The Role of the Nurse Practitioner in Primary Care pain Triage
advertisement

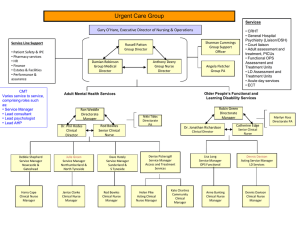
The Role of the Nurse Practitioner in Primary Care Pain Triage & Management Objectives Define and apply models of care that can assist with triaging pain management patients. Understand how the biopsychosocial approach can impact pain management. Appreciate the role of the Nurse Practitioner with pain management in primary care and multidisciplinary care settings. Health Care Reform Focus on collaborative teams, care coordination, cost reduction, quality, and patient centeredness. Accountable Care Organizations (ACO’s), Patient Centered Medical Homes (PCMH), Transitional Care Management (TCM). These models focus upon primary care, coordination, accessibility, quality, and patient safety utilizing nurse practitioners and physician assistants. (Naylor, 2012, IOM 2011, Neilson, et al 2012) Nurse Practitioners Presence in healthcare grown 36% of non-metropolitan visits 2008-2009. (MMWR, 2012) Between 1995 and 2009, the number of Nurse Practitioners per primary care physician more than doubled from 0.23 to 0.48. 140,000 practicing NP’s in the US 2011.(www.aanp.org) NP Educational Benefits Health Promotion Patient Education Interdisciplinary Collaboration Quality Assurance Healthcare Design Research Greenfield S, Anderson H, Winickoff R, Morgan A, Komaroff A. Nurse‐protocol management of low back pain-Outcomes, patient satisfaction and efficiency of primary care. The Western Journal of Medicine. 1975; 123(5): 350-‐9. Garfin S, Kurz LT, Harlow SJ, Katz MM, Weisman M. Effectiveness of a nurse practitioner in screening patients in a spinal disorders clinic. Spine. 1988; 13(1): 121-‐3. Sarro A, Rampersaud YR, Lewis S. Nurse practitioner‐led surgical spine consultation clinic. Journal of Advanced Nursing. 2010; 66(12): 2671-6. Crosley L, Mueller L, Horstman P, Software assisted spine registered nurse care coordination and patient triage one organization’s approach. Journal of Neuroscience Nursing. 2009; 41 (4): 217-224. 95% agreement in diagnosis and management plan between NP’s and surgeons. Safely triaged red flags. Patient satisfaction exceeded 94%, superior in the NP group and higher patient satisfaction scores. Patient access improved. Only 26% of 177 patients desired to wait to see the surgeon NP’s demonstrate excellent care with other chronic diseases. HTN study decreased blood pressure 44%, decreased incidence end organ damage. (Hill et al, 2003) DM: study of planned chronic care visits by Kaiser Permanente participants led by a nurse educator had significantly lower glycated hemoglobin levels and lower use of hospitals than controls. (Sadur et all, 1999) Massachusetts RAND study (2009) Nurse Practitioners care for diagnoses at a lower cost than physicians while maintaining quality and patient satisfaction. They note that NPs provide more disease prevention counseling, health education, and health promotion activities than physicians, which can lead to down stream health care savings. 2009 IOM Report on Nursing Nursing represents the largest sector of health professionals more than 3 million USA. Shift toward team-based care. Affordable, quality care, patient centered, evidence based, outcome based. Chronic Disease SelfManagement Chronic illness is a leading cause of death and disability globally. (WHO, 2011) Nearly 1 in 2 US adults lives with chronic illness such as diabetes, heart disease, or arthritis and the prevalence is rising. (National Center for Chronic Disease Prevention and Health Promotion, 2009) Pain (National Center for Health Statistics Report: Health, United States, 2006, Special Feature on Pain) Chronic Pain Back pain is the most common form of chronic pain at 27% Neck pain accounts for 15% Headache and migraine 15% Facial pain 4% (National Center for Health Statistics Report: Health, United States, 2006, Special Feature on Pain) Patient Access Patient Triage How do we get pain patients to the right provider at the right time? Fairview health system (2013) used risk stratification using the Keel STarT tool. R/O red flags Agency for Healthcare Research and Quality (AHRQ) guideline. The Keele STarT Back Screening Tool ! " #$%#$&'( ) * +, ', " - '!" #$% &% ' ( ( ) #', #. %'/* +0'0- 12* $1- ', * ', " - '3* 44* 5 #$&'6+- 1, #* $17' ' ' ' ' * +#" , - ( ( % . , - ( ( % 8' 9' 9' : /') ( . %'2( #$'" ( 1'#/ - ( " 0% 01' 2% 3 4% !