREQUENT, UNANTICIPATED, UNPREDICTABLE NIGHTMARE Patient -1 • A 38 weeks G4P3 lady presents with ROM and contractions. She is quite distressed and thinks the baby is coming out. You perform a pelvic examination and next to the head you feel a pulsatile cord… Cord Prolapse • Presentation: Cord in front of presenting part before the rupture of membranes • Prolapse: Cord in front of presenting part after rupture of membranes Occult prolapse Cord lying alongside the presenting part Incidence (Anita pal, Kushgla, Sood 2006) • • • • • • • • Primigravida Multigravida Cephalic Frank breech Complete breech Footling Shoulder Contracted pelvis 0.45% 0.66% (Risk ratio 2:3) 0.3% 0.9% 5% 10% 15% 4-6 times Causes • • • • • • • • Malpresentation - face, brow, breech and shoulder Prematurity Polyhydramnios Multiple pregnancy Long cord (90-100 cm) PROM CPD Obstetric interventions - Amniotomy, Intrauterine pressure catheter, scalp electrode, external cephalic version, PROM, expectant management in preterm Dangers • • • • • • • Mortality rate as high as 50% Hypoxia Spasm of vessels Operative trauma to suboxgenated fetus More with vertex than breech Descent in front than behind More in primi than multi Diagnosis • • • • • Cord pulsations CTG shows variable decelerations Cord lying outside vulva USG – cord loops Fundal pressure causes bradycardia • Violent activity of baby • Meconium stained liquor Prevention • Refer to level II care • USG for malpresentation and cord presentation • Foetal mointoring • Avoid ARM in an unengaged head • PV exam after ROM Management • Lift presenting part off the cord • Instruct NOT to push • Position patient Knee chest Trendelenburg Exaggerated position Knee chest position Trendelenburg position Exaggerated sim’s position Management (cont..) • • • • • • Full bladder (Vago 1970) Vulval pad Replacement of cord Tocolysis (ritodrine) Forceps (Cx fully dilated) Second twin – internal podalic version and breech extraction • Stat C-section • Occult: Aminoinfusion Management (cont…) • Funic Reduction – Manual replacement of cord into uterus – Cord gently pushed above presenting part while other cord decompression techniques are applied – Rapid vaginal delivery Fetal Mortality • • • • • Overall - 50% 1st stage of labour - 70% 2nd stage of labour -30% Neonatal death - 4% Perinatal mortality- 20% < 5 minutes, prognosis good, > 5 mins, damage and death. VASA PRAEVIA • Fetal blood vessel lies in front of presenting part • Rupture - exsanguination of the fetus Cause and Management • Velamentous insertion Fresh bleeding vaginally with rupture of membranes • Management: Signs of fetal distress Stat C.S Send cord blood for Hb estimation PATIENT -2 Mother is pushing with each contraction and the baby’s head starts to come out. However, with each push, the baby’s head comes out and then retracts back in towards the perineum. You quickly recognize this as the “turtle sign” Obstructed labour • No advancement of presenting part despite strong, uterine contractions • Causes: Cephalo-pelvic disproportion Malpresentation shoulder/brow/persistent mento posterior Deep transverse arrest Pelvic mass Fetal abnormalities - Hydrocephalus, conjoined twins Causes Malpresentation: Signs of obstructed labour • • • • • • • • • Presenting part fails to advance Cervical dilatation slow Formation of retraction ring Early rupture of membranes Formation of elongated sac of forewaters If neglected, dehydration, ketosis Caput succedaneum and moulding urine output decreases fetal distress Management • • • • • Careful assessment of progress of labour Correct hydration Internal version Forceps application Stat C.Section Shoulder Dystocia • Incidence: 0.23% to 2.09% • Impaction of fetal shoulders in maternal pelvis • Head to body delivery time > 60s Risk factors • • • • • • Maternal Diabetes Mellitus Short stature Macrosomia Post-term Obesity Fetal shoulder circumference 40.9 ± 1.5cm Vs 39.5 ± 1.5 cm Complications Fetal morbidity: • Brachial plexus injury • Clavicular fracture • Facial nerve paralysis • Asphyxia • CNS injury • complication rate up to 20% Management Help – obstetrician, pediatrician Episiotomy Legs – elevate (McRoberts) Pressure - suprapubic Enter vagina – Rubin’s and Woods’ screw Roll or Remove posterior arm Zavanelli, Clavicular# , Symphysiotomy McRoberts Maneuver • hyperflexion of maternal hips • Increases intrauterine pressure (1,653mmHg - 3,262 mmHg) • Increases amplitude of contractions (103mm Hg to 129mm Hg) All-Fours Maneuver(Gaskin Maneuver) • Ina May Gaskin (1976) • changes pelvic dimensions in a similar way to McRoberts maneuver • apply downward traction to disimpact the posterior shoulder Suprapubic Pressure • direct posterior or oblique suprapubic pressure Rubin’s Maneuver • adduction of the most accessible shoulder • moves the fetus into an oblique position and decreases the bisacromial diameter Woods’ Cork Screw Maneuver • Abduct posterior shoulder exerting pressure on anterior surface of posterior shoulder Deliver posterior arm (Barnum Maneuver) grasp the posterior arm and sweep it across the anterior chest to deliver Zavanelli Maneuver • cephalic replacement via reversal