Presented by Gillian Longley RN, BSN, MSS
University of Nevada Las Vegas, November 2011
ETHICS:
The basic concepts and
principles of right human conduct.
KEY QUESTIONS
1.
Is it ethically acceptable to surgically alter the
natural genitals of a child, when no compelling
therapeutic reason exists?
2. Who is the appropriate person to give permission
for elective, nontherapeutic cutting of anyone’s
genitals?
OUTLINE
Principles of medical ethics and human rights
Ethics of common arguments for circumcision
Medical benefits rationales
Parents’ vs. child’s rights
Informed consent
Conscientious objection of health professionals
Pathways to a more ethical future
Four Principles of Medical Ethics
in relation to neonatal circumcision
Autonomy:
Does it respect the individual’s right to make his
own decisions?
Beneficence:
Is it reasonably expected to do good?
Non-maleficence:
Does it avoid doing unnecessary harm?
Justice:
Is it fair?
Human Rights: Key Documents
Universal Declaration of Human Rights (1948)
International Covenant on Civil & Political Rights (1966)
The Convention on the Rights of the Child (1989)
The Universal Declaration on Bioethics and Human
Rights (2005)
UNIVERSAL = NO EXCEPTIONS!
Human Rights: Key Principles
and circumcision
GENERAL RIGHTS:
Right to life, liberty, and security of person
Right to property
Right to freedom from torture, and cruel, inhuman, and degrading treatment
Right to equal protection before the law.
SPECIAL RIGHTS FOR CHILDREN:
Right to opportunities for children to develop physically, mentally, morally,
spiritually, and socially in a healthy and normal manner, and in conditions of
freedom and dignity.
Right to protection from all forms of mental and physical violence, injury, or
abuse, including sexual abuse.
Right of protection from traditional practices prejudicial to the health of
children.
Other medical ethics sources
AMA Code of Ethics
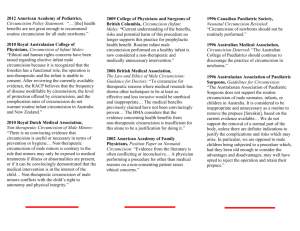
Circumcision position statements of medical
organizations (e.g. AAP, CPS, RACP, BMA, KNMG)
AAP Ethics Committee (1995): Informed consent,
parental permission, and assent in pediatric practice.
MEN’S VOICES
“When you do it to a
baby, there's no way
back. I’ll never know
what sex would be like
with a foreskin. It
makes me angry that
somebody else
decided for me,
to do something that
I probably would
not have done if
I was deciding
for myself.”
MEN’S VOICES
“I have never
been able to
accept the fact
that someone cut
part of my penis
off when I was a
baby. The sheer
monstrousness of
it haunts every
waking moment
of my life.”
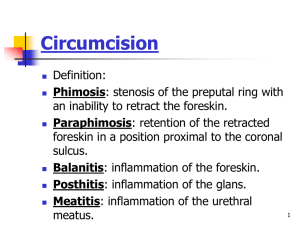
Neonatal Circumcision:
Core statement of the ethical problem
Circumcision is a
non-therapeutic
medically unnecessary
irreversible amputation
of a normal, healthy, functional body part
from a non-consenting person.
“MEDICAL BENEFITS”: A CAVEAT
Pathologizing
the foreskin
MEDICAL JUSTIFICATIONS
A medical-benefits or 'therapeutic' justification requires
that:
1.
benefits sought outweigh the risks and harms
2. only reasonable way to obtain these benefits, and
3. necessary to the well-being of the child.
None of these conditions is fulfilled for routine
infant male circumcision.
If we view a child's foreskin as having a valid function, we are no
more justified in amputating it than any other part of the child's
body unless the operation is medically required treatment and
the least harmful way to provide that treatment.
From: The Ethical Canary: Science, Society, and the Human Spirit, by Margaret Somerville. Toronto, 2000.
Question #1:
Q: Is it ethically acceptable to surgically alter the
natural genitals of a child, when no compelling
therapeutic reason exists?
A: NO
Nontherapeutic newborn circumcision of males
violates all four of the core principals of medical
ethics, and a host of human rights principals.
Circumcision of a child is acceptable only when
medically necessary, and only when conservative
treatment approaches have failed.
PARENTS’ “RIGHTS” vs.