( , 5#6'( , '1* ; - ', #; - '#$', " - '4( 1, '<'5 - - %1' !' !' <' ='" ( >- '" ( ? '2( #$'#$', " - '#718!0( - '* 0'2( 9) '( , '1* ; - ', #; - '#$', " - '4( 1, '<'5 - - %1' !' !' @' ='" ( >- '* $4/'' " !) ( 0% #71- $% 0+#$" 29( #') - . ( +1- '* 3'; /') ( . %'2( #$% !' !' A' =$', " - '4( 1, '<'5 - - %1B '='" ( >- '0- ( ##( 0% 3 1- ( % #!1' !4', " ( $'+1+( 4') - . ( +1- '* 3') ( . %' 2( #$' !' !' C' =, D 1'$* , '0- ( 44/'1( 3- '3* 0'( '2- 01* $'5 #," '( '. * $? #,#* $'4#%- '; #$- ', * ') - '2" /1#. ( 44/' ( . , #>- ' !' !' E' : 1- - 4+2, % $718, 7$#'" ( >- ') - - $'&* #$&', " 0* +&" '; /'; #$? '( '4* , '* 3', " - ', #; - ' !' !' F' ='3- - 4', " ( , '3 4% ; " 9) % / " +2% +#% $( - - +; !( '( $? '+$<#% 2( =( - % , 1+2, % $1% , ( $% " 24% ; ( $$( - ' !' !' G' =$'&- $- 0( 4'='" ( >- '21$% ( 2>14( 0'( 44', " - ', " #$&1'='+1- ? ', * '- $H * /' !' !' I J''K>- 0( 44B '" * 5 '; 1$7( - #13 ( '" ( 1'/* +0') ( . %'2( #$') - - $'#$', " - '!" #$% &% ' ( ( ) #' L * , '( , '( 44' M4#&" , 4/' : * ? - 0( , - 4/' N- 0/'; +. " ' OP, 0- ; - 4/' !' !' !' !' !' 8' 8' 8' 9' 9' ? 1$" !% #91- ( % 5" !!% @6A% BBBBBBBBBBBBBBBBBB% % % C8; % C91- ( % 5DEF@6ABBBBBBBBBBBBBB% % Q 'R- - 4- 'S $#>- 01#,/'89T8GT8F''' U+$? - ? ') /'V0, " 0#,#1'W- 1- ( 0. " 'S R Low to medium risk Reassurance. Self-management: activity modification, ice, heat, appropriate medication use, sleep. Stay active! High Risk Send to non-surgical specialist. Results: 50 times LESS opioid prescriptions than PCP, 56% more appropriate imaging, better outcomes. (American College of Physicians/American Pain Society Low Back Pain Guideline Panel 2007) Opioid Risk ORT: opioid risk tool. 5 items, 1 minute to administer. Intended setting primary care. High degree of sensitivity and specificity for risk for opioid abuse. (Webster & Webster 2005) Contraindications to opioid prescribing History substance abuse or prior prescription drug misuse. Unsanctioned dose escalation. Non-adherence to other recommendation for pain therapy. Unwillingness or inability to comply with treatment plan. Social instability. Unwillingness to adjust at risk activities resulting in serious reinjury requiring additional opioids. (AHRQ Guideline for Chronic Pain) Pain Management ≠ Opioid Prescribing Surgery Injections · in the clinic · xray-guided Medications · · oral topical Passive Therapies · · · · some PT manipulation massage, acupuncture, reiki etc. corset Active Therapies · some PT · strategies · Teachers Diet, Exercise, Sleep, · aerobic · stretching · strengthening Self Image · · · · hobbies habits psychological health job (Agency for Healthcare Research and Quality Technical Brief – Multidisciplinary Pain Programs for Chronic NonCancer Pain Published online July 28, 2010 (Final—September 30, 2011) www.effectivehealthcare.ahrq.gov Biopsychosocial Model Heads of workers compensation authority (HWCA) accepted model for injury management. Proposes that biomedical explanations are often insufficient in fully explaining ill health, damage to the tissue body or structure. Individual’s pain perception differs according to psychosocial variables. Cognitive behavioral approach—A problem solving approach to facilitate achievement of defined goals by breaking tasks down into achievable steps. Identify unhelpful beliefs. Challenge unhelpful beliefs. Introduce more helpful ways to think about/manage barriers—problem solving approach. Equip for self-management—to apply problem solving approach independently. http://www.hwca.org.au Pain Catastrophizing ‘Sur L’eau, novelist (1875). “Migraine is atrocious torment, one of the worst in the world, weakening the nerves, driving one mad, scattering one’s thoughts to the wind and impairing memory. So terrible are these headaches that I can do nothing but lie on the couch and try to dull the pain by sniffing ether.” Pain Catastrophizing is defined as “an exaggerated negative mental set brought to bear during actual or anticipated painful experience”. Elements of: Rumination: “I can’t stop thinking about how much it hurts” Magnification: “I worry that something serious may happen” Helplessness: There is nothing I can do to reduce the intensity of my pain” http://sullivan-painresearch.mcgill.ca/ Scores above 30 70% remained unemployed. 70% described themselves as totally disabled. 