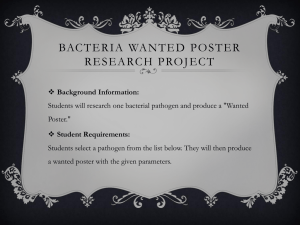
Streptococcus anginosus as a Culprit of Osteomyelitis: A Review of 11 Cases
Tristan Timbrook, BA, Allen T. Griffin, MD, Julie Harting, Pharm.D, and Diana Christensen, MD
Division of Infectious Diseases, University of Louisville
ABSTRACT
INTRODUCTION (Cont’d)
RESULTS (Cont’d)
Discussion
Background: The Streptococcus anginosus group is comprised of
three species of bacteria that are loosely classified within the viridans
streptococci. Like other viridans streptococci, the anginosus group has
a penchant to create hematogenous complications by adhering to
damaged endovasculature and prosthetic devices. Quite distinct,
however, is the proclivity for abscess formation. While a variety of sites
in the human body claim anginosus as an etiologic agent of infection,
osteomyelitis is unusual, particularly when not originating
hematogenously. The objective of the present study was to describe a
series of 11 patients with osteomyelitis due to Streptococcus anginosus
in terms of demographics, comorbidities, anatomic site of infection,
laboratory values, and outcomes.
abscess.7 As a sequela of hematogenous dissemination, S. anginosus
has been found occasionally to infect the cervical8 and lumbar
spines9,10 as well as the iliac11 and femur bones.12 Finally, isolated
cases of contiguous osteomyelitis in the setting of prosthetic
material13,14 and a diabetic foot infection15 have been described. Given
that S. anginosus as an etiology of osteomyelitis has been infrequently
reported, the objective of the present study was to describe a series of
patients with osteomyelitis due to S. anginosus in terms of
demographics, comorbidities, anatomic site of infection, laboratory
values, and course.
Seventy-five percent of these cases were complicated by abscess
formation while S. anginosus bacteremia was present in 30%. All
anginosus isolates were sensitive to penicillin and vancomycin (Table
1). Common coinfecting pathogens were Prevotella species (42%),
Bacteroides fragilis (25%), and methicillin-resistant Staphylococcus
aureus (25%).
The present study documents 11 cases of osteomyelitis due to the S.
anginosus group. Illustrated herein is the difficulty in treating this group
in the setting of osteomyelitis in terms of the need for prolonged
treatment ( > 10 weeks), the need for extensive debridement (> 3
surgeries on average), even amputation, and the propensity for
abscess formation and bacteremia. This study is unique given the
limited literature describing the phenomenon of S. anginosus
osteomyelitis. Despite the virulence illustrated here with this group of
bacteria, penicillin still appears to be an effective antibiotic against
these pathogens.
Methods: We reviewed our database of skin, soft tissue infections, and
osteomyelitis for cases of osteomyelitis caused by Streptococcus
anginosus. Cases were excluded from review if no bone infections
were documented. Data collected and described included patient age,
comorbidities, anatomic site of infection, route of infection
(hematogenous versus contiguous), inflammatory markers, confecting
pathogens, susceptibility pattern of the anginosus isolate, length of
treatment, and need for amputation.
Results: Eleven patients with osteomyelitis due to Streptococcus
anginosus were identified. All cases arose from a contiguous anatomic
site, with the exception of one case that was hematogenous. Five
instances were related to foot osteomyelitis while three, two, and one
case, respectively, were related to mandibular, cranial, and vertebral
osteomyelitis. Seventy-five percent of patients had associated abscess
formation. All required extensive debridement with an average of three
surgeries (SD=2.8) per patient to control infection. The mean length of
antibiotic treatment was 11 weeks (SD=7.4). All anginosus isolates
were sensitive to penicillin.
Conclusions: Osteomyelitis due to Streptococcus anginosus is rarely
reported. Our case series illustrates the proclivity of Streptococcus
anginosus for associated abscess formation in the context of
osteomyelitis, the need for multiple debridements to control infection,
and the importance of prolonged treatment.
MATERIALS AND METHODS
Study Design
This study was retrospective review of osteomyelitis cases in our
database at the University of Louisville hospital in Louisville, KY.
