UNIVERSAL NEWBORN SCREENING FOR SCID
advertisement

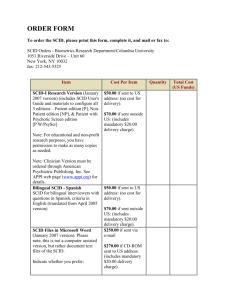
UNIVERSAL NEWBORN SCREENING FOR SCID DR. PETER VICKERS WHAT IS IT? Newborn screening for SCID is a test that takes place immediately after birth to ascertain whether or not a newborn child has SCID. It would be done at the same time as screening for PKU (phenylketonuria) automatically take place. Phenylketonuria (PKU) is a rare genetic condition that is present from birth. The body is unable to break down a substance called phenylalanine, which builds up in the blood and brain. A sample of blood would be taken from a heel prick (as with PKU) and sent to a laboratory for testing HOW IS IT TESTED? Once in the lab, a polymerase chain reaction (PCR) assay is conducted of the blood spot from the heel prick performed after birth. The test uses a TREC (T-cell receptor excision circle) assay. This simple test has transformed the possibilities of early detection/diagnosis of SCID TRECs are a surrogate marker for the number of naïve T cells. TRECs are reduced in all forms of severe T cell lymphopaenia (SCID and others). WHY? Early diagnosis of SCID is critical because of the very high risks of infection and death within a few weeks/months of birth. It is a rare disease (prevalence 1:50,000 – 1:100,000 – but this is only a guess because of the poor rate of diagnosis). The baby appears normal at birth, and there are usually no signs or symptoms until after a few months, by which time it may be too late. Early treatment (usually haematopoietic stem cell transplantation – HSCT) decreases morality rates. Therefore, the ability to detect a case of SCID through newborn screening (NBS) is, at the moment, the ideal method that we currently possess which allows us to detect children with SCID with virtually no delay. However, there are financial and ethical considerations that have to be addressed before such screening takes place. Is it cost effective? Will it harm the child? Is the pain caused by the heel prick a bar to this particular screening for SCID, given the rarity of the condition? What about false positives and the effects on the child and family? EXPERIENCES We have some knowledge and experience of NBS for SCID in the USA, where many states have already set up this screening. The costs have been worked out at between 5-6 dollars per screening of one child. However, this has to be set against the cost of treating just one child with SCID who may be diagnosed after a few months – which are enormous Interestingly, there have been no reported cases of SCID in Wisconsin that had not been identified by NBS Current Implementation Status (2012) Number of States Shading Status 9 Statewide and Fully Implemented 2 Selected Populations 9 Pilots and/or Screening Planned for 2012 27 Not Implemented 4 Pilots and/or Screening Planned for 2013 FLORIDA NEWBORN SCREENING ALGORITHM for SEVERE COMBINED IMMUNE DEFICIENCY (SCID) Initial TREC Assay SCID-I-01-LOW SCID-I-01-NORM No Repeat TREC with β-Actin Yes TREC >40 NORMAL Full or Preterm TREC ≤ 5 β-Actin >5,000 Full term TREC >5-25 β-Actin >10,000 Full term TREC >25-40 β-Actin >10,000 Full or Pre-term TREC ≤ 5 β-Actin ≤5,000 Full term TREC >5-25 β-Actin ≤10,000 Full term TREC >25-40 β-Actin ≤10,000 Pre-term TREC >5-25 β-Actin >10,000 Pre-term TREC >5-25 β-Actin ≤10,000 Pre-term TREC >25-40 β-Actin >10,000 Pre-term TREC >25-40 β-Actin ≤10,000 Full or Pre-term TREC >40 Presumptive Positive Presumptive Positive Previous Borderline Inconclusive Inconclusive Inconclusive Low Inconclusive Low Inconclusive NORMAL SCID-C-01-INC SCID-C-03-INC SCID-C-06-INC SCID-C-02-LOW SCID-C-04-INC SCID-C-05-LOW SCID-C-07-INC SCID-C-01-NORM SCID-C-01-ABNR SCID-C-02-ABNR Yes Borderline Report to CMS for follow-up (via Patient Care) SCID-C-02-BORD No Borderline SCID-C-01-BORD β-Actin – serves as amplification control TREC – T-lymphocyte receptor excision circle Full term – baby’s age of gestation (AOG) is ≥37 weeks Pre-term – baby’s AOG is <37 weeks Presumptive Positive – determination used for possible SCID, SCID variants, or T-cell lymphopenias Inconclusive – determination used when amplification control (β-Actin) is below the acceptable limit and/or baby is pre-term (<37 weeks AOG) TREC and β-Actin cutoff values may change after the validation period Jojo Dy 05-15-2012 Request for a repeat specimen (Baby’s age must be equivalent to ≥37 wks. of gestation) What is the likelihood that the referral is going to be a true SCID? Sensitivity is 100% (so