Chapter 13
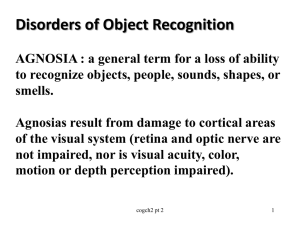
Disordered Seeing with Normal Eyes
A neurological approach to vision
Kate Denker Welch
History
1836- Charles Wheatstone describes stereoscopic vision
1844- A.L. Wigan described facial agnosia
1878 Herman Munk described “mind blindness” in a dog who had both
occipital lobes removed and could not recognize people, animals, or
things.
1887- Herman Wilbrand described “mind blindness” in a 64 yo F, who
could not connect visual information to current or past perceptions
1888- Louis Verry published a paper describing the relationship
between localized damage to the left occipital lobe and loss of color
vision in his patient Mme. R.
1890- Heinrich Lissauer defined two types of mindblindnessAssociative mind blindness and a type where there was a failure to
form adequate current perceptions
1891- Sigmund Freud coined the term “agnosia”
History Cont…
1917- During World War I, Captain George Riddoch (of the Royal Army
Medical Corps) described case studies of injured soldiers who had brain
injuries that resulted in visual agnosia.
1919- Gordon Holmes (neurologist for the British Expeditionary Force)
and Captain Gilbert Horrax (U.S. Army) described the loss of
stereoscopic vision and visual agnosia for depth in a soldier who was
shot through the head.
1947- Joachim Bodamer described three cases of prosopagnosia in
soldiers who had received a traumatic brain injury. He was the first to
use the term prosopagnosia.
1971- A.B. Ruben and D.F. Benson described “double dissociation”.
What Causes Visual Agnosia?
Damage to temporal, occipital, or the
parietal lobe.
Different types of agnosia relate to
specific damaged regions of the brain.
Overall, visual agnosia means that there
is an inability to recognize stimuli.
Visual Agnosia
Types:
Associative Visual Agnosia
Apperceptive Visual Agnosia
Color Agnosia
Object Agnosia
Prosopagnosia
Movement agnosia
Depth Agnosia
Associative Visual Agnosia
Inability to connect current perception of what is presented with
past experience.
Can not recognize something even though the shape itself can
be perceived. Perception exists but comprehension of perception
does not.
Can draw things that they do not recognize.
Damage to an area among the ventral stream.
Most common cause of associative visual agnosia is carbon
monoxide poisoning.
MRI of CO victim with Visual Agnosia
Apperceptive Agnosia
Typically related to damage in the ventral stream occipital
region
Inability to recognize and discriminate between overall shapes
and visual space
Can not copy or draw objects without great difficulty.
Visual Agnosia for Form
Form Agnosia is the inability to perceive
shape
Goodale and Miller described a case
study of a 34 yo woman called DF.
The Case of DF
34 yo F, lost consciousness from carbon monoxide poisoning. Awoke
from coma blind. Her vision returned after 10 days but with poor
perception of shape.She could identify things like the color or size of an
object (dorsal stream must be intact) but not the object itself (ventral
stream is damaged).
Tested by Melvyn Goodale and David Milner
Orientation test- asked to put a card through a slot
She failed that task but succeeded when asked to put it
through an imaginary slot
Efron square test- asked to discriminate between rectangle plaques
and square plaques. Next asked to estimate width of plaques with
her fingers.
She failed at the two tasks. She succeeded at a task where
she could pick up the plaque with appropriate finger width.
Drawing- She poorly copied drawings but was much better at
drawing objects from memory (despite not recognizing what she
had drawn).
Diagnosed with visual agnosia for form, the damage to her brain was
primarily in the ventral stream on visual areas V2, V3, and V4.
Ghent Overlapping
Contour
Boston Naming Test
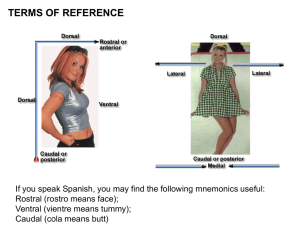
Dorsal (Green) and Ventral Pathways (Purple)
Visual Agnosia for Movement
Visual Agnosia for Movement
What is it?
Also known as motion blindness. It is the inability to detect
motion
What causes it?
Disruption to the “Where” pathway for processing vision
Damage to the brain caused by stroke, brain trauma, or
Alzheimer’s disease.
Damage to the middle temporal cortex, specifically visual
area 5 (V5) also known as the visual area MT (middle
temporal)
Why?