66% met dx for moderate depression. (BDI-II) Higher risk for chronicity with higher levels of pain and emotional distress. Pain catastrophizing may be the result of trauma Major losses, severe accidents, abuse, PTSD. (Peterson & Moon,1999) Pain catastrophizers are unsuccessful in using cognitive attention diversion coping strategies to reduce pain. (Sullivan et al, 1997) Hyperalgesic State Increased sensory flow pain signals. Increased sensitivity to pain. (Melzack, 1990) Neuroimaging: prefrontal, parietal, anterior cingulate cortex, thalamus more activated. (Seminowicz & Davis, 2006) Interventions Importance of reducing pain catastrophizing is a key factor to successful interventions for chronic pain. (Spinhoven et al 2004, Sullivan et al, 2005) Multidisciplinary program 40% reduction in catasrophizing scores. (Jensen et al 2001) Education, activity resumption and instruction on selfmanagement skills characterize content in multidisciplinary pain programs. (Gatchel et al, 2007) Progressive Goal Attainment Program 10 week program with cognitive behavioral interventions to increase activity and minimize psychological barriers in work related injuries. 62% return to work (RTW) rate in those absent > 6 months. 78% RTW rate for those absent 3 to 6 months. Reductions in catastrophizing were related to an increased RTW. (Sullivan & Stanish, 2003) Example: CLBP “medical symptom stress cycle”. Anxiety can lead to behavioral changes that exacerbate the pain the patient experiences. Treatment could include biofeedback and relaxation techniques. Goal is to reduce the anxiety associated with the pain. (Gatchal, et al, Spine J. 2008 ; 8(1): 40–44. doi:10.1016/j.spinee.2007.10.007) Case Study One 35 year old male, seen 2010 specific complaints, LE sciatica since 2003. Received treatment in the military stabilized with physical therapy baseline by 2004. Worsening LE symptoms seen 2010. No significant medical co-morbidities. PFSH: mother alcohol and prescription abuse. Physical exam: Decreased dermatome left L-5, decreased heel walking right. Positive SLR right. Muscle atrophy right calf. Dx: MRI mod stenosis L-4-5, HNP with tear L5-S1. Treatment Counseling for PTSD. Physical therapy. Sleep cycle disturbance. Reaction to amitriptyline. Spinal epidural with 90% improvement of symptoms. Re-visit 2014 Circles all descriptors on pain questionnaire. Does not localize pain. Gained 40 lbs, BMI 40. No exercise. PTSD ongoing. Sleep better not working 3rd shift, but interrupted by pain. Physical exam: poor core strength, difficulty bridging, turning supine to prone, guarding, LROM significantly reduced. No new diagnostics. Treatment Counseled for nutrition and weight loss. Physical therapy: active modalities rather than passive. PTSD discussed relationship to chronic pain. Consider SNRI, neurontin, lyrica (previously negative response to Elavil). Case Study 2 50 year old female, chronic widespread pain since 2010, MVA 2009. PMHX: FMS, Sadness, depression, headaches seen by neurology, GERD, cholecystectomy. ROS: sleep cycle disturbance pain, new urinary incontinence. Previously had cognitive behavioral therapy for pain. DX: MRI 2012 mod spinal stenosis C5-6, severe foraminal narrowing, EMG 2010 EMG neg radic. Record Review Psychological counseling: relaxation techniques and CBT. “Hides in her home because she feels she is negatively judged as a stay at home mother.” “Chronic pain has become her whole world.” “Because she doesn’t bring a paycheck, she does not deserve pleasure.” R/O Red Flags Exam: Positive hoffman’s right, DTR’s increased lower extremity, positive clonus, increased RLE tone and difficulty tandem walking. New urinary incontinence. MRI cervical spine ordered. To be continued…. Nurse Practitioner in Primary Care Triage Utilize models of care to r/o red flags. Understand the Keele STarT method for triaging patients. Initial treatment: stay active, reassurance, physical therapy. Prescribe non-opioid medications as first line agents. Follow responsible opioid prescribing, review risk/benefits. Complex patients with psychosocial concerns refer to specialist. Nurse Practitioner in Multidisciplinary Pain Assist the primary care provider in neurological, musculoskeletal assessment. Order diagnostic imaging when needed. Recommend future treatments. Create a plan of care for complex patients that involves: Physical conditioning. Psychological counseling, CBT. Vocational Rehabilitation, social integration. Adjustment to disability. Medication adjustments. Workers compensation management. Surgical vs. conservative treatment.





![Slides [PowerPoint]](http://s2.studylib.net/store/data/005600327_1-9e9384bed45e687960e45f966cb28408-300x300.png)