Instances of S. anginosus osteomyelitis were selected from 300
patients entered into the database from June 1, 2010 to August 1,
2012.
Inclusion Criteria:
• 18 years of age or older
• Confirmed diagnosis of osteomyelitis
Exclusion Criteria:
• S. anginosus not identified as an infecting organism
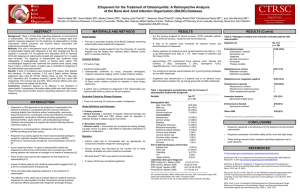
Categories of data collected in the osteomyelitis database and used for
analysis were age, sex, comorbidities, site of infection, route of
infection (contiguous or hematogenous), laboratory data, S. anginosus
minimal inhibitory concentrations (MIC) (Table 1), presence of
orthopedic hardware, presence of abscess formation, presence of S.
anginosus bacteremia, coinfecting pathogens, and patient course.
Factors included in patient course included length of antibiotic
treatment, number of surgeries, and requirement for amputation.
Statistics:
Data were analyzed descriptively in terms of number (percentages),
means, and standard deviations.
INTRODUCTION
RESULTS
The Streptocococcus anginosus (S. anginosus) group includes three
species of bacteria which are classified within the viridans
streptococci.1 Similar to other viridans streptococci, the anginosus
group often spreads hematogenously, adhering to damaged
endovasculature and prosthetic devices, causing complications.
Uniquely, S. anginosus has a propensity to form visceral abscesses.2
Incidence of osteomyelitis as a result of this group of organisms is quite
uncommon. In a review of 186 cases of S. anginosus infection, for
example, only a single case of bone infection was documented.3 Both
the pediatric4,5 and adult literature6 have elucidated the rare finding of
S. anginosus as an agent of cranial osteomyelitis due to abscess
extension from the paranasal sinuses while other literature has
documented the occurrence of mandibular osteomyelitis related to
contiguous spread from an oral
Eleven patients with osteomyelitis due to the S. anginosus group were
identified. All 11 cases arose from a contiguous anatomic site, with the
exception of a single case of hematogenous vertebral osteomyelitis
that developed subsequent to gynecologic surgery. In addition to the
case of vertebral osteomyelitis, five instances were related to foot
osteomyelitis in the context of a progressive diabetic foot ulcer while
there were three cases of mandibular osteomyelitis associated with
tooth decay, bisphosphonate usage and radiation exposure, or
radiation exposure alone, respectively. Finally, two instances of postsurgical cranial osteomyelitis due to S. anginosus were identified. The
most common comorbidities in these patients were diabetes mellitus,
hypertension, peripheral arterial disease, and peripheral neuropathy
(Table 1).
The average length of treatment was 10.9 weeks (SD=7.4). Each
patient required an average of three surgeries (SD=2.8) to fully debride
infected tissue. Four of the five foot osteomyelitis cases required
partial amputations of the foot while one of the cranial osteomyelitis
cases required the entire skull cap to be removed. No patients died.
All patients were treated with intravenous therapy. The most common
antibiotic utilized was penicillin G in dosages ranging from 24 to 30
million units per day.
Future research needs to better characterize S. anginosus outcomes in
the setting of osteomyelitis and other infections in terms of straintyping, minimal inhibitory concentrations, and serum bactericidal levels.
