Management of Patients
With Intestinal and Rectal
Disorders
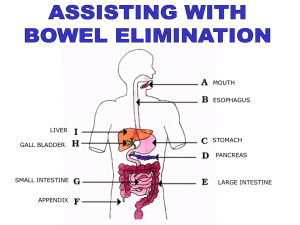
Basic Anatomy
of Intestines
• Small Intestine
– 3 regions: duodenum, jejunum, ileum
• Large Intestine
– Cecum, appendix, colon, rectum, anal canal
– Appendix is attached to the cecum
Basic Anatomy
of Intestines
Basic Anatomy
of Intestines
Basic Anatomy
of Intestines
Basic Anatomy
of Intestines
Basic Anatomy
of Intestines
Bowel Elimination
•
•
•
•
•
Feces moved by peristalsis
Defecation reflex
Sigmoid colon contracts
Anal sphincter relaxes
Valsalva maneuver expels feces
Topics to Consider for Health
History of a Problem Bowel
•
•
•
•
•
•
•
•
•
•
Onset of problem
Characteristics and course
Severity
Precipitating and relieving factors
Cramping
Bleeding increased constipation
Recent travel outside the U.S.
Any changes in activities of daily living
Diarrhea
Constipation
Physical Assessment of
Bowel Integrity and Function
•
•
•
•
•
Auscultation of bowel sounds
Rectal exam
Anal exam
Exam of stool
Palpation (do last)
Altered Intestinal Function
•
•
•
•
Abdominal Assessment
Inguinal Assessment
Perianal Assessment
Fecal Assessment
Constipation
• Abnormal infrequency or irregularity of
defecation; any variation from normal habits may
be a problem.
• Causes include medications, chronic laxative use,
weakness, immobility, fatigue, inability to
increase intra-abdominal pressure, diet, ignoring
urge to defecate, and lack of regular exercise.
• Increased risk in older age.
• Perceived constipation: a subjective problem in
which the person’s elimination pattern is not
consistent with what he or she believes is normal.
Manifestations
•
•
•
•
•
•
•
•
•
Fewer than 3 BMs per week
Abdominal distention
Decreased appetite
Headache
Fatigue
Indigestion
A sensation of incomplete evacuation
Straining at stool
Elimination of small-volume, hard, dry stools
Complications
•
•
•
•
•
Hypertension
Fecal impaction
Hemorrhoids
Fissures
Megacolon
Diagnostic Findings
• Pt Hx
• Physical examination
• Barium enema or sigmiodscopy (to id is it from
spasm or narrowing of the bowel)
• Anorectal manometry ( to id malfunction of the
sphincter)
• Defecography
• Pelvic floor MRI
Bowel Disorder
Medications
• Laxatives
– Fibercon, Bran, Citrucel, Metamucil
– Nursing Responsibilities
• Mix agent with at least 6 oz of water just prior to administering
• Do not administer to clients with possible stool impaction or
obstruction
– Client and Family Teaching
• Client should drink at least 6-8 glasses of fluid daily
• Agents may be mixed with fruit juice, water or milk
• Do not take at bedtime
Patient Learning Needs
•
•
•
•
•
•
•
See Chart 38-1
Normal variations of bowel patterns
Establishment of normal pattern
Dietary fiber and fluid intake
Responding to the urge to defecate
Exercise and activity
Laxative use (see Table 38-1)
Diarrhea
• Increased frequency of bowel movements (more
than 3 per day), increase amount of stool (more
than 200 g per day), and altered consistency (i.e.,
looseness) of stool.
• Usually associated with urgency, perianal
discomfort, incontinence, or a combination of
these factors.
• May be acute or chronic.
• Causes include infections, medications, tube
feeding formulas, metabolic and endocrine
disorders, and various disease processes.
Manifestations
• Increased frequency and fluid content of
stools
• Abdominal cramps
• Distention
• Borborygmus
• Painful spasmodic contractions of the anus
• Tenesmus
Bowel Disorder
Medications
• Antidiarrheal Medications
– Kaopectate, Donnagel, Pepto-Bismol
– Nursing Responsibilities
• Administer on empty stomach
• Assess for potential contraindications
– Client and Family Teaching
• Do not use for more than one week unless specified
• Take in the morning
Complications
• Fluid and electrolyte imbalances
• Dehydration
• Cardiac dysrhythmias
Patient Learning Needs
•
•
•
•
•
•
•
•
Recognition of need for medical treatment
Rest
Diet and fluid intake
Avoid irritating foods—caffeine, carbonated beverages, very hot and cold
foods
Perianal skin care
Medications
May need to avoid milk, fat, whole grains, fresh fruit, and vegetables
Lactose intolerance (see Chart 38-2)
Selected Diets
• Diarrhea
– Oral fluids, glucose electrolyte balanced
(Gatorade, Pedialyte) for bowel rest
– Soft foods after 24 hours
– Add milk products and fat last
• Constipation
– High fiber (vegetable, raw fruits) to bulk up the
stool mass
– Reduce intake of refined foods and meats
Inflammatory Bowel Syndrome (IBS)
• Functional disorders of intestinal motility
• No known cause, usually hereditary factor,
psychological stress, depression and anxiety, diet
high in fat and stimulating or irritating food,
alcohol consumption and smoking.
