BASIC HEMATOLOGY - VCU Massey Cancer Center
advertisement
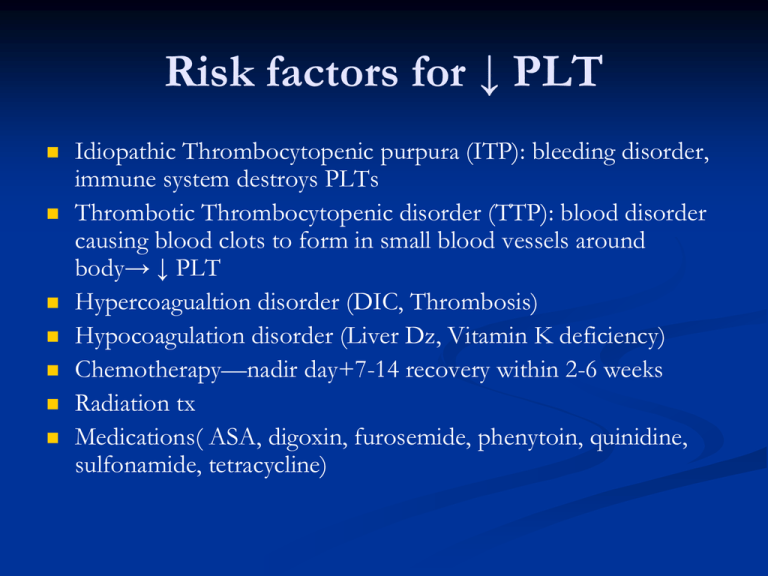
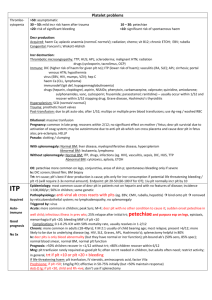
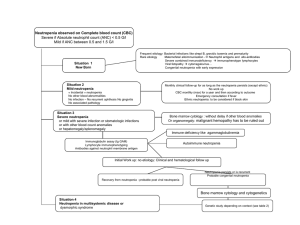
Risk factors for ↓ PLT Idiopathic Thrombocytopenic purpura (ITP): bleeding disorder, immune system destroys PLTs Thrombotic Thrombocytopenic disorder (TTP): blood disorder causing blood clots to form in small blood vessels around body→ ↓ PLT Hypercoagualtion disorder (DIC, Thrombosis) Hypocoagulation disorder (Liver Dz, Vitamin K deficiency) Chemotherapy—nadir day+7-14 recovery within 2-6 weeks Radiation tx Medications( ASA, digoxin, furosemide, phenytoin, quinidine, sulfonamide, tetracycline) Mgmt Thrombocytopenia PLT transfusions PLT<10,000 Colony stimulating factors, eg IL 11 (Neumega) Steroids Progesterone ↓ menstrual bleeding Nursing interventions Avoid tight BP cuffs when PLT<20,000 Avoid invasive procedures Avoid sharp objects/no barefoot Apply firm pressure to venipuncture sites for 5 minutes Treat nose bleeds with high fowler’s position-icepack Prevent constipation Encourage soft toothbrushes Why do we evaluate WBC? To assess body's response to significant bacterial insult, such as appendicitis, Pelvic inflammatory disease, pneumonia, pyelonephritis, and SEPSIS WHITE BLOOD CELLS Segmented Neutrophil (60%) Lymphocytes(30%) Monocytes(6%) Eosinophils(3%) Basophils(1%) SEGMENTED NEUTROPHIL 1ST line of defense Normal 50-70% Survive 1-2 DAYS LYMPHOCYTES 2 Types by appearance: Large granular and small Large granular are NK cells Small are T & B cell T cell mediated immunity B cell humoral immunity MONOCYTE 5-10 % Circulating WBCs When stimulated become Macrophages and dentritic cells in the tissue Clean up the debris EOSINOPHIL 1-5% Circulating WBCS Involved in parasitic infections Involved with mechanism associated with allergy and asthma ↑In case of w.w.w. BASOPHIL < 1% circulating WBCS Involved with allergic and inflammatory response Release histamines and cytokines Hematological Symptoms Hematological Symptoms Neutropenia—defined as ANC<1000/mm3 Anemia--↓RBC & Hgb Thrombocytopenia—low PLT <100,000 Leukopenia—decrease in WBC, below the lower limit Pancytopenia-an abnormal deficiency in all blood cells, RBC, WBC, & PLT; usually associated with bone marrow tumor or with aplastic anemia) Risk factors for febrile neutropenia Previous Hx Chemo/Type of chemo/prior radiation Tx Age>65/ female gender Poor nutritional status Advanced cancer and bone marrow involvement ↑LDH, ↓Hgb Leukemia/lymphoma/lung cancer Open wounds DM COPD Prevention of Neutropenia Growth stimulating factors activate production of bone marrow cells. It can be given prophylactically or therapeutically BMT give GCSF on day+4 of stem cell SCT GCSF-/filgrastim 5mcg/kg Pegfilgrastim--Neulasta 6mcg/kg Neutropenic Precautions Limit exposure of