Recovery of anesthesia
advertisement

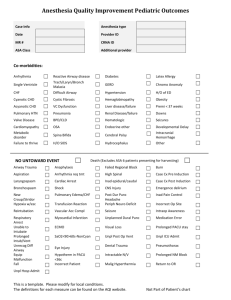
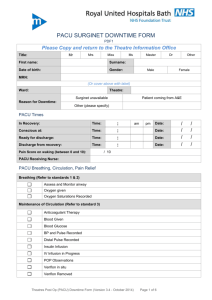
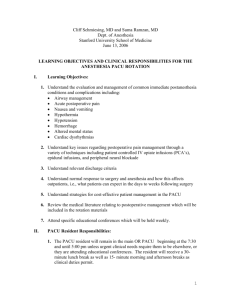
RECOVERY FROM ANAESTHESIA Sanaa Farag Wasfy Lecturer of anaesthesia and intensive care * Recovery is a continual process, the early stages of which overlap the end of intraoperative care. * Patients cannot be considered fully recovered until they have returned to their preoperative phsiological state. -The entire process may last many days Divided into three phases : 1- Early recovering (awaking and recovery of vital reflexes) 2- Intermediate recovery (immediate clinical recovery and home readiness) 3- Late recovery(full recovery and psycholgical recovery). Early recovery commences on discontinuation of anesthetic agent, which allows the patient to awaken, recover protective airway reflexes, and resume motor activity. It traditionaly continues in postanesthsia care unit (PACU). Patients are likely to begin responding to verbal stimuli when alveolar anesthetic concentrations are decreased to about 0.5 MAC for the volatile anesthetic drug (MAC awake) if unimpeded by other factors. Increased ventilation results in a more rapid decline in alveolar anesthetic concentration which hastens recovery, provided that the arterial carbon dioxide pressure is not so low that it diminshes cerebral blood flow and the removal of aneshetic agent from the brain. Recovery from neuromuscular blockade may be monitored by peripheral nerve stimulation and by clinical indices. Recovery from intravenous opioids and hypnotics may be more variable and difficult to quantify than recovery from inhalation and neuromuscular blocking agents. Transport Transport from the operating room is usually complicated by the lack of adequate monitors, access to drugs, or resuscitative equipment. Patients should not leave the operating room unless they have a stable and patent airway, have adequate ventilation and oxygenation, and are hemodynamically stable. All patients should be taken to the PACU on a bed that can be placed in either the head down or head up position. PACU The PACU should be located near the operating rooms. A central location in the operating room area, Proximity to radiographic, laboratory, and other intensive care facilities on the same floor is also highly desirable. A ratio of 1.5 beds per operating room is customary. Every effort should be made to diminish unnecessary noise in PACU. The PACU should be staffed only by nurses specifically trained in the care of patients emerging from anesthesia. They should have expertise in airway management and advanced cardiac life support as well as problems commonly encountered in surgical patients relating to wound care, drainage catheters, and post operative bleeding. The nurse-to-patient ratio is 1:1 for sick patients and 1:2 or 1:3 for routine cases. Monitoring Vital signs should be recorded at least every 15 minutes and recorded on a separate sheet. The patient is encouraged by the nurse to cough, breathe deeply, and change body position. The most important monitor is a well informed and skilled person; with immediate access to anaesthetic assistance. Technical support is important but sophisticated electronic monitors are not universally essential Postanaesthesia care problems 1) Pain. 2) PONV. 3) Agitation. 4) Croup. 5) Sore-throat. 6) Headache. 7) Shivering. 8) Increased body temperature. 9) Cardiovascular. 10) Respiratory. Discharge Scores determines when patients are fit for discharge from PACU, various criteria for readiness for discharge from PACUs have been established. The modified Aldrete score is the most common system used. A score> or = 9 is required for discharge. Postaesthesia discharge scoring system(PADSS) determines home readiness and the optimal length a patient stays after day-case surgery. Scoring system must be practical, simple, easy to remember, and not place additional burden on personnel. Fast track recovery It is the ability to transfer suitably recovered patients from the OR directly to the phase II recovery area, by passing the most costly PACU. Children derive an additional benefit from fast tracking in that they are more quickly reunited with their parents. To institute successful fast tracking programs, it is necessary to modify anesthetic techniques and to use the newer shorter acting anesthetics, narcotics and muscle relaxants. Modified aldretes scoring system may not be adequate after day case procedures because it fails to consider common side effects as pain nausea and vomiting, therefore a new fast track scoring system that incorporates both has been proposed. Delayed recovery It is delayed return of level of conscious. There are several causes: metabolic and electrolytes. Cerebral hypoperfusion. Cerebral depression by drugs. Summary 1. Immediate recovery from anaesthesia is a concept of care during not just a place to put the patient after surgery. Responsibility can never be fully delegated by the anaesthetist to others. 2. Most problems relate to Airway, Breathing and/or Circulation; with delayed return of consciousness and inadequate analgesia being other common related issues. All these should be anticipated. 3. Facilities required are the same as those necessary for anaesthesia where-ever that might be administered. If such facilities cannot be duplicated in a separate location, then the safest place to recover patients is in the operating room. 4. The most important monitor is a well informed and skilled person; with immediate access to anaesthetic assistance. Technical support is important but sophisticated electronic monitors are not universally essential 5. Discharge to a general ward should only be considered when you have a conscious, cooperative and comfortable patient who is well oxygenated and well perfused; and likely to remain so. THANK YOU