Gastric Outlet Obstruction
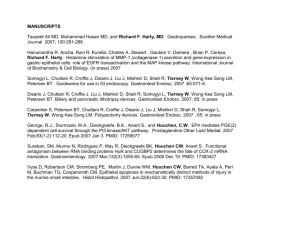
advertisement
Clinical Case Conference November 30, 2011 Karen A. Chachu CC: Epigastric abdominal pain • HPI: 49yo F with PMH of alcohol abuse, GERD, p/w 3 days sharp abdominal pain radiating to her back. • 1st presentation: She was initially seen in Presby ED with c/o epigastric abdominal pain and nausea. Received zofran IV, morphine IV, CT scan. She was told there was an abnormality on her abdominal CT and sent home with a “To Go Pack” of 4 percocet. She was supposed to see her PCP on 4 days later but no-showed. • . CC: Epigastric abdominal pain • HPI: 49yo F with PMH of alcohol abuse, GERD, p/w 3 days sharp abdominal pain radiating to her back. • 1st presentation: She was initially seen in Presby ED with c/o abdominal pain. Received zofran IV, morphine IV, CT scan. She was told there was an abnormality on her abdominal CT and sent home with a “To Go Pack” of 4 percocet. She was supposed to see her PCP on 4 days later but no-showed. • 2nd presentation: 3 weeks later p/w ongoing abd pain & coffee ground emesis DOA. Abd pain not relieved by Aleve, Tylenol or Percocet. Pain worsened by food, but not by EtOH. Emesis 2x daily for 3 weeks, involuntary and self-induced due to sense of early satiety. Night PTA, had 1st episode of blood tinged emesis, previously non-bloody, non-bilious. Denies melena, hematochezia, dysphagia, odynophagia, diarrhea, LH, dizziness. • PMH/PSH – Asthma – Tracheostomy placement & decannulation in setting of laryngeal injury after assault – Chronic shoulder pain – Alcohol abuse • FamHx: NC • SocHx: – ½ ppD cig x 20 years – 6 pack beers daily – Quit cocaine 1-2 years ago • Meds: – albuterol inhaler prn • Allergies: • ROS: otw neg – ACE inhibitors angioedema – methadone Vitals: T 98, BP 124/71, P 108, RR 18, O2Sat 98% on RA Exam: Gen: NAD HEENT: NCAT, anicteric, MMM, supple CV: Tachy Lungs: CTAB Abd: soft, epigastric & RUQ ttp. No r/g Ext: no LE edema Neuro: A&Ox3, NF Rectal: melena NGL: Coffee grounds which cleared after ~500ml. No frank blood. Labs BMP: K 3.3 CBC: Hgb 7.5 (baseline 9-10), had been 11.8 3 weeks ago; platelets 111, MCV 111 AST 75, ALT 38 Amylase 152, lipase 73 INR 1.0 Albumin 2.7 Plan: IVF, morphine IV, PPI gtt Octreotide gtt Ceftriaxone 1g IV x1 Banana bag 2U pRBC CT A/P with IV contrast 1. Wall thickening in the pylorus and the filling defect in the first part of the duodenum concerning for mass or polyp. The filling defect described in the duodenum is soft tissue in density but has an atypical configuration for a duodenal mass. However this could represent a polyp from the stomach that has prolapsed into the duodenum . 2. Hepatomegaly without obvious hepatic metastases. 3. Diverticulosis coli without diverticulitis. 4. Gallbladder is collapsed. The spleen, pancreas, adrenal glands, kidneys, bladder, uterus, and adnexae are unremarkable. The vasculature shows scattered atherosclerotic calcifications. EGD: No esophageal or gastric varices. Ulcerated duodenal mass without clear active bleeding. Pathology DUODENAL MASS: • Duodenal mucosa with mild villous blunting and expansion of lamina propria with chronic inflammatory cells. Superficial fragments of gastric type mucosa with mild chronic inflammation. • Fibrinopurulent exudate mixed with bacterial colonies and fungal organism (yeast form) present. • No dysplasia seen. • This biopsy may not represent the mass lesion seen endoscopically. Rebiopsy is recommended if clinical indicated. What should be the next step in management? Next… • Discharged home with PPI po BID • Plan repeat EGD as out patient …6 weeks later EGD: Pylorus was ulcerated and strictured. The scope could not be advanced beyond the pyloric channel. Therefore, attempted to dilate the area using a 10mm-12mm TTS balloon. Even following dilation was unable to advance the scope beyond the pylorus. • What is the differential diagnosis of this presentation? • What should be the next step in management? Differential: gastric outlet obstruction • Malignant – Pancreatic cancer with extension to stomach or duodenum – Primary distal gastric cancer – Gastric lymphoma – Primary duodenal adenoCa – Ampullary adenoCa • Benign – Acute PUD – Chronic PUD – Gastro-duodenal Crohn’s disease – Chronic Pancreatitis • • • Infectious: Gastric TB Structural: Gastric volvulus Bouveret's syndrome: – large gallstone