CHILD’S RIGHTS
Parents given wide latitude on childrearing decisions
Children not considered competent to make medical
decisions for themselves
Parents as proxy/surrogate decision-makers
“Best Interests”:
Deciding for Children
Factors in determining “best interests”
Maximizing benefits while minimizing harms
Consider both physical and emotional needs
Least restrictive and least intrusive way to obtain desired benefits
Family’s views and socio-cultural background
Patient’s own ascertainable wishes, feeling, and values
BMA: “… prioritising of options which maximize the patient’s
future opportunities and choices.”
British Medical Association, 2006. The Law & Ethics of Male Circumcision: Guidance for Doctors.
General problems with
proxy consent:
Risk of surrogate making decisions for another based on
their own concerns and values.
Surrogate has no intrinsic motivation to fully consider the
impact of a medical decision made for another.
Surrogates do not always make the decisions that their
wards would have chosen, esp. with elective interventions
Problems with pediatric
proxy consent
Parents do not own the child, rather guardians.
Proxy consent
Appropriate for cases of actual medical need.
Not valid for non-therapeutic procedures?
The child is the patient:
“Pediatric health providers… have legal and ethical duties
to their child patients to render competent medical care
based on what the patient needs, not what someone
else expresses.”
AAP Ethics Committee, 1995. Informed consent, parental permission and assent in pediatric
practice.
AAP Circumcision Position
Statement, 1999: Ethics Section
“In cases such as the decision to perform a
circumcision in the neonatal period, when there are
potential benefits and risks and the procedure is
not essential to the child’s current well-being, it
should be the parents who determine what is in
the best interests of the child.”
No mention of the rights of the child.
However…
AAP Proxy Consent statement, 1995
“Parents should not exclude children and adolescents
from decision-making without persuasive reasons.”
“A patient’s reluctance or refusal to assent should carry
considerable weight when the proposed intervention
is not essential to his or her welfare and/or
can be deferred without substantial risk.”
AAP (1995). Informed consent, parental permission, and assent in pediatric practice.
Compare AAP to…
Royal Dutch Medical Association, 2010
“Insofar as there are medical benefits, it is reasonable to put
off circumcision until the age at which such a risk is relevant
and the boy himself can decide about the intervention, or
can opt for any available alternatives.”
“Non-therapeutic circumcision of male minors is contrary to
the rule that minors may only be exposed to medical
treatments if illness or abnormalities are present, or if it
can be convincingly demonstrated that the medical
intervention is in the interest of the child…”
“Non-therapeutic circumcision of male minors conflicts with
the child’s right to autonomy and physical integrity.”
Royal Dutch Medical Association (KNMG), 2010. Non-therapeutic Circumcision of Male Minors.
ETHICS SUMMARY: Cultural comparisons
x
Child as stakeholder
x
x
x
x
Ethical problems acknowledged
x
x
x
x
Legal problems acknowledged
x
x
x
x
x
Conscientious objection
acknowledged
Comparison to FGM
x
x
x
USA
(AAFP) 1999
x
USA
(AAP) 2002
British Columbia
(CPSBC) 2009
x
Canada
(CPS) 2002
United Kingdom
(BMA) 2006
Parents’ choice
Australia / NZ
(RACP) 2010
Netherlands
(KNMG) 2010
ETHICS IN MEDICAL ORG POSITION STATEMENTS
x
x
Question #2:
Q: Who is the appropriate person to give
permission for elective, nontherapeutic cutting
of anyone’s genitals?
A: The owner of the penis, i.e. the male
himself, when he is old enough to give his
own informed, voluntary consent.
No ethical problem with circumcision of
consenting, adequately informed adults.
PARENTS’ VOICES
“If only ONCE
someone had
mentioned that it
wasn’t medically
necessary...
I know I
would have
questioned it.
But no one did…”
“It was an assault
on him, and on
some level it was
an assault on me…
I will go to my
grave hearing that
horrible wail…”
“I really, honestly, don't
think I will ever forgive
myself for letting this
happen to him.”
PARENTS’ VOICES:
“If only I had known …”
That it would affect breastfeeding.
That it would look so gruesome.
That it would affect the sensitivity of the penis.
That the foreskin had a purpose.
That there is a risk of death.
That I might possibly regret it so seriously.
Never thought that he might not want
to be circumcised.
