Evaluating a CBT Hearing Voices Group
advertisement
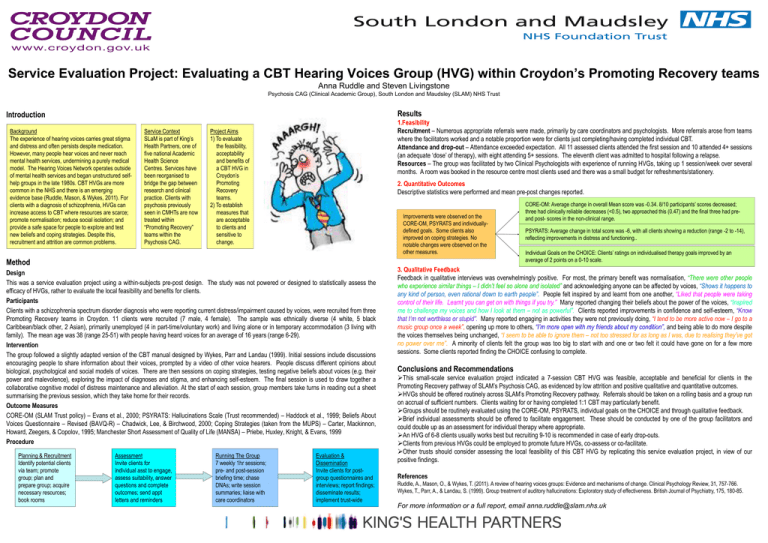
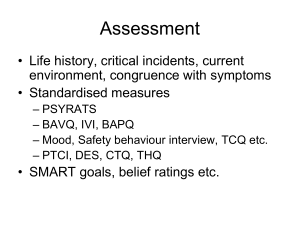
Service Evaluation Project: Evaluating a CBT Hearing Voices Group (HVG) within Croydon’s Promoting Recovery teams Anna Ruddle and Steven Livingstone Psychosis CAG (Clinical Academic Group), South London and Maudsley (SLAM) NHS Trust Results Introduction Background The experience of hearing voices carries great stigma and distress and often persists despite medication. However, many people hear voices and never reach mental health services, undermining a purely medical model. The Hearing Voices Network operates outside of mental health services and began unstructured selfhelp groups in the late 1980s. CBT HVGs are more common in the NHS and there is an emerging evidence base (Ruddle, Mason, & Wykes, 2011). For clients with a diagnosis of schizophrenia, HVGs can increase access to CBT where resources are scarce; promote normalisation; reduce social isolation; and provide a safe space for people to explore and test new beliefs and coping strategies. Despite this, recruitment and attrition are common problems. Service Context SLaM is part of King’s Health Partners, one of five national Academic Health Science Centres. Services have been reorganised to bridge the gap between research and clinical practice. Clients with psychosis previously seen in CMHTs are now treated within “Promoting Recovery” teams within the Psychosis CAG. 1.Feasibility Recruitment – Numerous appropriate referrals were made, primarily by care coordinators and psychologists. More referrals arose from teams where the facilitators worked and a notable proportion were for clients just completing/having completed individual CBT. Attendance and drop-out – Attendance exceeded expectation. All 11 assessed clients attended the first session and 10 attended 4+ sessions (an adequate ‘dose’ of therapy), with eight attending 5+ sessions. The eleventh client was admitted to hospital following a relapse. Resources – The group was facilitated by two Clinical Psychologists with experience of running HVGs, taking up 1 session/week over several months. A room was booked in the resource centre most clients used and there was a small budget for refreshments/stationery. Project Aims 1) To evaluate the feasibility, acceptability and benefits of a CBT HVG in Croydon’s Promoting Recovery teams. 2) To establish measures that are acceptable to clients and sensitive to change. 2. Quantitative Outcomes Descriptive statistics were performed and mean pre-post changes reported. Improvements were observed on the CORE-OM, PSYRATS and individuallydefined goals. Some clients also improved on coping strategies. No notable changes were observed on the other measures. Method Design This was a service evaluation project using a within-subjects pre-post design. The study was not powered or designed to statistically assess the efficacy of HVGs, rather to evaluate the local feasibility and benefits for clients. Participants Clients with a schizophrenia spectrum disorder diagnosis who were reporting current distress/impairment caused by voices, were recruited from three Promoting Recovery teams in Croydon. 11 clients were recruited (7 male, 4 female). The sample was ethnically diverse (4 white, 5 black Caribbean/black other, 2 Asian), primarily unemployed (4 in part-time/voluntary work) and living alone or in temporary accommodation (3 living with family). The mean age was 38 (range 25-51) with people having heard voices for an average of 16 years (range 6-29). Intervention The group followed a slightly adapted version of the CBT manual designed by Wykes, Parr and Landau (1999). Initial sessions include discussions encouraging people to share information about their voices, prompted by a video of other voice hearers. People discuss different opinions about biological, psychological and social models of voices. There are then sessions on coping strategies, testing negative beliefs about voices (e.g. their power and malevolence), exploring the impact of diagnoses and stigma, and enhancing self-esteem. The final session is used to draw together a collaborative cognitive model of distress maintenance and alleviation. At the start of each session, group members take turns in reading out a sheet summarising the previous session, which they take home for their records. Outcome Measures CORE-OM (SLAM Trust policy) – Evans et al., 2000; PSYRATS: