Diagnosis and Treatment - Alport Syndrome Foundation
advertisement

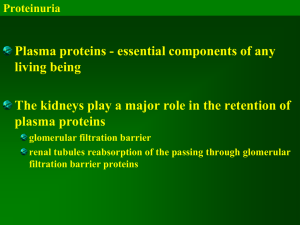
Alport Syndrome – Diagnosis and Treatment Christoph Licht The Hospital for Sick Children, Toronto, ON Alport Syndrome Family Conference 2012 Minneapolis, MN - 21.-22.7.2012 The challenge Alport syndrome: A disease progressing to ESKD Phase IV Phase III Phase II Phase I Proteinuria Hematuria ESRD ↓ Renal Fx Proteinuria Hematuria Hematuria Specific Disease Progression with Age/Time Birth Late childhood Early adolescence Adulthood Figure 1. Mechanisms underlying the activation of inflammatory and fibrogenic pathways in proximal tubular epithelial cells by ultrafiltered protein load Abbate, M. et al. J Am Soc Nephrol 2006;17:2974-2984 Copyright ©2006 American Society of Nephrology Alport Syndrome: Current therapeutic approaches in humans and animal models Gross and Kashtan, Kidney Int 2009 COL4a3 knockout mice • COL4a3 knock out-mice • From week 4 From week 6 From week 7 At about 10 weeks Hematuria Proteinuria Nephrotic syndrome Death from renal failure • In vivo model for Alport syndrome • In vivo model for chronic proteinuric CKD Cosgrove et al, Genes Dev 1996 Increased lifespan by ACE inhibitor treatment No treatment (Placebo) ACE-inhibitor treatment: - Late: from week 7 (proteinuria) - Early short: week 4-10 (hematuria) - Early long: from week 4 (hematuria) until death Gross et al, Kidney Int 2003 AT1 receptor blockers: Less efficient than ACE inhibitors No treatment (Placebo) Treatment: o Ramipril (ACEinhibitor) from week 4 o Candesartan (AT1antagonist) from week 4 Gross et al, Nephrol Dial Transplant 2004 RAAS blockade in pediatric AS patients A Tale of Two Trials Webb NJ et al. NDT. 2011 • Multicenter, randomized, doubleblind study of losartan versus placebo or amlodipine • 30 children, ℞ for 12 weeks • Significant in proteinuria • No safety concerns, increase in creatinine or hyperkalemia Gross O et al. Kidney Int. 2012 • European Alport Registry • 283 patients (109 received no ℞) over 20 years • 3 groups with respect to commencement of ACE ℞ : o Onset of microalbuminuria o Proteinuria >0.3 g/day or o CKD stage III and IV Survival benefit with therapy Gross et al, Kidney Int 2012 Start therapy early In sibling pairs where the elder sibling had invariably been started on ℞ much later Median age of starting renal replacement was 27 years, while it was delayed until a median age of 40 in the younger child. Gross et al, Kidney Int 2012 Time to ESKD delayed with therapy RRT delayed 3 years in CKD group & 18 years in proteinuric group Proteinuria reduced in all More sustained if ℞ started prior to CKD stage III-IV Gross et al, Kidney Int 2012 Initiation of ACE inhibitors and/or ARBs at the onset of overt proteinuria to prolong renal survival and delay the need for renal replacement therapy ACE inhibition should be first-line ARB or aldosterone inhibition second-line agents Aldosterone inhibition • Increasing evidence that aldosterone inhibition has a reliable blood pressure- independent, antiproteinuric effect in adult studies • Remains to be proven to translate to an improvement in GFR Navaneethan et al, Clin J Am Soc Nephrol 2009 Aldosterone inhibition • Spironolactone is known to be relatively safe in the pediatric setting • May offer renoprotection in CKD patients, especially if exhibiting the phenomenon of ‘aldosterone breakthrough’ • Escape trial - Proteinuria decreased by 50% but gradually rebounded Ku et al, Pediatr Nephrol 2009 Wühl et al, Kidney Int 2004 Aldosterone inhibition in Alport Syndrome • Only pediatric study of aldosterone inhibition in kidney disease involved 5 Alport patients o persistent proteinuria despite ACE inhibition or ACE/ARB in combination • Significant improvement in proteinuria achieved & maintained for at least 18 months • eGFR remained unchanged, lower BP (no ill effect), tendency to hyperkalemia (never exceeded 5 mmol/L) Kaito et al, Pediatr Nephrol 2006 Aldosterone inhibition in Alport Syndrome Kaito et al, Pediatr Nephrol 2006 Telmisartan – ARB with benefits Telmisartan • Second generation ARB • Renoprotective and antiproteinuric effects due to its agonistic effect on the PPAR receptor • Reduce oxidative stress and inflammation • Improved endothelial & vascular function • Meta-analysis of clinical trials involving 25,425 patients confirmed antiproteinuric effect and can delay progression of proteinuria Destro et al, Expert Opin Pharmacother 2011 Zhang et al, J Mol Endocrinol 2012 Kusunoki et al, Hypertension 2012 PPAR • Peroxisome-proliferator-activated-receptor (PPAR) - nuclear receptor that regulates gene transcription • Expressed & upregulated in injured podocytes • Thiazolidinediones - ligands for PPAR developed for the management of insulin resistance o Reduce proteinuria o Activate PPAR & directly increase nephrin gene transcription thus restoring slit diaphragm integrity o Decrease apoptosis of podocytes Yang HC et al. Kidney Int 2006 Benigni A et al. J Am Soc Nephrol 2006 Summary and Perspectives • RAAS inhibition via ACEIs and ARBs is safe and effective in children • Early therapeutic intervention seems to be key for … - delaying (preventing?) ESKD - improving quality of life • International registries and treatment trials in children are needed focusing on safety, efficacy and cost saving of early therapy