migrating into duodenum via a cholecystoduodenal fistula, in the setting of cholecystitis – elderly women, ~70 years • • • Eosinophilic gastroenteritis Chronic granulomatous disease Gastroduodenal amyloidosis UGI • Mildly distended stomach with an abrupt transition to a narrowed caliber in the distal gastric antrum with the appearance of the overhanging edges. • A narrowed area extended from the antrum into the duodenal bulb an occluded the pylorus and was about 2.5 cm in length. There is ulceration of the inferior aspect of this area of narrowing and nodular distortion of the mucosal folds with a nodular impression on the inferior base of the duodenal bulb. • There is mild generalized narrowing of the descending duodenum with slight nodular thickening of the folds in the descending duodenum. • The findings are consistent with an infiltrating gastric carcinoma invading the duodenal bulb. Hospital Course • NGT, IVF, NPO • 5 days later: Distal gastrectomy with Bilroth II procedure • Pathology – Focal ulceration with acute and chronic inflammation, hyperplasia, fibrous scar formation and marked reactive atypia. – No evidence of dysplasia or neoplasia. No malignancy. – Benign resection margins. – Five lymph nodes, no tumor seen. – No definitive H. pylori organism. Fungal spores within the fibrinous exudate covering the ulcerated area. Hospital Course • NGT, IVF, NPO • 5 days later: Distal gastrectomy with Bilroth II procedure • Pathology – Focal ulceration with acute and chronic inflammation, hyperplasia, fibrous scar formation and marked reactive atypia. – No evidence of dysplasia or neoplasia. No malignancy. – Benign resection margins. – Five lymph nodes, no tumor seen. – No definitive H. pylori organism. Fungal spores within the fibrinous exudate covering the ulcerated area. Severe peptic ulcer disease complicated by gastric outlet obstruction Management of GOO (benign) • Medical/endoscopic management – Endoscopic dilation – Recurrent stenoses • Surgical management Lau et al. Gastrointest Endosc 1996;43:98-101. Kuwada et al. Gastrointest Endosc 1995;41:15-7. Management of GOO (benign) • Can recurrent GOO post dilation be prevented? • Which patients are more likely to develop recurrent GOO? Surgery 76% 78% (93%) 45% (64%) 76% successful dilation 36% recurrence at 2 years Median f/u: 24 (16-40) months 6% perforation rate Lam et al. Gastrointest Endosc 2004;60:229-33. Surgery 76% 78% (93%) 45% (64%) 76% successful dilation 36% recurrence at 2 years Median f/u: 24 (16-40) months 6% perforation rate Lam et al. Gastrointest Endosc 2004;60:229-33. Management of GOO (benign) • Repeat endoscopic dilations may be needed & can be successful. • Testing and eradication of H. pylori is an important component of the treatment algorithm. Cherian et al. Long-term follow-up of patients with gastric outlet obstruction related to peptic ulcer disease treated with endoscopic balloon dilatation and drug therapy. Gastrointest Endosc 2007;66:491-7. • Small observational study – 23 consecutive referred patients with GOO 2/2 PUD between 1995-2006 in UK • Endoscopically confirmed GOO: food in stomach, unable to pass 9mm endoscope beyond obstruction – Evaluation for etiology • • • • • • H. pylori (52%): rapid urease test or UBT & HP serology ASA & NSAIDs use (13%) & 9% with HP +ASA/NSAIDs Serum gastrin level Stop smoking Biopsies neg for malignancy Idiopathic (26%) – PPI use in all patients +/- Zantac – TTS balloon dilation to 15mm Average age 71 (43-94) 43% male Symptoms 78% abdominal pain 74% vomiting 34% weight loss 9% UGIB Location of GOO 61% pyloric stenosis 26% duodenal stenosis 13% both # dilations needed 2 (range 0-8) 28% 1 dilation 72% 2-8 dilations Median length of f/u 43 (5-90) months Remission rate 100% Remission was defined as the absence of symptoms in combination with endoscopic evidence of a patent gastric outlet and healing of PUD. Cherian et al. Gastrointest Endosc 2007;66:491-7. Management of GOO (benign) • Medical management – Endoscopic dilation – PPI maintenance – H. pylori eradication – Stop NSAIDs • Surgical management Cherian et al. Gastrointest Endosc 2007;66:491-7. Lam et al. Gastrointest Endosc 2004;60:229-33. ASGE guidelines: The role of endoscopy in the management of patients with PUD …. returning to our patient • 41 day hospitalization – MRSA bacteremia – Aspiration pneumonia – C.difficile colitis