Anti-TNF, Immunosuppression and
Renal Disease: Approaches in TB
Dr Heather Milburn
Consultant Respiratory Physician
Guy’s & St Thomas’ NHS Foundation Trust
READER IN Respiratory Medicine
KING’S College London
Relative risk of developing active TB
(Nice Guidelines, 2006/2011)
Clinical Condition
Relative Risk
Diabetes mellitus
Solid organ transplantation
2-4
20-74
Silicosis
30
Chronic renal failure/haemodialysis 10-25.3
Gastrectomy
Contact smear +ve TB
2.5
5-10
HIV
10
Anti-TNF therapy
Corticosteroids, MMF, tacrolimus,
ciclosporin, aza, mtx, rituximab…..
5
?
Difficulties in Management of TB & LTBI in Renal
Disease
• Risk: ethinic minorities inc risk both TB & CKD
• Screening: when? How? skin anergy; IGRA tests –
evaluation.
• Diagnosis: unusual presentations
• Treatment: timing; dosage; drug interactions.
Renal Disease – TB Risk
• Chronic Kidney Disease
- Acqu’d i/d state
- Functional abnorm N, T&B lympho,
monos, NK cells; vitamin D deficiency
- Risk 31.4 in China, ?UK
• Maintenance Haemodialysis
- Risk 10-25x (NICE 2006)
• Transplant
- Risk 100-400x (Europe & USA; ISC
?higher)
- NICE 2006 overall relative risk x37
Incidence of TB - CKD
• TB incidence UK 15/100,000; London 44.4/100,000
• Dialysis 1,187/100,000 (Moore et al 2002)
No. of
cases/100,000
1400
1200
1000
800
600
400
200
CAPD
Haemodialysis
Functioning
Transplant
Total
Transplants
General UK
Population
London
0
Palchaudhuri et al 2011
Uraemic Milieu
Intracellular Ca++
Zn deficiency
Malnutrition –
low albumin
Fe overload
Uraemic toxins –
guanidines, polyamines
neutrophil
Myeloperoxidase
O2 radicals
bacterial killing
bacterial virulence
Uraemic milieu
Renal replacement therapy
Vit D deficiency
C’ activation
IL1b
IL6
Monocyte/APC
Chronic inflammation
TNFa
IL12
costimulation
IL6/IL10 imbalance
T cell
IL6
TH1
differentiation
TH2
IL4
IFNg
Cellular immune
response
B cell
Humoral immune
response
Renal Disease – LTBI & Prophylaxis
• Who?
- All uraemic patients?
- Only those with particular risk?
• When?
- CKD?
- On dialysis?
- Pre-transplant?
- Post-transplant?
• How?
- TST?
- IGRA?
• What?
- 6/12 H
- 3/12 RH (drug interactions)
- 4-6/12 R (drug interactions)
Renal Disease – Method of Screening
• Pre-transplant
• TST – Anergy 30-50%
Drugs – pred, aza, 6-MCP, mtx,
cycloph, mycophenolate, ciclosp,
tacrolimus
• Interferon-g tests – evaluation?
• CXR
Bumbacea et al. Eur Respir J 2012;40:990-1013
IGRAs in Immunosuppression
CKD
Systematic Review of 30 studies (47):
• Predominantly HD
• Countries with low-mod TB prevalence
• 9 compared IGRAs with TST, 17 TST only, 4 other tests.
• cf +ve TST, +ve ELISA more strongly assoc with radiol evidence past TB (OR
4.29, CI 1.83-10.3, p=0.001) and contact with aTB (OR 3.36, CI 1.61-7.01,
p=0.001)
• cf –ve TST, -ve ELISA more strongly assoc with BCG (OR 0.30, CI 0.14-0.63,
p=0.002)
• Insufficient data to compare ELISPOT with TST or ELISA
• ELISA more strongly assoc with risk factors for LTBI in CKD than TST
(Rogerson et al., Am J Kidney Dis 2013)
Study design
Data set consisting of
• Mendel Mantoux skin-test
• T-SPOT.TB
• QuantiFERON-TB Gold In-Tube
Clinical data
• TB risk factors
• Level of immunosuppression
TBNET
Percentage of positive results
Similar percentages of
positive test results in all assays
CRF
40
30
26.3%
26.7%
27.1%
all
<5 years of dialysis
>5 years of dialysis
20
10
0
TBNET
Patients with
chronic renal
failure
Percentage of positive results
Similar percentages of
positive test results in all assays
CRF
40
30
all
<5 years of dialysis
>5 years of dialysis
20
10
TBNET
0
Patients with
chronic renal
failure
Agreement between the tests
K=0.3
2
neg
pos
K=0.2
8
neg
CRF
pos
neg
158
(60.3%)
35
(13.4%)
neg
155
(59.2%)
38
(14.5%)
pos
34 (13.0%)
35
(13.4%)
pos
36 (13.7%)
33
(12.6%)
K=0.5
2
neg
pos
TBNET
neg
167
(63.7%)
25 (9.5%)
pos
24 (9.2%)
46
(17.6%)
CRF
No association with TB exposure
crude
TBNET
age, sex, duration of
dialysis
OR
95% CI
OR
95% CI
1.2
0.6-2.2
1.1
0.6-2.3
1.3
0.7-2.3
1.2
0.6-2.3
1.2
0.6-2.5
1.3
0.6-2.6
BTS Recommendations 2010
• Screening for LTBI - Method:
Use IGRA with or without TST
• Who to screen:
Pre-transplant
Contacts
• Chemoprophylaxis:
6H if post transplant
3RH if pre transplant
4R if pre transplant
Drug Recommendations: Chemoprophylaxis
• H & R - normal doses in CKD.