• More common in women than in men
• In it the peristaltic waves are affected at specific
segments & the intensity of propel the fecal
pattern, no evidence of inflammation or tissue
changes in intestinal mucosa
• C\M: Alteration in bowel pattern (primary symptoms)
constipation or diarrhea or mixing of both, abdominal
pain ( ↑ with eating & ↓ with defecation) , bloating, abd
distension
• Diagnosis: Stool studies, contrast X-ray, Barium enema,
colonoscopy, proctoscopy, manometry, electromyography
• Medical management: Restrict food and then
reintroduction of foods is important to determine type of
food that is irritating (beans, caffeinated products, fried
food, alcohol, spicy food)
• Stress reduction techniques
• Manage diarrhea and constipation
• Nursing management: Nurse should educate
family and patient about the importance of good
dietary habits, chewing food slowly and eat
regularly, not taking fluid with meal since it may
cause abd destination, discouraged alcohol and
smoking.
Selected Diets
• IBS
– May benefit from high fiber diet
– Adding bran and fluid reduces incidence of loose
diarrheal stools and constipated stools
• Gluten Free Diet: prescribed for clients with
sprue
• Low Residue Diet: for clients with ileostomies
and colostomies to prevent blockage.
Diarrhea, Constipation,
IBS, and Fecal Incontinence
• Fecal Incontinence
– Loss of voluntary control of defecation
– Contributing factors included both physiologic and
psychologic
– Diagnosis based on client history and physical
examination of the pelvic floor and anus to
evaluate muscle tone
– Nursing care includes bowel training programs
and other measures to manage fecal incontinence
Appendicitis:
- Appendix is a small, finger-like structure within the abd,
about 10 cm long and attached to the cecum just below
the ileocecal valve
- fills with food and empties into the cecum
- It is prone to obstruction and to infection (appendicitis)
- Common cause of acute abd, and emergency
abdominal surgery
- Occur in all ages but it common between age 10-30
years
Bowel Disorders
• C\M:
- vague epigastric pain or periumblical pain that progress to
the RLQ
- associated with low grade fever, N & V
- loss of appetite
- Localized tenderness at the Mc Burney’s point ( point
between the umbilicus and the anterior superior iliac
spine
- positive rebound tenderness & rovsing sign
- If it rupture pain become more diffuse, with the
development of abdominal distention
- Constipation may occur, so pt not given laxative
•
•
-
Medical management:
Immediate surgery (Appendectomy)
AB pre op
If it perforated drainage is applied to the abscess, then
appendectomy is performed
Nursing management:
Relive pain
Prevent FVD
Reduce anxiety
Prepare the pt for surgery
After surgery place pt in high fowler position or supine with
leg slightly flexed
•
-
-
Give pt opioid analgesic
Give food as tolerated
Teach pt wound care
Instruct pt that he can resume normal physical activity within 2-4wk’
Nursing interventions for patient with complications after
appendectomy:
Peritonitis: observe for abd tenderness, fever, vomiting, abd rigidity
and tachycardia, employ constant NG tube, correct dehydration,
administer antibiotic
Pelvic abscess: evaluate N & V, chills, fever, diaphoresis, diarrhea,
prepare patient for rectal exam and surgical drainage,
Subphrenic abscess (under the diaphragm): evaluate for chills and
fever, prepare x-ray exam, prepare patient for surgical drainage of
abscess.
ileus: assess for bowel sounds, employ NG tube and suction, replace
F& E, prepare for surgery
• Peritonitis:
- An inflammation of the peritoneum, the serous
membrane lining the abd cavity and covering the
viscera.
- Results from bacteria (E.Coli, klebsiella, Proteus&
pseudomonas) or MO from GI disease, in women it
occur from disease of reproductive organ. It can
result from trauma or injury (gunshot, stab wound)
or kidney inflammation.