Area V5 is the part of the extrastriate visual cortex that
sends information from the dorsal stream to the inferior
parietal lobule
Zilhl’s Patient
“‘I see the world in snapshots – like the frames of a movie, but
most of the frames are missing.”
Patient was a 45 yo F who was admitted to the hospital with
headache, nausea, vertigo, and an inability to detect movement.
She had normal vision for color, shape, and facial recognition.
Zilhl’s patient had experienced a stroke that effected the V5
area of her brain and caused her to have motion blindness.
She was unable to see the movement of people, cars, or
objects. However, she could discriminate between movement
and stationary objects in her peripheral vision.
Evolutionarily, her intact peripheral vision for movement speaks
to the importance of peripheral vision in predator/prey tracking
and self-preservation.
Case of Colonel T.
Described by Captain George Riddoch of the Royal Army Medical
Corps during WWI
Colonel T. was shot in the head. His right occipital lobe was
damaged which resulted in his inability to see still objects in the
left visual field.
“Moving things” could be detected in the left visual field but
they looked grey blobs.
Visual Agnosia for Depth
What is it?
Lack of stereoscopic vision
What causes it?
Damage to right posterior hemisphere
Can also be caused by poor development
Case Studies of Depth Agnosia
Captain de W.
Described by George Riddoch
Cpn. W had shrapnel removed from his brain that dmaged the right
occipital lobe and left frontal lobe.
He lost all ability to understand depth and everything looked flat.
Riddoch determined that stereoscopic vision relies on more than
just binocular vision to produce 3 dimensional images.
George Holmes and Captain Gilbert Horax
They treated a soldier who had been shot through the back of the
head. The patient reported that everything looked flat to him.
Color Agnosia
What causes it?
Damage to the extrastriate visual cortex,
specifically the V4 area.
The visual area 4 (V4) is cut off from sending
information to the inferior temporal lobe. Without
the ability to send that information to the “What”
pathway of the temporal lobe, the color cannot be
recognized.
Color agnosia differs from color blindness just as recognition differs from
perception.
Color blindness is caused by a lack of genetic code for the cones
responsible for color vision in the retina therefore color can not be seen.
Color agnosia is caused by a lack of recognition for color in the visual
cortex.
Deficit a short film by Calum MacAulay
QuickTime™ and a
decompressor
are needed to see this picture.
Prosopagnosia
Prosopagnosia
What is prosopagnosia?
Inability to recognize faces. Also known as face blindness
Types of prosopagnosia:
Associative prosopagnosia
More common version
Less severe because faces are not recognized but facial
positioning is understood (they know where the mouth
and nose should be placed)
May be able to draw faces but not recognize the face
they drew
Apperceptive prosopagnosia
Faces are not recognized and facial position is not
understood
Drawing faces may be very difficult
May have covert recognition
Prosopagnosia
Why just faces? What about objects?
Fusiform gyrus responds to faces
Parahippocampal gyrus responds to inanimate objects
Double Dissociation- The areas for recognizing faces
and inanimate objects are separate therefore agnosia for
objects and prosopagnosia do not occur together
Parrahippocampal gyrus
Fusiform Gyrus
The Fusiform gyrus is located in the temporal
lobe
Image of Left Fusiform Gyrus (Visual Word Form Area -VWFA)
and Right Fusiform Gyrus (Weiner et al, 2004.)
The left fusiform gyrus (
referred to as the visual
word form area) is
responsible for word
recognition.
The right fusiform gyrus
is (referred to as the
fusiform face area)
responsible for facial
recognition.
What Causes Prosopagnosia?
Damage to occipitaltemporal regions of the brain
Specifically the fusiform gyrus of the interior temporal cortex
The cause of damage can be from head injury, degenerative
diseases (ex. Alzheimer’s and Parkinson’s disease), right
temporal lobe atrophy, encephalitis, or strokes (ex. Posterior
cerebral artery stroke or transient ischemic attack).
There is also a genetic form of prosopagnosia that can be passed
down from a parent to child. Prosopagnosia can also be the result
of a developmental disorder.
Evolutionarily facial recognition is important
There must be an adaptive benefit for facial recognition. Newborns
show great preference for human faces despite their poor visual acuity.
Newborns use eye contact and facial expressions to engage caretakers
to take care of their needs. Socially facial recognition became essential
to survival because it provides self-identity, identity for group
members, and identity for non-group member (could be an enemy?).