Hallucinations Scale (Trust recommended) – Haddock et al., 1999; Beliefs About Voices Questionnaire – Revised (BAVQ-R) – Chadwick, Lee, & Birchwood, 2000; Coping Strategies (taken from the MUPS) – Carter, Mackinnon, Howard, Zeegers, & Copolov, 1995; Manchester Short Assessment of Quality of Life (MANSA) – Priebe, Huxley, Knight, & Evans, 1999 Procedure Planning & Recruitment Identify potential clients via team; promote group; plan and prepare group; acquire necessary resources; book rooms Assessment Invite clients for individual asst to engage, assess suitability, answer questions and complete outcomes; send appt letters and reminders Running The Group 7 weekly 1hr sessions; pre- and post-session briefing time; chase DNAs; write session summaries; liaise with care coordinators Evaluation & Dissemination Invite clients for postgroup questionnaires and interviews; report findings; disseminate results; implement trust-wide CORE-OM: Average change in overall Mean score was -0.34. 8/10 participants’ scores decreased; three had clinically reliable decreases (<0.5), two approached this (0.47) and the final three had preand post- scores in the non-clinical range. PSYRATS: Average change in total score was -6, with all clients showing a reduction (range -2 to -14), reflecting improvements in distress and functioning.. Individual Goals on the CHOICE: Clients’ ratings on individualised therapy goals improved by an average of 2 points on a 0-10 scale. 3. Qualitative Feedback Feedback in qualitative interviews was overwhelmingly positive. For most, the primary benefit was normalisation, “There were other people who experience similar things – I didn’t feel so alone and isolated” and acknowledging anyone can be affected by voices, “Shows it happens to any kind of person, even rational down to earth people”. People felt inspired by and learnt from one another, “Liked that people were taking control of their life. Learnt you can get on with things if you try.” Many reported changing their beliefs about the power of the voices, “Inspired me to challenge my voices and how I look at them – not as powerful”. Clients reported improvements in confidence and self-esteem, “Know that I’m not worthless or stupid”. Many reported engaging in activities they were not previously doing, “I tend to be more active now – I go to a music group once a week”, opening up more to others, “I’m more open with my friends about my condition”, and being able to do more despite the voices themselves being unchanged, “I seem to be able to ignore them – not too stressed for as long as I was, due to realising they’ve got no power over me”. A minority of clients felt the group was too big to start with and one or two felt it could have gone on for a few more sessions. Some clients reported finding the CHOICE confusing to complete. Conclusions and Recommendations This small-scale service evaluation project indicated a 7-session CBT HVG was feasible, acceptable and beneficial for clients in the Promoting Recovery pathway of SLAM’s Psychosis CAG, as evidenced by low attrition and positive qualitative and quantitative outcomes. HVGs should be offered routinely across SLAM’s Promoting Recovery pathway. Referrals should be taken on a rolling basis and a group run on accrual of sufficient numbers. Clients waiting for or having completed 1:1 CBT may particularly benefit. Groups should be routinely evaluated using the CORE-OM, PSYRATS, individual goals on the CHOICE and through qualitative feedback. Brief individual assessments should be offered to facilitate engagement. These should be conducted by one of the group facilitators and could double up as an assessment for individual therapy where appropriate. An HVG of 6-8 clients usually works best but recruiting 9-10 is recommended in case of early drop-outs. Clients from previous HVGs could be employed to promote future HVGs, co-assess or co-facilitate. Other trusts should consider assessing the local feasibility of this CBT HVG by replicating this service evaluation project, in view of our positive findings. References Ruddle, A., Mason, O., & Wykes, T. (2011). A review of hearing voices groups: Evidence and mechanisms of change. Clinical Psychology Review, 31, 757-766. Wykes, T., Parr, A., & Landau, S. (1999). Group treatment of auditory hallucinations: Exploratory study of effectiveness. British Journal of Psychiatry, 175, 180-85. For more information or a full report, email anna.ruddle@slam.nhs.uk