of the cardinal movements of labor Clavicular Fracture • fracture the anterior clavicle by pushing it against the pubic ramus or using a closed pair of scissors • Symphysiotomy Complications • • • • • • Maternal morbidity 4th degree perineal lacerations Cervical & Vaginal lacerations Bladder injury Postpartum hemorrhage Endometritis Patient - 3 • Mother in third stage of labour. Using the controlled cord traction, the midwife tries to deliver the placenta. Unfortunately, notices the descent of uterus instead of placenta. Uterine Inversion • 1/20,000 deliveries Causes: • uterine atony (40%) • Increase in intra abdominal pressure • Fundal attachment of placenta (75%) • Short cord • Placenta accreta • Excessive cord traction Degrees of uterine inversion • 1st - Dimpling of fundus, remains above internal os • 2nd - fundus passes through the cervix, but lies inside vagina • 3rd - (complete) Endometrium with or without placenta is outside the vulva Dangers • Shock - Neurogenic Pressure on ovaries Peritoneal irritation • Hemorrhage • Pulmonary embolism • Infection Management • Uterine relaxant (terbutaline 0.25 mg IV followed by 2 g of MgSO4 over 10 min) • Treat hypovolumeia • Without placenta: Repositioning Uterine Inversion Management(cont…) • • • • • • With placenta: Do not remove placenta Replace uterus Bimanual compression Hydrostatic pressure (O’Sullivan 1945) Start oxytocin Laparotomy Patient - 4 A mother in second stage of labour suddenly complains of persistent pain, and bleeding per vagina becomes profuse and the monitor shows decelerations in fetal heart rate. Uterine Rupture • 1/2000 deliveries Types: • Complete • Incomplete • Rupture Vs Dehiscense of C.S scar Rupture of lower uterine segment Causes • Uterine injury sustained before current pregnancy C.S /hysterotomy/ repaired uterine rupture/ Myomectomy Uterine trauma - curette, sounds Sharp or blunt trauma - accidents, bullets, knives Congenital anomaly Causes Uterine injury during current pregnancy • Before delivery Intense spontaneous contractions Labour stimulation Intra-amnionic instillation Perforation by internal catheter External trauma - sharp or blunt External version Uterine overdistension - multiple pregnancy Causes (cont…) • During delivery: Internal version Difficult forceps delivery Breech extraction Difficult manual removal of placenta Fetal anomaly • Acquired: Placenta increta / percreta Retroverted uterus (sacculation) Diagnosis • Prolonged fetal decelerations (70.3%) • Bleeding (3.4%) Pain (7.6%) Monitor tracing demonstrating fetal heart rate decelerations, increase in uterine tone, and continuation of uterine contractions in a patient with Management Total Hysterectomy Sub total hysterectomy Simple repair Patient 5 Mother has just delivered a male baby. You wait for 30 minutes But no signs of placental separation and descent is present. Manual removal fails. Placenta Accreta • • • • • Incidence: 1 in 2,562 deliveries Firm adherence of placenta to uterine wall partial or total absence of decidua basalis Placenta increta: Villi invade the myometrium Placenta percreta: Villi penetrate myometrium Risk factors • Defective decidual formation placenta previa Previous cesearean scar uterine curettage • Grand multiparity Diagnosis and Management • Dx in third stage of labour • Maternal hemorrhage • Treatment: Hysterectomy Patient 6 • A pregnant mother on oxytocin induction suddenly becomes short of breath and tachypneic. Vital signs drop and the patient goes into asystolic arrest. Amniotic Fluid Embolism • Incidence: 1 in 3,500 to 1 in 80,000 • Amniotic fluid enters the maternal circulation and reaches pulmonary capillaries • Through a tear in amnion and chorion • Opening in maternal circulation • Increased intrauterine pressure Amniotic Fluid Embolism Risk factors • • • • • • • • Multiparity Large fetus Meconium in amniotic fluid Intrauterine fetal death Precipitate labour Placental abruption Intrauterine catheter Rupture of uterus Manifestations • Phase I : Pulmonary vasospasm Hypoxia Hypotension Cardiovascular collapse • Phase II: Left ventricular failure Pulmonary edema Hemorrhage Coagulation disorder Management • • • • • • • • • Intubation + Mechanical ventilation CVP monitoring Blood transfusion + I.V. Fluids Dopamine 2-20mg/kg/min IV Digitalization (0.1 - 1.0mg) Prostaglandin Morphine Aminophylline Hydrocortisone Be prepared, except the unexpected and above all, communicate • Communicate congruently • Careful, sympathetic and optimal communication • Avoid medical jargon • Psychological support- one member - Touch • “Talking through” the process • Smile of reassurance • Information and support to partners Fear during labour • Worries that infant may die or born with abnormality. • Review labour process • Provide with frequent progress report • Personal availability of nurse • Promise postnatal debriefing sessions NURSE’S ROLE IN INTRAPARTUM CARE COUNSELLOR CO ORDINATOR ADVOCATE NURSE MIDWIFE MANAGER RESEARCHER CARE GIVER EDUCATOR COMMUNICATOR Interestingly, loving care does not require twice the time,but it does require more than twice the presence.” - Erie Chapman THEY NEED YOU AND YOUR CARE