iv and blood transfusions
advertisement

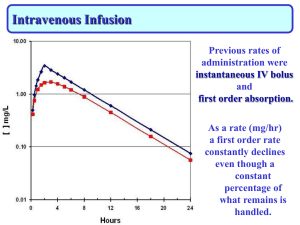
Principles Of Intravenous Infusions And Blood Transfusions Sharon Harvey Definition of an Intravenous Infusion The term intravenous can be described as administering a solution into or within a vein The term infusion is defined as a slow injection of a substance into a vein or subcutaneous tissue Advantages of using an intravenous route An immediate therapeutic effect is achieved due to a rapid delivery of the drug/fluid to target sites Pain and irritation caused by some substances when given intra muscularly or subcutaneously if patient cannot tolerate drug by oral route Disadvantages of using the intravenous route The inability to recall the drug Insufficient control of administration may lead to speed shock Additional complications such as microbial contamination (intrinsic or extrinsic) Vascular irritation - chemical Phlebitis Drug incompatibilities Some drugs cannot be absorbed by any other route A better control is offered over the rate of administration IN ORDER TO ADMINISTER FLUIDS OR DRUGS SAFELY The nurse must have: knowledge of the solutions Their effects and side effects The factors that affect flow The complications that can occur Gravity flow devices Gravity infusion devices depend on gravity to drive the infusion. The system consists of an administration set containing a drip chamber and utilizing a roller clamp to control flow which is measured by counting the drops Gravity infusions are ideal for infusing fluids which do not need to be infused with absolute precision Factors That Influence Flow Rates. The composition, viscosity and concentration of the fluid affect flow e.g. An infusion of cold blood will result in venospasm and impede the flow rate IV fluids run by gravity and any changes in their height will alter the flow rate. Any changes in patient position can also alter the flow rate Flow Rates Can Also Be Affected by the Following: The condition and size of the patients vein e.G. Phlebitis can reduce the lumen size and reduce flow The gauge of the cannula/catheter The position of the device within the vein, if it is up against the vein wall The site of the vascular access. The flow may be affected by limb position such as the elbow joint Kinking, pinching or compression of the cannula of the administration set may cause rate variation Occlusion of the device due to clot formation which may result from a BP cuff on the infusion arm, or with the patient lying on the side of the infusion. The patient - The dangers Patients occasionally adjust the control clamp or other parts of the delivery system! Pumps today have tamper proof features (Jensen 1995) Positioning of the patient will affect the flow and patients should be instructed to keep the arm lower than the infusion on a gravity device (Dolan 1999) Complication of inadequate flow control Fluid overload with accompanying electrolyte imbalance Metabolic disturbances Toxic concentrations of medication resulting in speed shock Air embolism due to containers running dry before expected. An increase in venous conmplication such as a chemical phlebitis caused by reduced dilution of irritant substances e.g potassium. Complications associated with under infusion Dehydration Metabolic disturbances A delay response to medications or below the therapeutic dose Occlusion of a cannula due to a cessation of flow. CLIENT GROUPS ASSOCIATED WITH FLOW CONTROL PROBLEMS: INFANTS AND YOUNG CHILDREN THE OLDER PERSON PATIENTS WITH COMPROMISED CARDIOVASCULAR STATUS PATIENTS WITH IMPAIRMENT OR FAILURE OF ORGANS PATIENTS WITH MAJOR SEPSIS PATIENTS SUFFERING WITH SHOCK WHATEVER THE CAUSE POST-OPERATIVE OR POST TRAUMA PATIENTS PATIENTS RECEIVING MULTIPLE MEDICATIONS WHOSE CLINICAL STATUS COULD CHANGE RAPIDLY Calculating flow rate Flow rate is calculated using a formula that requires the following information: The volume to be infused, the number of hours the infusion is running over and the drop rate of the administration set. Volume to be infused x drop rate Time in hours x 60mins =drops in minutes Infusion Device Definitions An infusion device is designed to deliver measured amounts of drug or fluid either intravenously or subcutaneously over a period of time. This is set at an appropriate rate to achieve the desired therapeutic response and prevent complications. (Mallet & Bailey 1996) Types of infusion pumps – Drip rate pumps: These were the first infusion pumps which controlled the rate of drop formation using a standard gravity set – Volumetric pump: This works by calculating the volume delivered. This is achieved when the pump measures the volume displaced in the reservoir. It calculates that every fill and empty cycle of the reservoir delivers the given amount of solution Aims of Intravenous Infusions devices. The aims of using an infusion device is to ensure the delivery of a drug or fluid to a patient at a constant rate over a set period of time with no adjustments to “catch up” This is not only to ensure a therapeutic response but also to avoid complications of over and under infusion The use of infusion devices both mechanical and electronic has increased the level of safety in IV therapy. However, the equipment is only as good as the person who is selecting and setting up! Advantages and disadvantages of infusion pumps – The