• Long term use of isoniazid is not recommended.
• No evidence for prolonged chemoprophylaxis with
any of above.
• No evidence for lower doses - lower peak levels and
drug resistance.
Guidelines for management of TB & LTBI in CKD;Thorax 2010:65:559-70
Active TB
Routine Assessment:
• History – prev TB, Rx & time, recent contact
• Chronic cough, wt loss, sweats – CXR
• Sputum, ind sputum, FOB, EBUS
Presentation:
• Not always classic
• Extra pulmonary common – 30-50%; peritoneal
Investigation:
• Active TB suspected –fluid or tissue for culture & sensitivity testing;
histology
• Active pulm disease – isolate in negative pressure room
• Notify
• INVOLVE CHEST PHYSICIANS
40yr old white M
Peritoneal dialysis 1yr
Abdom pain, Cloudy dialysate, No cough
T 38, WCC 5.4, N 4.4, Ly 0.8, CXR unremarkable
Blood cultures –ve, MC&S of dialysate –ve
From Latvia, UK 1yr
Antibiotics 1/52
No improvement
Further specimens neg
Change antibiotics
No improvement
Abdo US – nodes and omental thickening
Biopsy – granulomata, no AFB seen, grew H resistant TB
Pharmacokinetics & Toxicity of first-line drugs in
CKD
• H: metabolised by liver
- neurotoxicity – give pyridoxine
- neuropsychiatric disturbance
- ototoxicity – rare and can occur in CKD
• R: metabolised by liver
- no signif increase tox
• Z: metabolised by liver
- uric acid retention – gout
• E: 80% excreted unchanged by kidneys
- ocular toxicity dose dependent
- increased efficacy normal dose less often
Treatment aTB
47yr old Black African, HD, sm+ PTB, dry wt 68kg
Management?
Not on open HD unit!
Medication:
Rifater 6 daily
Ethambutol 600mg daily
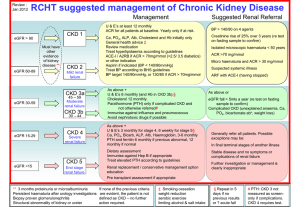
Renal Disease - Treatment
CKD Stage 1 normal function but structural abnormality
CKD Stage 2 Cr Cl 60-90mls/min; Stage 3 30-60mls/min;
Stage 4 15-30mls.min; Stage 5 <15mls/min.
• Dose
Do not reduce dose as leads to lower peak dose
- Iso, Rif, – normal doses; Give piridoxine
- PZA & E – normal doses for stages 1-3;
increased dose intervals in stages 4 & 5 CKD
and HD;
- Moxi – normal dose stages 1-3 & Tx; not suitable
3x/wk
Renal Disease - Treatment
• When?
- H & R daily or 3x/wk
- E & Z daily for stages 1-3, otherwise
3x/week; E peak & trough levels
- Z signif removed by dialysis
- 4-6hrs before haemodialysis or
immediately after
- Moxi daily 1-3 & Tx; not 3x/week
Peritoneal dialysis? – careful monitoring
Renal Disease - Treatment
• Duration
Standard 6/12 for fully sensitive
CNS – 1 year
• Immunosuppression
Rif interferes with most regimens.
Monitor levels
Double steroid doses
MMF, ciclosporin and tacrolimus dosages
adjustment
need
Drug recommendations…active TB
• Standard chemotherapy agents, standard
duration as per NICE guidelines
• Monitor peak & trough levels - Ethambutol and
aminoglycosides. Concern about over-and underdosing.
• CKD stage 4-5 or haemodialysis – increase dosing
intervals to 3 times weekly for E, Z &
aminoglycosides. Reduces risk of drug
accumulation and toxicity
BTS Guidelines Thorax 2010
TB in CKD - Summary
•
•
•
•
•
•
•
•
•
High risk of TB – partic non-UK born, EMGs
Screen pre-tx & those at particular risk
Usual chemoprophylaxis
aTB – extra-pulmonary, low index of suspicion
Medication – do not reduce dose but inc dosing interval (E, Z,
aminoglycosides Stages 4-5 & haemodialysis)
Increased risk drug resistance
Drug interactions - Rif
Drug monitoring
VIGILANCE!
»
BTS Guidelines Thorax 2010
Renal Impairment & TB:
Unanswered Questions
What are the rates of TB and LTBI in countries with
low background rate?
• What is the increased risk?
How do the IgRA tests perform?
When to screen for LTBI?
Which patients should receive chemoprophylaxis?
Dosages, dose intervals, timing on HD?
Pharmacokinetics for patients on peritoneal dialysis?