pts to infections Hand washing ↓spread Avoid crowds Avoid fresh fruits /vegetables/flowers Avoid caring for animals esp. cleaning excretes Avoid gardening Infections Mechanical barriers—skin, mucous membranes Chemical barriers-pH of tissues Inflammatory and immune responses Risks of Infections High risk Intermediate risk Low risk High Risk for infection Allogeneic BMT Acute Leukemia's GVHD tx ↑dose steroids Neutropenic lasting >10 days Break in skin/mucosal barrier Prolonged ABX or steroid use Poor nutrition Invasive procedure Poor personal hygiene Intermediate Risks for infections Autologous BMT Lymphoma/MM/CLL Neutropenic anticipated to last >7-10 days Low Risk for infections Standard Chemotherapy Neutropenia <7 days PT AND PTT PT (PROTIME) Test the extrinsic pathway PTT Tests the intrinsic pathway COUMADIN (WARFARIN) Affects the Vitamin K factors (II,VII,IX,X ) of which factor VII is the most labile Hemophilia is a factor VIII deficiency INR: Method for standardizing Protimes. It is a ration of tested results : control COAGULATION PRODUCTS Fresh Frozen Plasma Cryoprecipitate: Factor VIII, Fibrinogen Activated Products: Factor IX Chemistry Tests Liver Function Studies Renal Function Electrolytes—Na, K, Ca, Mg, Po4, Co2 LIVER FUNCTION Hepatocelluar Enzymes: AST (ASPARTATE AMINOTRANSFERASE) ALT (ALANINE AMINOTRANSFERASE) SGGT (very specific) LDH (Lactate Dehydrogenase) LIVER FUNCTION ALKALINE PHOSPHATASE-AP not specific to liver AP= LARGE COMPONENT IN BONE BILIRUBIN -2 TYPES DIRECT OR CONGUGATED AND INDIRECT OR UNCONGUGATED. AP / BILIRUBIN the first enzymes to rise with liver GVHD INDIRECT BILIRUBIN associated with hemolysis LDH Nearly every type of cancer, as well as many other diseases, can cause LDH levels to be ↑, cannot be used to dx a particular type of cancer. LDH levels can be used to monitor treatment of some cancers, including testicular cancer, Ewing's sarcoma, non-Hodgkin's lymphoma, and some types of leukemia Elevated LDH levels can be caused by a number of noncancerous conditions, including heart failure, hypothyroidism, anemia, and lung or liver disease. RENAL BUN (BLOOD UREA NITROGEN) Elevated with: Kidney dysfunction, Dehydration, excess protein in blood such as TPN, High protein diet, GI bleeding Creatinine: chemical waste is generated from muscle metabolism. Creatinine is produced from creatine, a molecule of major importance for energy production in muscles. Creatinine is transported through the bloodstream to the kidneys. The kidneys filter out most of the creatinine and dispose of it in the urine. CREATININE CONT. The ratio of BUN : creatinine determines renal dysfunction VS pre-renal dysfunction such as dehydration. CALCULATED CREAT. CLEARANCE: in ml/min---CRCL=(140-AGE) x ideal B.W./Scr. x 72 (x 0.85 for females) ELECTROLYTES SODIUM POTASSIUM CALCIUM PHOSPHORUS MAGNESIUM CO2 SODIUM/POTASSIUM SODIUM /POTASSIUM MEMBRANE PUMP CALCIUM/PHOSPHORUS DIRECT INTERACTION IF GIVEN CONCOMBINETLY: NaPO4 + CaCO3 = CALCIUM Calcium in plasma is bound to Albumin. If Albumin is low, you get a falsely low serum calcium. 