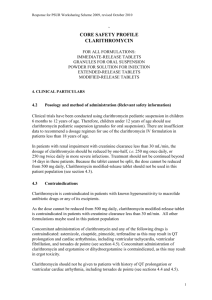
Diagnosis, Treatment, and Prevention of Nontuberculous
advertisement
Diagnosis, Treatment, and Prevention of Nontuberculous Mycobacterial Diseases American Thoracic Society Documents Am J Respir Crit Care Med 2007; 175:367416 www.atsjournals.org Diagnostic Criteria CXR, or chest HRCT on non-cavitary disease 3 or > sputum for AFB Exclusion of other pulmonary dis, eg TB Mycobacterium avium complex (MAC), M kansasii, M abscessus Pulmonary symptoms, nodular or cavity in CXR, HRCT shows multifocal bronchiectasis with nodules Positive culture: 2 sputums or 1 bronchial lavage Lung biopsy with granuloma or AFB, culture+NTM Susceptibility testing for MAC: clarithromycin only M kansasii: rifampin only M fortuitum, M abscessus, M chelonae: amikacin, imipenem, doxycycline, the fluoroquinolones, a sulfonamide, cefoxitin, clarithromycin, linezolid, tobramycin Prophylaxis and Treatment of NTM Disease MAC Pulmonary Disease Nodular/bronchiectatic MAC lung disease;initial 3 times weekly regimen Clarithromycin 1000 mg or azithromycin 500 mg Rifampin 600 mg Ethambutol 25 mg/Kg Follow with sputum culture monthly Treatment to be continued until culture negative for 1 year Prophylaxis and Treatment of NTM Disease MAC Pulmonary Disease Fibrocavitary or severe nodular/bronchiectasis,init Daily treatment Clarithromycin 500-1000 or azithro 250/day Rifampin 600 mg,or rifabutin 150-300 mg Ethambutol 15 mg/Kg, +/- 3 times weekly amikacin or streptomycin for 3 months. Treatment continued until culture negative for 1 year. Treatment of Macrolide-resistant MAC Lung Disease Analogous to treatment for drug resistant TB Risk factor for resis: macrolide monotheray, inadequate companion drug use. Parenteral aminoglycoside: parenteral streptomycin or amikacin Surgical resection (debulking) 4 drug regimen: INH, Rifampin, ethambutol, streptomycin for 3-6 mo moxifloxacin? INF gamma? MAC disseminated Clarithromycin 500 mg bid or azithro 500/d Ethambutol 15 mg/K/d +/- Rifabutin 300 mg/d (interferes with metabolism of protease inhibitors and mononucleoside reverse transcriptase inh. Therapy discontinued with resolution of symptoms and reconstitution of cell mediated immune function (CD4 count >100/mcL for 12 mo). Otherwise, treatment should be life long. Prophylaxis of Disseminated MAC disease When CD4 T-lymphocyte count is <50cells/mcL Azithromycin 1200 mg/week or clarithromycin 1000 mg/d or rifabutin 300 mg/d Treatment of M kansasii pulmonary disease INH 300 mg/d Rifampin 600 mg/d Ethambutol 15 mg/d Until culture negative for 1 year. Treatment for M abscessus pulmonary disease No drug regimen. Clarithromycin 1000 mg/d and multidrug reg Surgical resection of localized disease Treatment of nonpulmonary disease by RGM (M abscessus, M chelonae, M fortuitum) Based on in vitro susceptibilities. M absessus: a macrolide regimen is often used. Treatment of NTM cervical adenitis Mostly due to MAC Surgical resection with >90% cure rate A macrolide-based regimen for extensive MAC lymphadenitis. Epidemiology on NTM Widely distributed in the environment. Organisms found in soil and water, both natural and treated water sources. M kansasii, M xenopi, M simiae almost exclusively from municipal water sources. No evidence of animal-to-human or humanto-human transmission of NTM. Human disease acquired from environ exposures. Epidemiology NTM diseases in most industrialized countries: 1.0-1.8 cases per 100,000. CDC report of NTM: 75% pulmonary, 5% blood, 2% skin and soft tis, 0.4% lymph n. 1 mil population: MAC 29-36 isol, M fortuitum 4.6 to 6 isol, M kansasii 2-3.1 isol Southeastern US: higher isolation rates Pathogenesis HIV: disseminated NTM infection typically occurred only after CD4 T-lymphocyte is <50/microliter. In non-HIV, disseminated NTM infection assoc with specific mutation in INF gamma and IL-12 synthesis and response path. IFN-gamma receptor 1, IFN-gamma receptor 2, IL-12 receptor beta1 subunit, IL-12 subunit p40. the signal transducer and activator of transcription 1, and the nuclear factor-kappa beta essential modulator. An association between bronchiectasis, nodular pulmonary NTM infection and particular body habitus in postmenopausal woman: pectus excavatum, scoliosis, mitral valve prolapse. Host Defense Mycobacteria phagocytosed by macrophages, which produce IL-12, which up-regulates IFN-gamma. INF-gamma activates neutrophils and macrophages to kills intracellular pathogens. Positive feed back loop between INFgamma and IL-12. Disseminated NTM is manifestation of immunologic defect. Pulmonary Disease with NTM Predisposing lung diseases COPD Bronchiectasis (NTM often coexist) CF Pneumoconiosis Prior TB Pulmonary alveolar proteinosis Esophageal motility disorders Body Morphotype Woman with nodular NTM pulmonary infections associated with bronchiectasis have similar clinical characteristics and body type. So called Lady Windermere’s Scoliosis, pectus excavatum, mitral valve prolapse and joint hypermobility Hypersensitivity-like Lung Disease MAC exposure associated with hot tub use (“hot tub lung”) MAC has predisposition for growth in indoor hot tubs. Mycobacteria are relatively resistant to disinfectants and wide range of temp. Metal working fluids may cause similar disM. immunogenus, a rapidly growing M. Hot Tub Lung Subacute onset of dyspnea, cough, fever Occas hypoxemic respiratory failure Non-smokers Chest HRCT: diffuse nodular all over Culture from sputum, bronchial washing, tissue biopsy isolating MAC Treatment: removal, antimicrobials, corticosteroids. Tumor Necrosis Factor Inhibition NTF-alpha blocking agents, blocking antibodies infliximab and adalimumab and the soluble receptor etanercept lead to relatively high rate of active TB in latent infection. Relevance to NTM unknown