CONCLUSION
Table 1. Demographic and laboratory data for 11 cases of osteomyelitis related to
Streptococcus anginosus.ª
N=11
(No./%)
______________________________________________________________________
Demographic data
Age, Mean (SD)
54.8 (13.9)
Male Sex
7 (63.6)
Comorbidities
Hypertension
Diabetes
Smoking
Peripheral arterial disease
Peripheral neuropathy
Coronary artery disease
Cancer
Chronic renal disease
COPD
Bisphosphonate usage
Cirrhosis
8 (72.7)
6 (54.5)
6 (54.5)
5 (45.5)
4 (36.4)
2 (18.2)
2 (18.2)
1 (9.1)
1 (9.1)
1 (9.1)
0 (0)
Route of Infection
Arising contiguously
Arising hematogenously
10 (90.9)
1 (9.1)
Site of Infection
Diabetic foot
Mandible
Cranium
Vertebrae
5 (45.5)
3 (27.3)
2 (18.2)
1 (9.1)
Laboratory
WBC (cells/mm³), Mean (SD)
ESR (mm/hr), Mean (SD)
CRP (mg/dl), Mean (SD)
Procalcitonin (ng/ml), Mean (SD)
16.4 (5.9)
75.8 (50.4)
11.5 (10.5)
2.8 (3.5)
S. anginosus MIC
Penicillin, Mean (SD)
0.05 (0.03)
Vancomycin, Mean (SD)
0.81 (0.24)
______________________________________________________________________
ªAll values are given as No. (%) unless otherwise specified. SD, standard deviation;
COPD, chronic obstructive pulmonary disease; WBC, white blood cell count; ESR,
erythrocyte sedimentation rate; CRP, C-reactive protein; procalcitonin; MIC, minimal
inhibitory concentration.
In conclusion, the present study documents cases of osteomyelitis due
to S. anginosus and illustrates the virulence of this pathogen in terms
of the tendency to produce bacteremia and abscess formation in the
setting of osteomyelitis. Furthermore, the importance of prolonged
treatment and need for extensive debridement are illustrated.
REFERENCES
1. Mandell Bennett, Dolin (eds.). Mandell, Douglas, and Bennett's Principles and Practice
of Infectious Diseases. 2010 (7th ed.); Elsevier.
2. Jacobs JA, Pietersen HG, Stobberingh EE, et al. Bacteremia involving the
"Streptococcus milleri" group: analysis of 19 cases. Clin Infect Dis 1994;19(4):704-3.
3. Singh KP, Morris A, Lang SD, et al. Clinically significant Streptococcus anginosus
(Streptococcus milleri) infections: a review of 186 cases. N Z Med J
1988;101(859):813-6.
4. Karaman E, Hacizade Y, Isildak H, et al. Pott's puffy tumor. J Craniofac Surg
2008;19(6):1694-7.
5. Han JK, Kerschner JE. Streptococcus milleri: an organism for head and neck infections
and abscess. Arch Otolaryngol Head Neck Surg 2001;127(6):650-4.
6. Bannon PD, McCormack RF. Pott's puffy tumor and epidural abscess arising from
pansinusitis. J Emerg Med 2011;41(6):616-22.
7. Coman G, Pânzaru C, Diculencu D, et al. Pyogenic infections with different locations
caused by Streptococcus anginosus alone or in association with anaerobic bacteria.
Rev Med Chir Soc Med Nat Iasi. 1995;99(3-4):215-9.
8. Fabie F, Arrue P, Thorn-Kany M, et al. Cervical spine infection with Streptococcus
anginosus. Case report. Neurochirurgie 1999;45(5):417-21.
9. Faraj A, Krishna M, Mehdian SM. Cauda equina syndrome secondary to lumbar
spondylodiscitis caused by Streptococcus milleri. Eur Spine J. 1996;5(2):134-6.
10. Barham NJ, Flint J, Mifsud RP. Osteomyelitis complicating Streptococcus milleri
Endocarditis. Postgrad Med J 1990;66:314-5.
11. Calza L, Manfredi R, Briganti E, et al. Iliac osteomyelitis and gluteal muscle abscess
caused by Streptococcus intermedius. J. Med Microbiol 2001;50:480-2.
12. Archibald LK, Harrelson JM, Reller LB. Osteomyelitis of the femur complicating
Streptococcus milleri endocarditis. Orthopedics 2005;28(7):707-8.
13. Dronda F, Bach A. Osteomyelitis around a knee prosthesis due to Streptococcus
anginosus. Rev Clin Esp 1992;190(5):284-5.
14. Gil-Garay E, Fernandez-Baillo N, Martinez-Pineiro L. Osteomyelitis of the pubic
symphysis due to Streptococcus anginosus. A case report. Int Orthop 1993;17(1):51-3.
15. Shlaes DM, Lerner PI, Wolinsky E, et al. Infections due to Lancefield group and related
Streptococci (S. milleri, S.anginosus). Medicine.1981;60(3):197-207.