Glomerulonephritis
advertisement

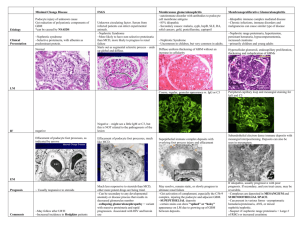
Orange Urine on Halloween Eva Delgado, MD Morning Report Overview Case Presentation Indications for Referral/Admission Work-up based on Differential Discussion of Pathophysiology Treatment and Prognosis Take Home Points Case Presentation 12 y/o F with OCD develops “orange” urine with sediment. PMD advises watchful waiting. Case Presentation Orange urine persists x 4 days, so mom makes appointment with PMD. PMD notes elevated BP, weight gain, and then orders one key test……….. URINALYSIS: + hematuria, + proteinuria A Word on Urinalysis UA with >/= 5 RBC/hpf on 3 samples over several weeks = HEMATURIA Only UA can distinguish between confounders: Myoglobin, hemoglobin, toxins, foods/coloring Massengill, Peds In Review, 2008 A Word on Disposition Hematuria AND proteinuria Proteinuria may be due to notable hematuria, BUT.. Combination of both increases risk of renal disease Hypertension Can be a symptom of fluid overload warranting diuresis and further observation PMD sends patient to the ED….. Boineau and Lewy, Peds in Review, 1989. Simckes and Spitzer, Ped in Review, 1995. Physical Exam in ED Wt 60kg (↑ over last 6 mos) VS: T 36.4, P 68, BP 146/80, R 20, 100% O2 Gen: no distress HEENT: no peri-orbital edema, MMM Chest: CTA b/l CV: RRR, no murmur Abd: soft, NTND Ext: slight erythema in skin folds, no edema Differential and Work-Up Urinalysis Chemistry panel CBC C3, C4 ASO +/- Throat swab Imaging Do you need a biopsy? Thinking of Glomerulonephritis Clues to look for in H&P: Edema, discolored urine (in 30-50%), HTN due to ↓GFR and hypervolemia, oliguria Clues to look for in UA: + hematuria, + proteinuria, + casts (60-85%) RBC dysmorphology implies glomerular damage Sensitivity 95%, specificity 90% McCory, Peds in Review, 1983. Boineau and Lewy, Peds in Review 1989. Glomerulopathy vs. Glomerulonephritis Nephrotic Syndrome Glomerulonephritis Edema R = Red urine (hematuria) Proteinuria O = Oliguria Hypoproteinemia P = Proteinuria Elevated LDL E = Elevated BP, BUN Hypercoagulability (↑fibrinogen, factor V) Low C3 = Post-Strep, Membranoproliferative, SLE Silverstein, Laughing your way to passing the pediatric boards, 2008. Laboratory Results UA: 3+ blood, 2+ protein, 1+ LE, 0 nitrites, 11-20 WBC, numerous RBC, 1-3 granular casts Chemistry: BUN/Cr = 17/0.8 CBC: Hbg 11.3, HCT 32.5, MCV 79 C3: 26 (86-184) C4: 21.5 (20-59) ASO: 2130 (<400 unit/ml); and + Rapid strep Poststreptococcal GN Most common type of Acute GN Usually occurs in 5-15 y/o 50% of cases are asymptomatic Diagnosed by evidence of Group A Strep ASO titers detectable 2-4 weeks s/p pharyngitis Anti-DNase-B titers helpful in post-pyoderma type The Role of Grp A Strep Nephritogenic strains of streptococci Wall protein M12 in pharyngitis, M49 in pyoderma These strains pose ~ 15% risk of PSGN approx 2 weeks after initial infection Antibiotic treatment to prevent GN? Simckes and Spitzer, Peds in Review, 1995. The Role of Grp A Strep PANDAS = Post-infectious Autoimmune Neuropsychiatric Disorders Associated with Streptococcal Infection Syndenham’s Chorea and Rheumatic Fever OCD/Tic disorders shown to emerge or worsen with temporal relation to Grp A Strep infection PANDAS patients may have higher susceptibility to Grp A Strep infection, + family h/o Rheumatic Fever Kurlan et al. 121 (6): 1188. (2008) Pediatrics Considering the DDX of PSGN Low C3 80-90% of PSGN cases have low C3 x 2 mos Also seen in GN due to SLE Consider MPGN if low C3 > 2 mos MPGN can also present after infection MPGN may also low C4 Diagnose by biopsy TRAM-TRACKING Considering DDX of PSGN Normal C3: IgA Nephropathy Alport’s Suspect if recurrent hematuria with URIs/Infections + Family History HUS or HSP can present with gross hematuria Post-viral GN Boineau and Lewy Peds in Review 1989. Treatment of AGN in General Admit if HTN, edema, or signs of renal failure Monitor/correct electrolyte anomalies Treat HTN to avoid sequelae Diuresis loop diuretics like lasix Fluid and salt restriction Anti-hypertensives like the Ca-channel blockers Treatment Specific to PSGN Antibiotics to target Grp A Strep Cultures often positive even if no symptoms, suggesting active infection Treatment may milder course of PSGN Epidemics of Grp A Strep may warrant ppx to prevent PSGN, especially in underdeveloped societies Unclear/controversial role for impact on OCD Rodriguez-Iturbe and Musser, J Am Soc Nephrology, 2008 Prognosis and Sequelae Good prognosis in children CLOSE follow-up! HTN resolves in ~ 1-2 weeks C3 levels return to normal in ~ 6 weeks Gross hematuria resolves in ~ 6 weeks Microscopic hematuria resolves in ~ 1 year Proteinuria resolves in ~ 6 months Progression to renal dysfunction RARE McCrory, Peds in Review 1983. Take Home Points Urinalysis is KEY test to w/u discolored urine UA with casts/dysmorphic RBCs = GN HTN, edema, or renal dysfunction admit Poststrep GN = most common, due to characteristics of Strep and/or patient Treat Strep infection and co-morbidities Guarantee follow-up Works Cited Boineau and Lewy, “Evaluation of Hematuria in Children and Adolescents,” Pediatrics in Review, 1989. Kurlan et al., “Streptococcal Infections and Exacerbations of Childhood Tics and OCD Symptoms: A Prospective Blinded Cohort Study,” Pediatrics 2008. Massengill, “Hematuria,” Pediatrics in Review, 2008. Rodriguez-Iturbe and Musser, “The Current State of Poststreptococcal Glomerulonephritis,” Journal of American Society of Nephrology, 2008. Simckes and Spitzer, “Poststreptococcal Acute Glomerulonephritis,” Pediatrics in Review, 1995. McCrory, “Glomerulonephritis,” Pediatrics in Review, 1983.