2 ways to get a more accurate Calcium: IONIZED CALCIUM CORRECTED CALCIUM CORRECTED Calcium: [(4.0 – serum alb) x 0.8 ] + s Ca = corrected Ca MAGNESIUM Very important for Cardiac, Nervous and GI systems. Interacts with calcium and Potassium. Difficult to get a Normal serum level of Potassium if Mg is low. CO2 Gives a rough idea of pH and buffer system in blood Infections typically have low venous CO2 Bone marrow Biopsy-aspirate Used in Identi. metastatic Dz, esp hematological malignancies Assess iron stores Assess megaloblastic maturation, in Vit B12 and folate deficiencies or in MDS Assess fat atrophy, aplasia or fibrosis Other tests done in Hem/Onc Fractionated bilirubin—to differentiate cause of hyperbilirumia Stool guaiac--? bleeding Coombe’s test—direct/indirect Haptoglobin level—to detect hemolytic anemia Hgb electropheresis---- MICROBIOLOGY BACTERIA VIRUS FUNGAL/YEAST PROTOZOAN BACTERIA CATAGORIZED BY SHAPE AND STAINING PROPERTIES GRAM’S STAIN SHAPES ARE COCCI, RODS, AND SPIROCHETES BACTERIAL SHAPES COCCI RODS SPIROCHETES GRAM’S STAIN INTERACTS WITH THE BACTERIAL MEMBRANE AND STAINS IT EITHER BLUE OR RED BLUE IS GM (+) RED IS GM (-) GRAM POSITIVE COCCI: 1. STAPHALOCOCCUS EITHER COAGULASE (-) OR (+) COAG NEG=STAPH EPID. COAG POS= STAPH AUREUS 2. STREP, ENTEROCOCCUS RODS: BACILLUS, LISTERIA, CORYNEBACTERIA DIPTHERIA Staph aureus GRAM NEGATIVE COCCI: NEISSERIA, MORAXELLA, ACINETOBACTER RODS: E.COLI, PSEUDOMONAS, SHIGELLA, SALMONELLA, KLEBSIELLA, PROTEUS, ENTEROBACTER, VIBRIO Gram Negative rods FUNGUS MOLDS: ASPERGILLUS , MUCOR, YEAST AND YEASTLIKE: CANDIDA, TORULOPSIS, HISTOPLASMOSIS, CRYPTOCOCCUS, BLASTO. FUNGUS VIRUS CYTOMEGALOVIRUS EPSTEIN-BAR BK ADENOVIRUS INFLUENZA A & B PARAINFLUENZA RSV PNEUMOCYSTIS CARINII PREVIOUSLY CONSIDERED A PROTOZOAN BUT NOW IN FUNGUS CLASS References Demetri, G. (2001) Anemia and its functional consequences in cancer pts, current challenges in management & prospects for improving therapy. British Journal of Cancer,84,31-37 Dessypris, E, Erythropoiesis (1988). Lee G R, Foster J, Lukens J, Wintrobe M M, eds.Wintrobe’s clinical hematolology. Pa: Lippincott Williams & Williams 1998. 169-192. Ludwig H, & Strasser K.(2001) Symptomatology of anemia. Seminars in oncology, 28, 7-10 Means, R. (1999). The anemias of chronic disorders. Lee GR, Foerster J, Lukens J, Paraskeras F, Greer J P, Rodgers GM, eds. WIntrobe’s Clinical hematolgoy.10th ed, Pa. Lippincott Williams & Wilkin;1999:1011-1021 National Comprehensive Cancer Network (2007). Cancer and treatment related anemias, version 3.2007 The End Shortcut to DSC03990.lnk