disadvantages are that these are usually relatively expensive and dedicated administrations sets are required. Use of a wrong set could result in error even if the pump appears to work – These pumps are able to overcome resistance to flow by increasing delivery pressure and do not rely on gravity – Some are also complicated to set up which can lead to error Additional guidelines the infusion container should hang no longer than 24 hrs. This is reduced to 8 hrs for blood and blood products. Recent research indicates that changing sets every 48 - 72 hrs is not associated with increased infection rates and can result in considerable saving (department of health) It is desirable to record the date and time that the set is due to be changed The site of the infusion should be inspected every shift for complications such as infiltration or inflammation Dressings should be changed every 24 hrs or if it appears to be dirty or loose It is desirable to record the date and time that the set is due to be changed The site of the infusion should be inspected every shift for complications such as infiltration or inflammation Dressings should be changed every 24 hrs or if it appears to be dirty or loose. The dead space in the equipment has also been identified as a reservoir for micro-organisms which may be released into the circulation (Weinbaum 1987) Objectives of transfusion Increase circulating blood volume after surgery, trauma or haemorrhage To increase the number of red blood cells and aid haemoglobin maintenance Provide cellular components as replacement therapy Further recommendations in the light of recent research have shown that a closed system of infusion is maintained whenever possible This reduces the risk of extrinsic bacterial contamination Principles of blood transfusions Blood replacement or transfusion is the iv administration of whole blood or blood product such as plasma, packed red blood cells or platelets. Blood groups and types The determination of blood groups is based on the presence or absence of A and B red cell antigen The most important grouping for transfusion purpose is the ABO system, which includes A,B,O,AB blood types The Rh factor Other considerations when matching for blood transusions is the Rh factor, which is an antigenic substance in the erythrocyte of most people A person with the factor is Rh positive and a person without the factor is Rh negative Blood transfusions Transfusing blood or blood products is a nursing procedure. The nurse is responsible for the assessment before, during and after the transfusion and for regulation of the transfusion. Assessment is critical because of the risk of allergic reactions Guideline Checks To ensure that the right client receives the correct type of blood or blood product a thorough procedure is used to check the identity of the blood or blood product, the compatibility of the blood and the client Two registered nurses must check the label on the blood product against the clients identification number, blood Because of the dangers of a reaction it is very important to follow guidelines for the correct policy of administration The nurse must obtain the patients baseline vital signs before the transfusion begins as this allows the nurse to determine when changes in vital signs occur, which indicates a transfusion reaction occurring The expiry date on the blood is also checked Even if a minor discrepancy exists the blood should not be given and blood bank notified immediately Initiation of the transfusion begins slowly to allow for early detection of a reaction The rate of transfusion is usually specified by the doctor Ideally a unit of whole blood or packed red blood cells is transfused over 24hours. Beyond 4 hours there is a risk of the blood becoming contaminated Throughout the infusion the nurse monitors periodically for side effects, and assesses vital signs, and records all findings A reaction to the blood will usually occur in the first 15 mins. If a reaction is anticipated the nurse will obtain vital signs more frequently The rate of transfusion is usually specified by the doctor Ideally a unit of whole blood or packed red blood cells is transfused over 24hours. Beyond 4 hours there is a risk of the blood becoming contaminated Transfusion reactions and nursing interventions A transfusion reaction is a systemic response by the body to incompatible blood Blood transfusion reactions are life threatening, but prompt nursing intervention can maintain the clients physiological stability If a blood reaction is suspected the nurse stops the infusion immediately The line is kept open by the infusion of 0.9% saline solution The doctor is informed immediately The nurse remains with the patient monitoring their vital signs as often as every 5 mins The nurse prepares to administer emergency drugs I.e. antihistamines/adrenaline etc and if needed to perform CPR The blood containers, giving set, labels, form etc are retained and returned to blood bank for further investigation Summary – The nurse is responsible for the administration of intravenous fluids by the methods listed. In order to do this he/she requires a thorough knowledge of the principles, and their application, and a responsible attitude – The nurse must also be able to justify any actions taken and be prepared to be accountable for the action taken(UKCC 1992)