INFORMED CONSENT
The patient’s right to agree to, or refuse, a proposed
medical intervention, based on an adequate
understanding of the implications of his decision
Ethical foundation:
Respect for the self-determining dignity of the
individual
Practical purpose:
Supports the patient’s interest in rational decisionmaking through access to information
The Elements of
Valid Informed Consent
Competence
Voluntariness
Informed
Understanding
DISCLOSURE: Required content
Nature of the health problem
Nature of the proposed procedure
Benefits
Risks
Alternatives
The more elective the proposed procedure,
the higher the level of disclosure required
“The process of informed consent
for circumcision is inadequate.”*
PROCESS:
Practitioners’ survey:
Nearly half of those who performed circs did not discuss before birth
Of those who performed circs and provided prenatal care, 26% did not
discuss before birth
Mothers’ survey:
29% discussed with OB before birth, 28% discussed with pediatrician
25% (up to 37% in other surveys) reported they did not receive enough
info to make their decision about circumcision
CONTENT:
No info given on the alternative of not circumcising
* Ciesielski-Carlucci C, Milliken N, Cohen NH. Determinants of decision making for circumcision.
Camb Q Healthc Ethics 1996;5:228-236.
Inadequate Disclosure: COMPLICATIONS
Surveys of disclosure of complications
Parents typically informed only of risks of pain, infection,
bleeding.
60+% do not mention possibility of damage to other parts of
the penis
92% do not mention death
Christensen-Szalanski JJ, Boyce WT, Harrell H, Gardner MM. Circumcision and informed consent: Is
more information always better? Med Care 1987; 25(9):856-867.
Fletcher C R. Circumcision in America in 1998: Attitudes, beliefs, and charges of American physicians. In:
Male and female circumcision: Medical, legal, and ethical considerations in pediatric practice . New York:
Kluwer Academic/Plenum Publishers, 1999.
Inadequate Disclosure: ALTERNATIVES
Longley (2009): Content analysis of parent circumcision
info handouts for content on the alternative of not
circumcising.
Content found relevant to topic of not circumcising:
Anatomy, protective function, sexual function
Care and development of intact penis
Framing of intact penile hygiene
Counter-information given for medical and social claims
Ethics of neonatal circumcision
Circumcision not practiced in most societies
Normalizing terms
Adequacy of disclosure on alternative
of not circumcising (max. score = 12)
12
Average Adequacy Score
10
8
6
4
2
0
Average
Adequacy Score
Pro-circ
N=1
N Am med
orgs N = 6
N Am misc
N = 33
Austr/NZ
N=7
Anti-circ
N=8
1.50
3.83
4.56
6.71
10.31
Inadequate Disclosure: FRAMING
FRAMING:
How a story is told affects how the information is perceived.
E.g. Relative risk vs. absolute risk
E.g. Negatively framed messages on intact hygiene
E.g. Omission of relevant information
Framing constitutes informational manipulation.
.
Violates disclosure and voluntariness standards of valid
informed consent.
Informed Consent for Neonatal
Circumcision: A CAVEAT
Proper informed consent does not make
circumcision of children ethical.
However:
It gives parents the opportunity to make a truly
informed decision.
It forces health professionals to themselves be
more informed.
HEALTH PROFESSIONALS’ VOICES
“I did not become a nurse
to hurt babies. In 1992, I gave
notice to my employers that I
would no longer be an
accomplice in the atrocity
that is infant circumcision.
I have reclaimed
my tattered soul and
begun the process of
becoming whole
again.”
CONSCIENTIOUS OBJECTION
“Doctors are under no obligation to comply
with a request to circumcise a child.”
Right to conscientious objection acknowledged by:
British Medical Association
Royal Australasian College of Physicians and Surgeons
College of Physicians and Surgeons of British Columbia
Doctors Opposing Circumcision
Barriers to conscientious objection:
Lack of education among health professionals
Lack of ethical leadership by AAP
Lack of institutional support
Fear of losing patients
Fear of inconveniencing colleagues
Fear of sticking one’s neck out
Other ethical issues:
Inadequate pain relief
Physicians soliciting for unnecessary surgery
Commercial use of amputated foreskin tissue
Religious rights vs. child’s rights
And others….
The Ethics of Neonatal Circumcision:
Problems and Pathways to a more ethical future
“Ethics points us
to corrective vision,
i.e. to question practices
that have become routine,
or which we take for
granted.”
- College of Physicians and Surgeons of British Columbia, 2009.
THE END