Constipation: treatment in
primary care, when to refer
and novel therapies....
Lee Dvorkin
Consultant General , Colorectal & Laparoscopic
Surgeon
Spire Roding Hospital
Department of Surgery – North Middlesex University Hospital
The next 20-30 mins
• An overview
• Primary care management
• cIBS
• Faecal impaction
• When to refer
• Novel therapies
Constipation
• 2nd most common GI symptom
• 3% of population (2 - 34%)
• 1% have intractable symptoms
• Often in combination with FI
Epidemiology and Cost
• Constipation is more common in
–
–
–
–
Women (X3)
> 65 years
Non-whites
Poor socio-economic background
• Most common treatment is laxatives
– 3 million people (USA)
– > $725 million
Constipation
• A subjective term reported by patients when
their bowel habit is perceived to be
abnormal
• Wide variety of symptoms
• Objective criteria now exist
• Rome II (Thompson et al., 1999)
Rome II Criteria
•
At least 12 weeks in the preceding 12 months, of 2 or
more of the following
–
–
–
–
straining in > 25 % defaecations
hard stools in >25 % defaecations
incomplete evacuation in >25 % defaecations
anorectal obstruction / blockage in >25 %
defaecations
– digitation >25 % defaecations
– <3 defaecations / week
Specialists
~25%
consulters
Primary care
~75%
non-consulters
~70%
female
~30%
male
Constipation: Aetiology
Aetiology
Primary (bowel problem)
Structural
Functional
Colon or rectum
Secondary (systemic)
Drugs and Diet
Endocrine
Metabolic
Neurological
“Primary” Constipation
• Structural
Cancer
Strictures
Megacolon/rectum
Hirschsprung’s
Idiopathic
Outlet obstruction
Anal stenosis
Rectocele
Prolapse
Functional
c- IBS
Colonic inertia
Iatrogenic (post pelvic
surgery)
Evacuatory dysfunction
Rectal hyposensitivity
Anismus
Proctalgia fugax
‘anal fixators’
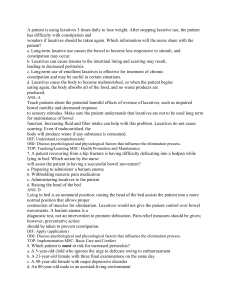
Treatment: functional constipation
Vast majority don’t need referral or Ix unless no
response to simple measures
Treatment focussed on underlying cause....
–
–
–
–
–
–
Combination of softener and stimulant
High fibre for slow transit
Suppositories for evacuatory dysfunction
Colonic Irrigation
Bowel retraining / Biofeedback
Novel therapies including surgery
cIBS treatment
•
•
•
•
•
•
Stress relief
Hypnosis/Yoga
Mebeverine 135mg tds before meals
Laxatives (avoid lactulose)
Antidepressants (avoid constipating ones)
Diet-wheat exclusion, reduce fibre
Faecal Impaction
• PR
• Elderly, immobile
patients
• No red flag
symptoms
• Treat with enemas
then reassess
Bowel-retraining programme
• Package of care
• Psychosocial counselling
• Optimisation of medication / diet/laxatives
• Pelvic floor co-ordination exercises
• ‘Biofeedback’ techniques
Pelvic floor co-ordination
exercises
•
•
•
•
•
Posture
Diaphragmatic breathing
Abdominal bracing exercises
Balloon expulsion
Splinting
‘Biofeedback’
• Physiological
parameter
(sphincter
pressure) displayed on a screen visible to
the patient
• Patients are re-educated, and learn how to
co-ordinate the activity of the pelvic floor
and anal sphincters
Novel therapies
Colectomy/Proctocolectomy for
constipation
• Poor results
• High complication rates
• Rectal and small bowel dysmotility reduces
effectiveness of colectomy
• Even stoma unsatisfactory but good results
in selected few
ACE
• Good results esp. with
neurological disease
• Intubate stoma with
water or osmotic
laxative
• High stoma
complication rate
Prucalopride
•
•
•
•
NICE approved
Women only
Failed 2 different laxatives after 6 months
If no response after 4 weeks unlikely to
work
• Selective serotonin agonists leads to colonic
motility (1-2mg od)
Sacral Nerve Stimulation
• Stimulation of S3
• “neuromodulation” effect on ascending
pathways, local autonomic system
– Locally (sphincter pressures, rectal
sensation)
– Distant (gut motility)
• 2 stage procedure
– Trial period 3 weeks
– Permanent implant
Indications
• Constipation
– not NICE approved
– Largest study to date, Kamm et al 2010, Gut.
– Sig improvement in no of defecations, straining,
incomplete emptying and abdo pain
– Used in both slow transit and obst defecation
– Difficult to achieve complete resolution of symptoms
SNS: Problems
• Expensive
– Test box £200, Lead £2000, Battery £8000
• Post operative problems
– Infection, nerve damage, battery lasts 6-8 years
• Loss of efficacy over time
– Requires regular “re-programming”
• Pregnancy
– Must be switched off during pregnancy
– c-section to avoid lead displacement
Posterior Tibial Nerve Stimulation
• 2003 used for FI
• Neuromodulation of
sacral plexus via the
posterior tibial nerve
• Achieved by
– Percutaneous
– transcutaneous
PTNS- Indications
• Just FI, so far
• Studies in constipated patients awaited
PTNS
• Cheap equipment costs
– Needles £200
– Pads £3
– Stimulator boxes £80
Conclusions
• Simple therapies often effective
• Tailor treatment to underlying
pathophysiology
• Refer to exclude underlying disease or if
simple measures ineffective
• Avoid surgery!