Composites Handout

Superior Aesthetics
Composite Layering vs Composite
Veneers
Munther Sulieman
Aesthetic Treatments
• Smile analysis
• Recontouring
• Whitening
• Micro/macro-abrasion
• Composite bonding
• Veneers
• Crowns
Factors affecting tooth shade
• Degree of polish
• Thickness of enamel
• Enamel morphology
• Fluorescence and translucency
• Dehydration
• Recession and dentinal exposure
• Intrinsic, extrinsic or internalised stain
Causes of Tooth Discolouration
• Intrinsic Discolouration
• Extrinsic Discolouration
• Internalised Discolouration
Intrinsic tooth staining causes
• METABOLIC
• Alkaptonuria
• Congenital erythropoietic porphyria
• Congenital hyperbilirubinaemia
• Rickets, Ehlers- Danlos syndrome
• etc.
Intrinsic tooth staining causes
• INHERITED
• Amelogenesis imperfecta
• Dentinogenesis imperfecta
• Dentinal dysplasias
Intrinsic tooth staining causes
• IATROGENIC
• Tetracycline stains
• Fluorosis
Fluorosis Staining
Caused by an interference with the calcification process of the enamel matrix which results in incomplete maturation accompanied with opacity and or porosity
Wide range of severity: mottled teeth- minor
(intermittent white flecking or spots) to severe manifestation that involves pitting and brownish surface stains
Only affects superficial enamel thickness usually
Intrinsic tooth staining causes
• TRAUMATIC
• Enamel hypoplasia
• Pulpal haemorrhage products
• Root resorption
• AGEING
• Teeth become darker, more yellow and slightly more red
Haemorrhagic discoloration
Rupture of blood vessels and extravasation of erythrocytes into the dentinal tubules which gives the tooth a pink hue but the tooth may still remain vital
Majority of post endo discoloration is caused by failure to completely remove blood or other organic material from the pulp chamber.
Pastes/ restorations: corrosion products from silver amalgam in dentinal tubules, silver in sealing pastes or zinc oxide eugenol- blue grey discoloration at cervical area
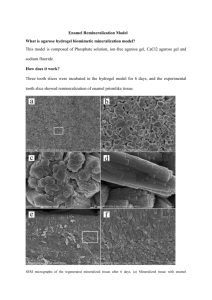
Enamel Hypomineralisation
Developmental disturbance in the formation of the inorganic component of enamel during amelogenesis- results in brown enamel, white opacities or enamel coloration defects of various hues.
Defects can be localised to one section or an entire surface of the tooth with coloured streaks, multiple spots or other patterns
Intrinsic tooth staining causes
• Idiopathic
• MIH: Molar Incisor
Hypomineralisation
Root Resorption
Extrinsic tooth staining-direct
• Tobacco products
• Tea, coffee and red wine
• Spices
• Vegetables
• Medicines
• Plaque
Extrinsic tooth staining-indirect
• CATIONIC ANTISEPTICS
• Chlorhexidine
• CPC
• Hexetidine
• OTHERS eg. Listerine
Internalised stains
• TRAUMA
• cracks
• loss of enamel
• recession
• CARIES
• RESTORATIONS
Enamel Decalcification
Lesions are acquired: occur when dental plaque persists undisturbed on enamel surface producing organic acids that etch the mineral content out of the enamel surface
Left undisturbed further leads to dental decay
If intercepted early, there is no need for restorations
Common sites for these lesions are cervical margins of teeth or around orthodontic brackets with poor
OH.
Tooth discolouration
• Regardless of the nature of the discolouration
Must decide whether the discolouration is confined to the superficial enamel thickness or in the deep dentine layers
This determines the complexity and extent of treatment as well as the absolute choice of treatment
Tooth discolouration
Treatment Options
1. Bleaching: Vital and Non-vital
2.
Enamel microabrasion
3. Direct composite veneers
4.
Indirect veneers (Porcelain/ Composite)
5.
Bleaching with indirect or direct veneers
Bleaching Options
• Vital
• Home
CP / HP -trays
• In-surgery
15-50% HP ± heat / light activation
35% CP waiting room
• OTC
Strips / Paint-on
• Other
Toothpaste Mouthrinse Chewing gum
• Non-Vital
Walking
HP,Perborate/HP, CP
Inside / Outside
CP
In-surgery
35% HP
Bleaching Indications
• Generalised staining
• Ageing
• Smoking and dietary stains
• Fluorosis
• Tetracycline staining
• Traumatic pulpal changes
• Aesthetics pre or post restorative
Bleaching Contraindications
Patients high expectations
Decay and periapical lesions
Patient can’t tolerate taste
Pre existing Conditions
Crowns
Extensive restorative dentistry: Composite and porcelain restorations
Major cracks
Exposed dentine
Pre existing problem sensitivity
Highly translucent tooth
Pregnancy
No scientific evidence against bleaching but there may be a psychological effect on mother
Bleaching may exacerbate pregnancy gingivitis
Treatment of White Fluorosis
Intensity, Location and Depth of lesion will determine Tx
Bleaching of background (reduce contrast between white spot and rest of tooth)
Micro-abrasion of foreground with or without bleaching
Bleaching/abrasion and composites
Composite Veneers
Where Why and When Does
Composite Work?