Early Descriptions
A.L. Wigan was the first to describe prosopagnosia
Bodamer’s Case studies (1947)
Joachim Bodamer was the first to use the term prosopagnosia
He published a paper about three German soldiers with TBI. In
describing their condition, Bodamer named the disorder
prosopagnosia. Today most psychologists would not consider those
cases to be prosopagnosia. One of the soldiers could recognize
faces but said the features were “grossly distorted.” Another soldier
seemed to have a problem in perceiving faces rather than not
being able to recognize them.
Modern Experiments
Justine Sergant- Modular View of facial
processing
Used PET and MRI scans to measure blood flow in
the brains of young men performing visual spatial
tasks
Vertical/Horizontal bars
Objects
Unfamiliar Faces- Which sex?
Familiar Faces
Showed that brain used three separate areas for
processing tasks
MRI of Fusiform Gyrus activating in response to facial pictures
( Pelphrey KA, Mack PB, Song A, G毟eldere G,& McCarthy G. 2003)
Brain activation is shown in red and deactivation in blue
Covert Recognition in Facial Agnosia
The patient cannot recognize faces explicitly but on an
unconscious level the patient recognizes it but it not aware that
recognition took place.
Evolutionarily the ability to know where something was arose
before the ability to know what something was. Facial
recognition follows the same eye to brain process as perceiving
movement but evolutionary different parts of the visual cortex
developed to reroute the information to the appropriate area. In
covert recognition, the ability to process and recall a face has
been disrupted and only unconscious awareness remains.
Tests for covert recognition
Celebrity face test
Matching faces
Category Test of Celebrities
The Case of PH
19 yo M, head injury from motorcycle accident
Awoke from a coma after 12 days and discovered he could no
longer recognize faces
He had no overt ability to recognize faces
On covert recognition tasks, he was slow in replying and
recognition occurred even though he was unaware of it.
Blind Sight
Blind sight is also known as unconscious vision.
Discovered by E. Poppel at MIT
Noticed that brain damaged patients who reported some
visual field blindness were able to follow the movement of a
light shone in the “blind spot” of their visual field. Although
the patients denied moving their eyes in the correct
direction, nevertheless their eyes followed the light even
without their knowledge.
Larry Weiskrantz named the disorder blindsight after studying a
patient named DB.
Case of DB
34 yo M, had a section of his right visual cortex removed with
the surgical removal of a tumor.
He experienced blindness in his left visual field, however, he
could still identify stimuli during testing on that side. When
asked to
Despite reporting no visual sensation or awareness of vision in
his left field, he could accurately answer the experimenter’s
questions about the visual stimuli.
Patient DB could detect the horizontal degree of change for the lines on the
circles. He could detect how much they changed as long as it was more than 10
degrees from horizontal. DB’s visual acuity could be determined from this test.
Non-Invasive Methods for Scanning the
Living Brain
MRI- Magnetic Resonance Imaging
ProsFunctional MRI can detect brain activity
Can detect tumors with good accuracy
Can detect differences between normal and diseased
similar tissue
Cons
Expensive
Magnetic force could be a problem for implantable
devices
PET- Positron Emission Tomography
Pros
Can detect brain activity during different tasks
Can see how glucose is metabolized in brain
Cons
Radioactive injection
Non-Invasive Methods for Scanning the
Living Brain
CAT- Computed Axial Tomography
Pros can help detect intercranial hemorrhages, strokes, and
some tumors
Help plan surgery
Slides can be rendered into a 3D model
ConsCannot detect artery blockage before a stroke,
intercranial pressure, as well as not the best tool for
detecting tumors
Contrast can not pick up differences between similar
tissues
Ionizing radiation exposure
Allergic reaction to iodine contrast agent
fMRI Visual Spatial Study
QuickTime™ and a
Sorenson Video 3 decompressor
are needed to see this picture.
Questions
1. Describe some of the early cases of visual agnosia (or mind-blindness). What
is the central deficit of the disorder?
2. Describe the case of DF, what sort of tests reveal the nature of her visual
deficit?
3. What is meant by 'double dissociation' between face and object
recognition? What does it indicate about the neural basis of these abilities? 4. What part of the brain was implicated in Bodamer's early studies of
prosopagnosia? Why wouldn't these cases be consider prosopagnosia today?
5. What is covert recognition? How is it measured and what does it indicate
about the evolutionary origins of processing facial information?
6. What dissociations of movement perception have been revealed by different
types of brain damage?
7. What is blindsight and what part(s) of the brain is (are) implicated in it?
8. Describe the three major non-invasive methods for monitoring on-going
brain activity and their strengths and weakness: CAT; MRI; PET.