- Other common causes are: appendicitis, perforated
ulcer, diverticulitis and bowel perforation,
peritoneal dialysis
• C\M:
- Diffuse pain (constant, localized, more intense near the site
of inflammation)
- Tenderness and distention in the affected area
- Rebound tenderness & paralytic ileus
- N&V, increase temp (37.8- 38.3), increase pulse rate
- Diminished peristaltic movement
- Rigid abdominal muscle
- Pain diminished in pt with diabetes (advanced neuropathy,
liver cirrhosis and on analgesic or corticosteroids
Intestinal Obstructions
•
•
•
•
Mechanical obstruction
Functional obstruction
Small bowel
Large bowel
Causes of Intestinal Obstructions
Bowel Disorders
Colostomy
• Is the surgical creation of an opening into the colon ,
allows the drainage of colon content to the out side
the body. It could be temporary or permanent fecal
diversion.
• The consistency of the drainage is related to the
placement of the colostomy.
• Indications : Large bowel obstruction, Colorectal
cancer. The colostomy begins to function 3- 6 days
after surgery.
Ileostomy
• Ileostomy: the surgical creation of an opening into
the ileum or small intestine, is commonly performed
after a total colectomy. It allows for drainage of fecal
matter from ileum to the out side of the body
• The drainage is liquid to unformed and occurs at
frequent intervals.
• Indication: chronic inflammatory bowel disease.
Colorectal Cancer
• The third most common cause of cancer deaths in the
United States.
• Risk factors (see Chart 38-8).
• Importance of screening procedures.
• Manifestations may include change in bowel habits;
blood in stool—occult, tarry, bleeding; tenesmus;
symptoms of obstruction; pain, either abdominal or
rectal, feeling of incomplete evacuation.
• Treatment depends upon the stage of the disease.
Areas Where Cancer Can Occur
Placement of Colostomies
Anorectal Conditions
•
•
•
•
•
Anorectal abscess
Anal fistula
Anal fissure
Hemorrhoids
Pilonidal sinus or cyst
•
•
-
-
Diseases of the Anorectum
Includes: Anorectal abscess, Anal fistula, Anal fissure,
hemorrhoids, pilonidal sinus or cysts.
Anal fissure:
Is a longitudinal tear or ulceration in the lining of the anal
canal
Causes: trauma, persistent tightening of the anal canal from
stress and anxiety (constipation), childbirth, overuse of
laxative
C\M: painful defecation, burning and bleeding during
defecation, bright red on the paper toilet
Rx: dietary modification ( fiber supplement), stool softener,
increase water intake, sitz bath, suppositories with
analgesic, surgery ( lateral internal shpinctretomy with
fissure excision)
-
-
Hemorrhoids
Dilated veins in the anal canal
50 % of people above 50y of age develop hemorrhoids.
Shearing effect on the anal mucosa during defecation
leading to sliding of the anal structure ( hemorrhoidal
and vascular tissue)
Pregnancy may initiate it due to the pressure in the
hemorrhoidal tissue
Classifies as: internal or external
S&S: pain, itching, bright red bleeding with defecation
External: associated with sever pain from inflammation
and edema caused by thrombosis lead to ischemia and
necrosis.
Internal is not painful until they bleed or prolapsed
when they enlarge
Anal Lesions
Bowel Disorders
Pilonidal Sinus
Management:
• avoid strain, hygiene, high-fiber diet, fruit, bran and fluid intake.
• Analgesic, bulk-forming agents such as (Metamucil),, warm
compresses, sitz bath, bed rest allow the engorgement to subside.
• None surgical treatment: infrared photocoagulation, bipolar
diathermy, laser therapy (to affix the mucosa to underling muscle) .
• Surgical treatment: rubber-band Ligation procedure after
anoscope. Can be painful and may cause secondary hemorrhage or
infection.
• Cryosurgical hemorrhoidectomy: freezing the hemorrhoid for
sufficient time to cause necrosis, painless, foul smelling, prolonged
healing, not very common.
• For hemorrhoids with thrombosed vein hemorrhoidectomy is
performed, after surgery small tube inserted through the sphincter
to permit flatus and blood drainage
Nursing Process: The Care of the Patient with an
Anorectal Condition—Assessment
•
•
•
•
•
•
•
Health history
Pruritis, pain, or burning
Elimination patterns
Diet
Exercise and activity
Occupation
Inspection of the area
Nursing Process: The Care of the Patient
with an Anorectal Condition—Diagnoses
•
•
•
•
•
Constipation
Anxiety
Acute pain
Urinary retention
Risk for ineffective therapeutic regimen
management
Collaborative Problems/Potential
Complications
• Hemorrhage
Nursing Process: The Care of the Patient with an
Anorectal Condition—Planning
• Major goals may include adequate elimination
patterns, reduction of anxiety, pain relief,
promotion of urinary elimination,
management of the therapeutic regimen, and
absence of complications.
Interventions
• Encourage intake of at least 2 L water a day
• Recommend high-fiber foods
• Bulk laxatives, stool softeners, and topical
medications
• Promote urinary elimination
• Hygiene and sitz baths
• Monitor for complications
• Teach self-care