• Biocompatibility
• Adhesion to Enamel and Dentine
• Colour Perception Optical Effects
• Harmonious Blending with Tooth structure
• Multiple Uses
27
Main problems in handling composite
• Stickiness
• Surface wetting
• Surface smoothness
• Homogeneity
• Adaptation
• Individualization of texture and shape
• Internal air bubbles and wetting defects
28
Freehand technique - problems
•
Aesthetic impression/expression
•
Anatomical form
2
•
Modelling incisal edges 3
•
Surface texture 4
•
Mammelons
5
•
Ridgeline contour
• layer
6
Control thickness of enamel
1
7
7
4
5
3
2
1
6
© Mario Besek
Direct Composite Veneers
Primary indications
White spot lesions
Severe fluorosis
Severe hypoplasia
All these discolorations are usually confined entirely to the enamel thickness and never extend into the dentine
Heavily restored stained anterior teeth
Direct Composite Veneers
• Advantages
• More conservative- no enamel removal!
• One session no lab costs
• Easier shade match compared to single porcelain veneer involving a lab especially if mock-up is used
Direct Composite Veneers
Only cut tooth tissue if absolutely necessary and then only into enamel
Consider air abrasion and bonding composite to reshape teeth
Mock-up may be needed to check contour and shade if patient agreement is deemed necessary
Shade match prior to tooth dehydration
Matching adjacent tooth roughness and texture greatly enhances appearance
Restoration of anterior teeth
• For small class IV and III cavities- centripetal approach (build up from inside to outside)
• For large class IV and incisal build up- buccolingual approach used in conjunction with silicone index
Natural Layering Technique
“The Clinical Procedure”
• Finishing & Polishing- aim is to re-create texture and gloss.
• Surface re-contouring with fine diamonds while discs are best for plane and convex surfaces.
• Smooth out concavities/uneven surfaces with fine diamonds or silicone points
• Fine shine best with hard polishing brushes
Polishing
• PC- Proximal contact
• BLP- Bucco-lingual profile
• TL- Transitional lines
• SM- Surface morphology
• IE- Incisal edge
COMPONEER
● are polymerized, prefabricated enamel shaded composite laminates
● is a direct Composite-Veneering-System
● simplify the freehand technique
● increases the quality of front teeth restorations
● is an economical system
36
Componeer thickness
● Minimal or no preparation due to the minimal thickness of composit laminates of 0.3 mm.
● Ceramic veneers have a minimum thickness of 0.5 – 0.8 mm
Contour guide
● Optimal form selection using the translucent, high-contrast contour guide
38
Properties & advantages
● High opalescence and natural blue effect of the enamel
● High flexure strength E-modulus similar to tooth
39
Form - shape - texture - surface - gloss
40
Properties & advantages
● Highest adhesion composite - composite, optimized by the microretentive surface (2 µm)
©
Componeer erosion 2µm
© Mario Besek
Properties & advantages
• Soaked for 1 week in water at 37 ° C
• 240‘000 cycles, 49N
• 600 x 5 ° / 55 °
• Cresylblue, 24h
• 80 specimen
• 74 showed no penetration
• 6 showed some slight discoloration
Prof.Dr. Ivo Krejci, University of Geneva
Simple individualization
43
Properties & advantages
● Optimized marginal quality - less polymerization stress
44
Advantages
• Extended indications
• Less objective & subjective limits
• Conservative Procedure
• Good Longevity /Repair
• Cost effectiveness
45
Componeer Clinical Procedure
• Choose correct size
• Choose correct shade
• Isolation of teeth
• Preparation small shallow chamfer/interporoximal conditioning
• Re check size and adjust componeer with possible try in
• Etch Bond Cure tooth
Componeer Clinical Procedure
• Place and adapt composite on tooth
• Bond but don’t cure Componeer, place composite and adapt on Componeer
• Fit first Componeer on tooth and firmly push into position
• Clean excess before curing
• Trim and polish
Indirect Porcelain or Composite Veneers
Indicated for conservative treatment of anterior teeth that are;
• Relatively intact
• Worn
• Discoloured
• Misaligned
• Malformed
Indirect Porcelain or Composite Veneers
• Porcelain
• High aesthetics
• Excellent gingival tissue response
• Relatively minimal labial reduction
• Durable and fracture resistant
• Shine through problem
(Blue grey)
• Composite
• High aesthetics
• Excellent gingival response
• More conservative
• Can be repaired if fractured
• Shine through problem
(Blue grey)
Porcelain Veneers
Types of preparation: depends on shade of discoloured tooth, its position and alignment and presence of restorations
Minimal: surface reduction just to bond to enamel
Conventional: 0.3mm reduction cervically, 0.5mm centrally within enamel and retain incisal edge or reduce by 1mm. Keep contacts!
Deep: 0.6mm reduction into dentine and removal of contact points