far none have been missed) False positives<0.1% NY (recent data – 2 years) – 475,713 screened, incidence 1/42,000; 0.1% referred for Flow FL likely get 5 – 10 SCID cases per year Referrals will be about 40 per year (across 3 centers) Clinic Nurse Manager Role Alert on-call (inpatient) fellow and attending of referral Contact family and inform them of abnormal newborn screen for SCID Set up confirmatory testing (T, B, NK cell enumeration) Must be done within 2 working days of the referral Discuss precautions until diagnosis is made Make appointment with immunologist Attempt schedule first with the provider - if not available any full time attending can see patient Must be seen within 5 working days of the referral Every template has a ‘hidden/emergency slot’ – open access for new patient evaluation for these referral (can be seen M-F) Contact PMD Keep open line of communication during this follow up process Keep log of patients and contact Note that this is the protocol for just one site in the USA THE POSITION IN THE UK Despite the experiences and information obtainable from the USA, the UK National Screening Committee decided that they had to get their own proof that this was the way to go. Invitations sent out to interested groups to submit consultation form for consideration. INGID was a part of this consultation, and had to consider a whole range of criteria, including: The condition should be an important health problem The epidemiology and natural history of the condition, including development from latent to declared disease, should be adequately understood, and there should be a detectable risk factor, disease marker, latent period or early symptomatic stage. There should be simple, safe, precise and validated screening test. The test should be acceptable to the population. There should be an effective treatment or intervention for patients identified through early detection, with evidence of early treatment leading to better outcomes than late treatment. The benefits from the screening programme should outweigh the physical and psychological harm (caused by the test, diagnostic procedures and treatment. The costs of the screening programme should be economically balanced in relation to expenditure on medical care. All other options for managing the condition should have been considered to ensure that no more cist effective interventions could be introduced. Public pressure for widening the eligibility criteria for reducing the screening interval and for increasing the sensitivity of the testing process should be anticipated – decisions about these parameters should be scientifically justifiable to the public. NBS for SCIDS has also picked up many other PIDDs Classic SCID 13. AK2 (Reticular dysgenesis) 1. IL2RG (common g chain SCID); X linked 14. ADA (Adenosine deaminase SCID) 2. JAK3 15. PNP (Purine nucleoside 3. IL7 Ra 4. RAG1 5. RAG2 phosphorylase SCID) 16. WHN (Winged-helix-nude SCID) 17. Unknown Variant SCID/ Leaky SCID 6. DCLRE1C (Artemis SCID) 1. NHEJ1 (Cernunnos/ XLF) 7. PRKDC (DNA-PKcs SCID) 2. AK2 8. LIG4 (DNA Ligase IV SCID) 3. PNP 9. CD3D (CD3δ SCID) 4. WHN 5. RAG1 10. CD3E (CD3ε SCID) 6. RAG2 11. CD3Z (CD3ζ SCID) 7. ADA 12. PTPRC (CD45 SCID) 8. IL2RG 9. IL7Ra 10. LIG4 11. DCLRE1C 12. CHD7 (CHARGE syndrome) 13. RMRP (Cartilage Hair Hypoplasia) 14. CORO1A (Coronin-1A) 15. Unknown Non-SCID 1. DiGeorge syndrome (del22q11.2; ~ >35 genes) 2. CHD7 3. ORA1 4. STIM1 5. CD3G (CD3γ SCID) 6. ZAP70 (primarily affecting CD8 T cell development) 7. LCK (p56lck) 8. MHC class II deficiency (CIITA, RFXANK, RFX5, RFXAP) 9. RMRP 10. Hoyeraal-Hreidarsson syndrome, HHS (DKC1, TERT, TINF2, DCLRE1B) 11. SLC46A1 (Hereditary folate metabolism, HFM); reversible SCID 12. ATM (Ataxia telangiectasia) 13. RAC2 14. Down Syndrome (Trisomy 21) 15. Jacobsen syndrome (del 11q) 16. Lymphopenia of prematurity 17. Idiopathic T cell lymphopenia 18. Unknown Now over to you to think about and discuss: What are the ethical considerations to consider? What about false positives? What about the effects and arrangements in all maternity units for this screening to take place – cost, staffing, emotional effects, etc. What about the financial costs? Thank you for your attention References & Further Reading Chase, et al (2011) Newborn screening for SCID: three years of experience. Annals of the NewYork Academy of Sciences, November; 1238 (99-105) Kelly, et al (2013) Screening for severe combined immunodeficiency in neonates. Clinical Epidemiology 3:5 (363-369)